A Study to Assess the Functional Outcome of Decompression and Posterior Lumbar Interbody Fusion of Low Grade Spondylolisthesis of Lumbar Vertebra
Deepak Hegde1, Sameer Mehra2, Santhosh Babu3, Arjun Ballal4
1 Associate Professor, Department of Orthopaedics, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
2 Postgraduate, Department of Orthopaedics, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
3 Senior Resident, Department of Orthopaedics, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
4 Consultant Orthopaedic Surgeon, Department of Orthopaedics, Ballal Healthcare, Udupi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arjun Ballal, Consultant Orthopaedic Surgeon, Department of Orthopaedics, Ballal Healthcare, Sweeny Complex, Santhekatte, Udupi Santhekatte, Udupi-576105, Karnataka, India.
E-mail: arjchess_lp@rediffmail.com
Introduction
Spondylolisthesis is defined as the forward displacement of one vertebra over the vertebra below. It is often accompanied by spinal canal stenosis and compression, which is the cause of all the symptoms.
Aim
To assess and study the functional outcome after decompression and Posterior Lumbar Interbody Fusion (PLIF) of isthmic spondylolisthesis of lower lumbar vertebra and to study the complications occurring with this technique.
Materials and Methods
A prospective study was conducted in the Department of Orthopaedics in Justice KS Hegde Charitable Hospital, Mangalore, Karnataka, India from March 2015 to August 2016. A total of 15 diagnosed patients with Grade I and II spondylolisthesis of L4-L5 and L5-S1 vertebrae with no neurological deficits, between the age group of 25-50 were included in the study. An initial two months of conservative treatment of back physiotherapy and flexion exercises was tried. Patients who did not improve with the conservative therapy were taken up for surgery with consent. Decompression and PLIF with bone grafting with interbody cage placement and pedicle screw instrumentation was performed. The patients were discharged on postoperative day 10 after suture removal. They were reviewed at postoperative day 10, week six and week 24. The scoring of the functional outcome of the back was done as per the Modified Oswestry low back pain Disability Questionnaire. The statistical analyses were done using the repeated measures ANOVA, SPSS version 20.
Results
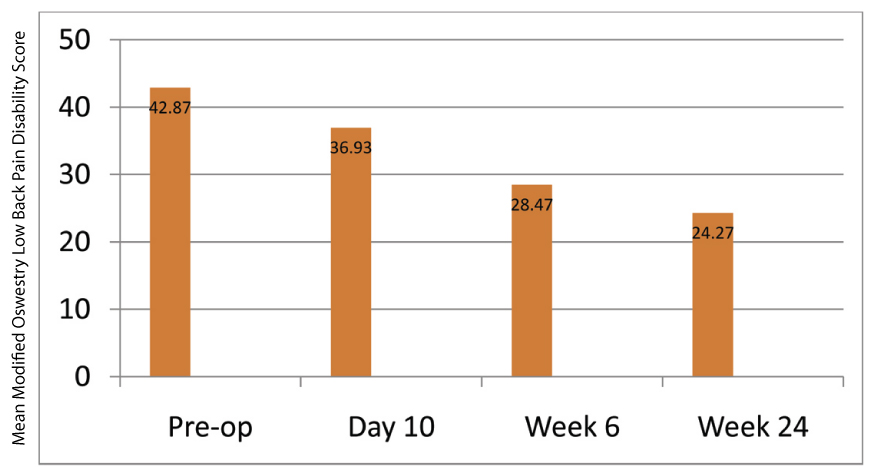
The mean Modified Oswestry low back pain Disability score preoperatively was noted to be 42.87+/- 3.46 points. The mean Modified Oswestry low back pain Disability score at postoperative day 10 was noted to be 36.93±3.75 points. The mean Modified Oswestry low back pain Disability score at postoperative week six was noted to be 28.47±3.70 points. The mean Modified Oswestry low back pain Disability score at postoperative week 24 was noted to be 24.27±3.01 points. Improvement in the Modified Oswestry low back pain Disability scores was noted during the follow ups. Foot drop was noted in two cases postoperatively which improved during the final follow up with physiotherapy.
Conclusion
Decompression and PLIF is noted to produce good to satisfactory functional results in cases of isthmic spondylolisthesis of lower lumbar vertebra.
Lumbar spine, Myerding slip grading, Neurological deficits
Introduction
In young adults, defect in the pars interarticularis (spondylolysis) is considered to be the commonest cause of spondylolisthesis [1]. Kilian first described spondylolisthesis in 1854 [1]. Acute low back pain is the major symptom of spondylolisthesis. Ligamentous strain from instability at the level of the slip can produce chronic low back pain. Traction and pressure on the nerve roots may predispose to sciatica and may also cause disc bulge [2].
Over the years several surgical techniques have been developed of which fusion of the vertebra with or without instrumentation is the most popular [1]. PLIF is one of the most popular technique of fusion and instrumentation that is employed in management of these conditions [3].
PLIF was introduced by Briggs and Milligan in 1944; they employed the bone chips after laminectomy as interbody graft [4]. But the popularity of PLIF increased when Cloward employed iliac crest bone grafts [4]. PLIF was reported to have over 85% fusion rates but was plagued with complications such as arachnoiditis, neural injury, graft extrusion etc., [4]. It was only in the 1990s when interbody implants developed and the ease with which they could be inserted increased the popularity of PLIF [4]. Synthetic cages and pre milled allografts have become a part of PLIF in stabilizing the vertebral end plates and maintaining the inter-discal height [4].
Bone grafting is sometimes associated with several complications as graft resorption, failure of hardware etc. Lately threaded fusion cages have been reported to maintain disc height and also bring about good fusion rates [5].
This study was done to assess and study the functional outcome after decompression and PLIF of isthmic spondylolisthesis of lower lumbar vertebra and to study the complications occurring with this technique.
Materials and Methods
A prospective study was conducted in the Department of Orthopaedic Surgery of Justice KS Hegde Charitable Hospital, Deralakatte, Mangalore, Karnataka, India from March 2015 to August 2016, after obtaining ethical clearance from the institution ethics committee and informed consent from the patients. Spondylolisthesis was diagnosed in the patients with flexion, extension X-Rays and MRI [Table/Fig-1]. A total of 15 patients meeting the inclusion criteria were included into the study. Diagnosis of spondylolisthesis was done and the percentage of slip was calculated as per the Myerding slip grading [6]. All the patients had symptoms for an average period of two years. Nine of these 15 patients were manual labourers who presented with a history of lifting heavy weights. All the patients presented with increase in symptoms while climbing up the staircase. All the patients had radiation of pain in one of the lower limbs. None had radiation to both lower limbs. A complete clinical assessment (Straight leg raising test-30 to 60 degrees) was done of all the patients. All the patients had undergone a minimum two months of conservative management for the symptoms with analgesics, flexion exercises and back physiotherapy and a lumbosacral brace was also applied. The inclusion criteria consisted of patients between the age groups of 25-50 years, Grade I and II anterolisthesis (as per the Myerding slip grading), non responsive to conservative management. Patients with history of recent trauma to the back, Grade III, IV and V Spondylolisthesis, retrolisthesis, diabetes, hypertension, associated spinal conditions and fractures, history of previous spine surgery, patients refusing surgery, patients with neurological deficits, patients with evident degeneration of the spine and age over 50 years and below 25 years were excluded. Preoperative assessment was done and scoring of function was done as per the Modified Oswestry low back pain Disability index [7].
Surgical technique: The patients were positioned prone for surgery. A midline incision was made and complete bone exposure was done and dissection was continued till the transverse processes were exposed. A medial laminectomy and extensive forminotomy after medial facetectomy was performed. After the placement of interbody cages and autologous bone graft, pedicle screw rod instrumentation was performed using the conventional technique. The bone graft harvesting was done from the laminae, articular facets and spinous processes. Nerve root retraction was done medial wards after ligamentum flavum resection. After complete discetomy end plate preparation was performed after distraction of disc space. Interbody cages were filled with morcelized bone chips. Wound closure was performed in layers over a suction drain. Postoperative antero-posterior and lateral radiographs were taken [Table/Fig-2]. Patient was assessed for neurological complications in the immediate postoperative and during all the reviews. Postoperative antibiotics were continued till postoperative day five. Mobilization was started on postoperative day three after application of a lumbosacral brace. Drain removal was done on postoperative day three to four depending on the amount of drain collection. Suture removal and discharge was done on postoperative day 10. Scoring was done as per the Modified Oswestry low back pain Disability index on day 10. Patient was followed up for six weeks and then at 24 weeks and functional outcome was assessed as per the Modified Oswestry low back pain Disability index during all the reviews. X-Rays were taken in anteroposterior and lateral views to assess for complications, during all the reviews.
MRI sagittal view showing a Grade II L4-L5 anterolisthesis (marked by the red circle).

Postoperative lateral and anteroposterior image after bone grafting, pedicle instrumentation and cage fixation.
Statistical Analysis
All the results were tabulated and calculated statistically as per the repeated measures ANOVA, SPSS version 20.
Results
A total of 15 patients were included into the study. The mean age of the patients under the study was 43 years. Nine patients were females and six patients were males. Seven of the 15 patients had L4-L5 spondylolisthesis and eight patients had L5-S1 spondylolisthesis. Nine patients had Grade I spondylolisthesis and six patients had Grade II spondylolisthesis. The mean Modified Oswestry low back pain Disability score preoperatively was noted to be 42.87±3.46 points. The mean Modified Oswestry low back pain Disability score at postoperative day 10 was noted to be 36.93±3.75 points. The mean Modified Oswestry low back pain Disability score at postoperative week six was noted to be 28.47±3.70 points. The mean Modified Oswestry low back pain Disability score at postoperative week 24 was noted to be 24.27+/- 3.01 points [Table/Fig-3]. Improvement in the Modified Oswestry low back pain Disability scores was noted during the follow ups. Foot drop was noted in two cases postoperatively which improved during the final follow up with physiotherapy.
Bar graph representing the improvement in the Modified Oswestry low back pain Disability index from preoperative period to review week 24.
Discussion
Operative fusion for spondylolisthesis has better outcomes than conservative management [1]. Interbody fusion is a technique which has its advantages over other techniques of management in several ways. Considering the biomechanics, the bone graft is placed in the centre of weight bearing zone of the spine wherein axial load is 80% [1]. Doing this maintains the sagittal balance and the disc height which provides optimal conditions for higher fusion rates and also is responsible for blood supply which is extensive from the end plates of the adjacent vertebrae [1].
The major advantage of PLIF is that the extent of posterolateral soft tissue exposure and muscle stripping is greatly limited. The use of Titanium cages provide the advantage of prevention of collapse and fracture which tends to happen with bone grafting without cage [1]. In addition the strength of the graft do not exceed the physiological loads of the spine [1].
The second advantage in cage fusion is the amount of bone graft required is also significantly reduced. The design of the cage permits bone growth around it and also augments to the strength of the construct when used with a rigid posterior instrumentation system [2,7].
PLIF is noted to have high clinical satisfaction rate and fusion rate. The main cause of improved fusion in PLIF is attributed to the repositioning of the intra discal height, the exposure of the bleeding cancellous bone surfaces and removal of end plates [1].
Cages are noted to restrict segmental motion and aid in anterior column reconstitution. The graft compression is done and blood supply from adjoining vertebral arteries is provided. Distraction of the interspace is also done hence; posterior foraminal height is also maintained [1].
We noted in our series that there was a higher predisposition of spondylolisthesis in men as compared to women. These results are comparable to those of Fathy and colleagues, who reported an incidence higher in females as compared to males [1]. The mean age of patients under study was under our series who presented with low grade spondylolisthesis was 43 years, these results are comparable to those of Fathy and colleagues who recorded a mean age of 36 years [1].
We noted an improvement in the Modified Oswestry low back pain Disability score after immediate postoperative period and during the final follow up at 24 weeks. This showed improvement in symptoms in the patients after surgery during the follow up. These results are comparable to those of Molinari et al., who reported an overall satisfaction rate of 70% in 30 cases included in the study [8]. Fathy and colleagues also reported a fusion rate of 88% and satisfaction rate of 76% [1].
Two of our patients were noted to have developed foot drop immediately after surgery which improved during the course of the reviews. These results were comparable to those of Molinari et al., who reported a 17% complication rate in their series of 30 cases [8].
Jacobs et al., studied different techniques for management of spondylolisthesis and concluded that with PLIF excellent or good clinical outcome was 45% and fusion rate was 80 and 95% [9]. We noted good results in our cases also.
Limitation
The sample size was small, consisted only 15 patients as we excluded all grade III, IV and V spondylolisthesis. The follow period was limited to just 24 weeks as most of the cases were from distant places and did not turn up for reviews after 24 weeks.
Conclusion
Decompression and PLIF is a good technique for management of low grade spondylolisthesis of lower lumbar vertebra with good functional outcome and minimal complication rate.
[1]. Fathy M, Fahmy M, Fakhri M, Aref K, Abdin K, Zidan I, Outcome of instrumented lumbar fusion for low grade spondylolisthesis; Evaluation of interbody fusion with and without cagesAsian J Neurosurg 2010 5(1):41-47. [Google Scholar]
[2]. Elias WJ, Simmons NE, Kaptain GJ, Chadduck JB, Whitehill R, Complications of posterior lumbar interbody fusion when using a titanium cage deviceJ Neurosurg [Spine] 2000 93:45-52. [Google Scholar]
[3]. Lee CK, Kopacz KJ, Lumbosacral: Posterior Lumbar interbody fusion. In: Herkowitz HN, et al., editorsRothman – SimeoneThe Spine 2006 PhiladelphiaElsevier:350-60. [Google Scholar]
[4]. Cole DC, McCall DT, Schmidt HM, Dailey TA, Comparison of low back fusion techniques: Transforaminal lumbar interbody fusion (TLIF) or posteriorlumbar interbody fusion (PLIF) approachesCurr Rev Musculoskelet Med 2009 2(2):118-26. [Google Scholar]
[5]. Klara PM, Freidonk SA, Rezaimiri S, Comparison of lumbar interbody fusion techniques using Ray Threaded fusion cages and pedicle screw fixation systemsNeurosurgry Quarterly 2003 13(1):20-29. [Google Scholar]
[6]. Wright IP, Who was Meyerding?Spine (Phila Pa 1976) 2003 28(7):733-35. [Google Scholar]
[7]. Fritz JM, Irrgang JJ, A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability ScalePhysical Therapy 2001 81:776-88. [Google Scholar]
[8]. Molinari RW, Sloboda JF, Arrington EC, Low grade isthmic spondylolisthesis treated with instrumented posterior lumbar interbody fusion in U.S. servicemenJ Spinal Disord Tech 2005 18(Suppl):S24-29. [Google Scholar]
[9]. Jacobs WC, Vreeling A, De Kleuver M, Fusion for low grade adult isthmic spondylolisthesis: A systematic review of the literatureEur Spine J 2006 15(4):391-402. [Google Scholar]