PCSFIOL implantation with sutures in correction of aphakia after combined PPV and lensectomy is gradually becoming popular especially when the capsular support, be it anterior or posterior, is inadequate or absent. Relative Spectacle Magnification (RSM) in simple terms refers to how images increase in size on the retina when extraocular methods are utilized in correction of aphakia. RSM is 1.00, 1.10, and 1.30 when aphakia is corrected with PCIOL, contact lens and aphakic glasses respectively. In other words, an image size magnifies by 10% and 30% with the use of contact lens and aphakic glasses respectively instead of a normal PCIOL. This may give way to aniseikonia and difficulty in fusion. Their worst effect is the miscalculation of distances and bumping into objects. These types of glasses are also associated with complications like pincushion distortions, reduced visual field and jack-in-the-box phenomenon apart from being heavy to wear [1]. Contact lens wear may be associated with eye lid, corneal and conjunctival complications. On the eyelid, blepharoptosis may occur. According to a research conducted by Robertson DM et al., the most feared complication of contact lens wear is Pseudomonas Aeruginosa Keratitis (PAK) whose treatment is very difficult [2]. Another study published by Weed NC et al., established that 87.5% of patients affected by PAK will have reduction in Best Corrected Visual Acuity (BCVA) even after best treatment modalities are applied [3]. Superior limbic keratconjunctivitis and giant papillary conjunctivitis may also occur with their use.
Anterior chamber intraocular lens implantation may bring about corneal endothelial decompensation, glaucoma and cystoid macular oedema [4]. Use of tissue fibrin glue in placing PCIOL has just started gaining grounds in ophthalmology. Therefore, literature on it is equally very little. In the American Academy of Ophthalmology 2012 Spotlight on Cataract Surgery Session, only 7.2% of the audience agreed to use this method in case they were faced with deficient capsular support [5]. According to Agarwal A et al., tissue glue has two main components which naturally occur in blood: fibrinogen and thrombin. They are kept separate until it is time for their use because when the latter comes into contact with the former it promotes rapid conversion of fibrinogen to fibrin producing local fibrin clot. The thrombin in the glue also interacts with endogenous fibrinogen in the sclera bringing about accelerated fibrotic healing which in turn helps to hold the haptics in place after the glue has degraded. Tissue glue, however, contains human products making viral transmission from one patient to another a risk factor [6]. Although, PCSFIOL with sutures may be associated with such complications as postoperative inflammation, erosions over the sutures, induced astigmatism and suture breakage in years after surgery [6], its advantages far outweigh its complication profile. To date, multiple published case series have shown favourable results when PCSFIOL is implanted with sutures after cataract surgery in which there is posterior capsular rupture. The purpose of our study was to evaluate the outcomes and complication profile of a large series of patients who underwent secondary PCSFIOL implantation with sutures after combined PPV and lensectomy.
Materials and Methods
The medical records of patients who underwent PCSFIOL implantation after combined PPV and lensectomy in our hospital were retrospectively analyzed. The study reviewed the records of consecutive patients who underwent the surgery mentioned above between 2010 and 2014 and had a minimum follow up of three months. Three experienced surgeons performed all the surgeries. Institutional ethical approval was required for this research and in a wider dimension, the tenets of Declaration of Helsinski utilized in an attempt to respect human rights of the participants. In addition to general demographic data, information on baseline preoperative visual acuity, indication for surgery, postoperative complications, latest Best Corrected Visual Acuity (BCVA) and indication for any subsequent surgical procedures was collected and analyzed. Out of the 160 patients whose medical records were reviewed, 12 were excluded from the study because they were followed up for less than three months or lost to follow up.
Aurolens single piece intraocular nonfoldable lenses (Aurolab, No.1, Sivagangai Main Road, Veerapanjan, Madurai-625 020, India) were used for all PCSFIOL implantations. These were single piece Polymethylmethacrylate (PMMA) lenses with eyelets, optic diameter of 6.5 mm and overall length of 13.0 mm. The secondary implantation of Intraocular Lens (IOL) was planned when the vitreo-retinal disease had subsided and remained stable for a minimum of eight weeks. IOL power was calculated using the SRK/T (Sanders-Retzlaff-Kraff theoretical) formula.
A scleral tunnel incision at 12 o’ clock position with a width of 6-7 mm was made in all cases. A double-armed 9-0 polypropylene suture (6092 PP, Aurolab, Madurai, India) with straight needles was used. One straight needle was passed perpendicularly through the full thickness sclera, 1.5 mm behind the limbus at 3 o’ clock position in a direction parallel to the iris, and was retrieved in the hollow of 26 gauge needles on the opposite side. The stretched suture was pulled out of the eye through a previously made sclerocorneal tunnel. The suture was then cut in the middle and the two suture ends were passed through the corresponding eyelet of the PCSFIOL and tied. The lens was inserted into the ciliary sulcus, and the sutures pulled to secure the IOL. The corneoscleral wound was secured with interrupted 9-0 nylon sutures. The needle ends of the 9-0 prolene suture were then bent and a Z-shaped intrascleral passes with at least five indentations were made to secure the IOL. The suture was cut without making any knots and covered by the conjunctiva [7].
The Snellen BCVA was converted into logarithm of the minimum angle of resolution (logMAR) units for statistical analysis. Patients whose visual acuities were hand motion were assigned the equivalence of 1.7 logMAR units.
Statistical Analysis
The chi- square χ2 test is used for determining relationships between categorical variables, and the paired t-test was used for normally distributed variables. All tests were considered to be statistically significant if the p-value was 0.05 or less. We conducted the Chi square test and paired t-test using SPSS and Graph Pad softwares respectively.
Results
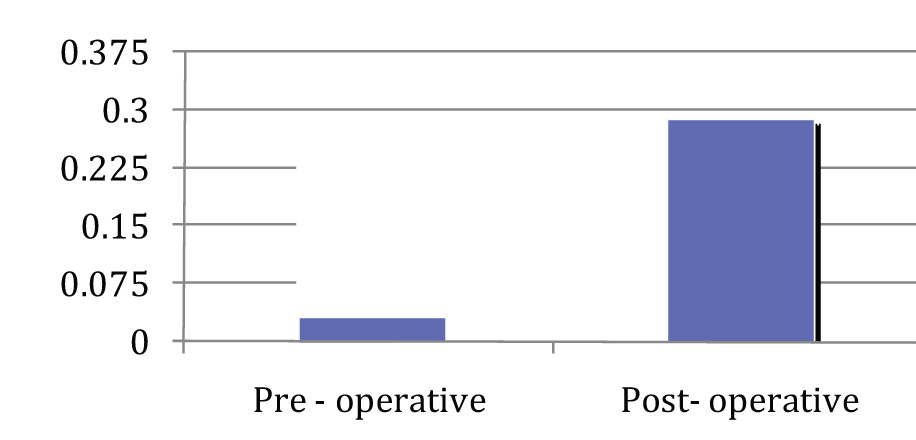
[Table/Fig-1] shows summary of visual outcome. BCVA did not change after PPV and the final BCVA after placement of PCSFIOL, but individuals had better visual acuities than before its implantation but the percentages did not change. The mean difference between final postoperative and preoperative visual acuity was 1.1±0.1 log MAR units which was statistically significant (p=0.001). This is shown in the graph pad below with its corresponding [Table/Fig-2,3].
Showing best corrected visual acuity after PCSFIOL.
| Sl No. | BCVA quality | After PCSFIOLnumber | Implantationpercentage |
|---|
| 1 | Maintenance | 4 | 2.70 |
| 2 | Worsening | 3 | 2.02 |
| 3 | Improvement | 141 | 95.27 |
| Total | 148 | 100 |
Mean difference between final postoperative and preoperative visual acuity.
| Preoperative | Postoperative | p-value |
|---|
| 0.030±0.078 | 0.293±0.287 | 0.0001 (***) |
Graph showing preoperative and postoperative visual acquity.
The underlying vitreoretinal diseases for which PPV was performed were retinal detachment (n=88 eyes; 59.46%); endophthalmitis (n=27 eyes; 18.24%); vitreous haemorrhage (n=18 eyes; 12.16%); dropped IOL (n=7 eyes; 4.73%); intraocular foreign body (n=6 eyes; 4.05%); dropped nucleus (n=1 eye; 0.68%) and non-settling panuveitis (n=1; 0.68%). In all 84 eyes (56.76%) had PPV as a result of traumatic, and 64 eyes (43.24%) non traumatic causes.
Out of the total number, the major indications for PCSFIOL were planned lensectomy (n=137 eyes; 92.57%); dropped IOL into vitreous (n=10 eyes; 6.76%) and dropped nucleus (n=1 eye; 0.68%). Those in whom planned lensectomy was performed were patients who had developed cataract of diverse aetiologies together with vitreoretinal disease prior to the PPV. Since the cataractous lenses were not allowing enough fundus view for appropriate PPV, lensectomy was performed. Some patients had also lost the integrity of their zonular fibres.
The mean preoperative BCVA was 1.7±0.60 logMAR units, which depended on the underlying vitreoretinal disease with which they reported for the first time. [Table/Fig-1] presents a summary of the visual outcome. In all 95.27% of patients had improvement, 2.70% unchanged and 2.02% worsening of their final postoperative visual acuity compared to preoperative measurement. The mean difference between final postoperative and preoperative visual acuity was 1.1 ± 0.1 logMAR units which was statistically significant (p=0.0001).
Overall 32 of 148 eyes (21.62%) developed postoperative complications from PCSFIOL as shown in [Table/Fig-3].
The most common complication was ERM formation (10 eyes; 31.25%) but did not lead to any visual impairment. This was corrected with secondary surgery in which epiretinal membrane peeling was performed with the use of trypan blue dye. Five eyes (15.63%) developed recurrent retinal detachment all of which had associated proliferative vitreoretinopathy. Two of them had worsening of their visual acuity. There were four (12.50%) recorded cases of dislocated PCSFIOL. This complication happened because the 10-0 Polypropylene Sutures (PPS) used in securing the IOLs got eroded and torn after few months. When these eyes were re-operated upon, we utilized 9-0 PPS and never again had similar complications till last follow up. The other complications which were IOL capture, uveitis, postoperative endophthalmitis, ocular hypertension, hyphaema and choroidal haemorrhage came to our setup with traumatic eye injuries. We strongly believe that these other complications from PCSFIOL were attributable to the primary traumatic injury with which the patients initially presented to us in the hospital. All eyes, eight weeks after PPV, whether trauma-associated or not were fit enough to undergo PCSFIOL surgery.
Out of 32 eyes which were re-treated due to complications after PCSFIOL, 26 (81.24%) and 6 (18.76%) had surgical and medical interventions respectively as shown in [Table/Fig-4]. Secondary implantation of PCSFIOL was made eight weeks after the first surgery in the eye. In all 141 (95.27%), 4 (2.70%) and 3 eyes (2.02%) had improvement, maintenance and worsening of their reporting visual acuities respectively at the latest follow up.
PCSFIOL complications and treatment.
| Sl No. | Complication | Number | Percentage | Treatment |
|---|
| 1 | Epiretinal Membrane (ERM) formation | 10 | 31.25 | ERM Peeling |
| 2 | Recurrent retinal detachment | 5 | 15.63 | Revitrectomy+Scleral buckling |
| 3 | Dislocated/Dropped PCSFIOL | 4 | 12.50 | Revitrectomy+Removal of old and replacement with new PCSFIOL+9-0 PPs |
| 4 | Proliferative vitreoretinopathy | 3 | 9.38 | Revitrectomy + Scleral buckling |
| 5 | Pupillary/IOL Capture | 2 | 6.25 | Cycloplegics + topical steroids + removal of old and replacement with new PCSFIOL |
| 6 | Uveitis | 2 | 6.25 | Cycloplegics + Topical steroids |
| 7 | Postoperative Endophthalmitis | 2 | 6.25 | Vitreous tap + Intravitreal antibiotics + Dexamethasone |
| 8 | Ocular Hypertension | 2 | 6.25 | Topical beta blocker + Carbonic anhydrase inhibitors |
| 9 | Hyphaema | 1 | 3.13 | Cycloplegic + Topical steroid |
| 10 | Choroidal Haemorrhage | 1 | 3.13 | Cycloplegic + Topical steroid |
| Total | 32 | 100 | |
Discussion
In the absence of capsular support or adequate zonular fibres in post vitrectomised aphakic eyes, PCSFIOL implantation is an effective surgical option compared to the use of other methods mentioned above in correction of aphakia. However, this procedure does have some potential complications and technical complexities, which can be minimized with good patient selection and surgical experience. The aim of this study was to assess the complication rate and visual outcome of PCSFIOL implantation with 9-0 PPS after combined PPV and lensectomy in a cohort of Indian patients who presented to our facility. In general, our results showed favourable outcomes with BCVA improved, maintained and worsened in 95.27%, 2.70% and 2.02% of eyes respectively. Outcomes of the present study were better than the studies reported in the literature [8,9].
In the present study, ERM formation was the most common complication. In terms of suture related complications, the hospital was using 10-0 PPS, many of which got eroded and torn giving way to subluxation or dislocation of IOL. We therefore stopped its use and started the use of 9-0 PPS which has not given us any complications. While elevated IOP requiring medical treatment occurred in only 6.25% of eyes in our study, it was more common in other case series. In a study published by Donaldson KE et al., comparing ACIOL and sutured PCSFIOL [10], the most common complication in both was increased intraocular pressure. This was defined as persistent ocular hypertension greater than 21 mmHg for more than 12 weeks requiring medical treatment. In their sutured PCSFIOL cohort follow up for a mean duration of 18 months, elevated IOP occurred in 42% of eyes. In another retrospective analysis of PCSFIOL by Krause L et al., 44% of eyes had transient increase in IOP as the most common postoperative complication [11]. Since some of our patients had silicone oil in their eyes during PPV with lensectomy in treating retinal problems, we performed 6 o’clock iridectomy to create an alternative pathway for aqueous humour to enter into the anterior chamber in case silicone oil blocked the pupil. This might have accounted for the lower rate of postoperative ocular hypertension in our study as opposed to other studies in which the surgeons did not perform any form of iridectomy.
Suture erosion incidence differs from one study to another. Solomon K et al., reported an incidence of 73% in their retrospective series of 30 eyes over 23 months whilst Uthoff D et al., reported an incidence of 17.9% in 624 patients during a one year follow up period [12,13]. In a longer term study published by Vote BJ et al., breakage of PPS was as high as 27% and the mean time from PCSFIOL implantation to suture breakage was 50 months [14]. In another study published by Luk ASW et al., suture breakage occurred in 1.9% over a mean follow up period of 73 months. All their patients with PCSFIOL implantation had 10-0, as 9-0 PPS was not routinely stocked in their hospital [15]. In our cohort we initially utilized only 10-0 PPS until end of 2010. Breakage rate was so high that we stopped its use and started with 9-0 PPS which has never given us any complications to date. The use of 9-0 may strongly reduce suture related complications because of its larger cross-sectional diameter and greater tensile strength compared to 10-0 PPS. Increased suture diameter size, however, may require large bore sclerostomies with the potential risk of leakage and endophthalmitis. The bigger suture is also technically more difficult to rotate and bury, and the knots if not buried may lead to erosion through the conjunctiva causing giant papillary conjunctivitis. Price MO et al., in a series on dislocated scleral sutured PCSFIOL, noted microscopic degradation and surface cracks in the 10-0 PPS remnants of explanted lenses [16]. Apart from being convinced that 9-0 is superior to 10-0 PPS in this procedure, they also recommend placement of IOL haptics into the ciliary body or ciliary sulcus with the aim to promoting scarring and permanent fixation of the IOL, a procedure which has been the normal practice in our hospital. This may help to enhance the long term stability of PCSFIOL. In future more studies are needed to substantiate the superiority of 9-0 over 10-0 PPS in management of post-vitrectomised aphakic eyes.
A 21.62% of eyes had to be re-operated or get more medical treatment as a result of complication in our case series. A 56.76% and 43.24% of PPV we performed were due to traumatic and non-traumatic causes respectively. It is therefore assumed that the complications which occurred in the traumatic cases were due to traumatic injury to the eye and not surgical incompetence. We strongly believe that these other complications from PCSFIOL were attributable to the primary traumatic injury with which the patients initially presented to us in the hospital. All eyes, eight weeks after PPV, whether trauma-associated or not, were fit enough to undergo PCSFIOL surgery.
Apart from ACIOLs, iris fixated IOLs are other modalities in aphakia correction in post-vitrectomised eyes when there is poor capsular support. Good visual outcomes have been reported in a large review by Wagoner MD et al., comparing secondary insertion of iris-fixated IOLs with ACIOLs and PCSFIOL [17]. Another study conducted in China in 72 eyes in a three-year period with the use of secondary anterior iris-fixated IOLs also reported good outcomes. Insertion of iris-fixated lens may be less technically demanding than PCSFIOL implantation with sutures. In addition, it avoids suture-related complications. It is useful for patients with pre-existing glaucoma with trabeculectomies, a procedure during which the surgeon may not like to tamper with the conjunctiva. Albeit iris-fixated lens is a good alternative, to date better long term outcomes have not been established for iris-fixated lenses or ACIOLs compared to PCSFIOL with sutures in the management of aphakia in post-vitrectomised eyes.
Sutureless PCSFIOL implantation with intrascleral haptic fixation and glued IOL procedures are gradually gaining recognition. Scharioth GB et al., reported good intermediate results without recurrent dislocation or retinal detachment in a median follow up of seven months [18]. In the glued IOL procedure described by Agarwal A et al., surgical fibrin glue sealant is used to secure the scleral flap and the externalized haptic to the scleral bed [19]. The fibrin glue assisted sutureless IOL scleral-fixation technique avoids suturing which invariably leads to reduction in complications such as persistent iris rubbing, pseudophakodonesis and ciliary body needle damage. A study published by Kumar DA et al., on glued IOL procedure in which there was one-year follow up showed good IOL centration outcomes without major complications [20]. Tissue glue, however, contains human products making infection transmission a risk factor. Irrespective of this risk, some vitreoretinal surgeons have used the technique in management of aphakia in post-vitrectomised eyes with Lee SJ et al., reporting comparable short term visual outcomes in their series of 31 eyes [21]. It is possible that there occurs late complications such as IOL subluxation or dislocation so further studies probing into its long term complication profile are needed to really accept or reject its efficacy.
In our centre, after the initial vitreoretinal surgery is performed, we wait for at least eight weeks for the surgical inflammation to resolve before we correct the aphakia with 9-0 PPS using the PCSFIOL approach. Comparative studies in primary and secondary PCSFIOL implantation are not conclusive with regards to which of the two is superior. According to Lee SJ et al., secondary implantation may have less early complications than the primary although late complications and final visual acuity were not significantly different in both scenarios [22]. The removal of a cataract during PPV is performed to enhance the vitreoretinal surgeon’s visualization of the posterior segment of the eye. We removed the lens capsule completely during PPV. It is possible to maintain the anterior capsule for subsequent IOL implantation without sutures, a procedure which is almost similar to PCIOL because in both cases the IOL is found behind the iris covered posteriorly by a capsule. However, the remaining anterior capsule has a risk of developing irido-capsular synechias which may complicate the secondary IOL implantation and also negatively affect the occurrence of postoperative refractive errors.
Limitation
A few aspects account for the limitations of our study; retrospective nature, multiple vitreoretinal surgeons performing the surgeries, one centre focus, lack of corneal endothelial cell account pre and postoperatively as well as variable follow up lengths.
Conclusion
The results of this study show excellent long term visual outcomes and low complication profile in correction of aphakia in post-vitrectomised eyes with implantation of PCSFIOL using 9-0 PPS in a large cohort of Indian eyes. Our study also shows very low 9-0 PPS breakage rate over a mean follow up period of 23 months. However, during the consent process for PCSFIOL implantation with sutures after combined PPV and lensectomy in correction of aphakia, patients should be carefully informed about the procedure, its merits and possible demerits taking into consideration preoperative history and other available surgical options. The visual outcomes and complication profile of our centre are comparable to other case series. Although patients have benefitted massively from its favourable long term safety, they should be informed before surgery about its suture related problems.
Contribution
FKO initiated the project, implemented and completed the data collection, NS contributed to statistical analysis. VKV, PS, RS and BD contributed to the management of cases and revised the paper. VKV, PS, RS and BD are guarantors.