Bilateral Synchronous Paratesticular Leiomyoma - A Rare Entity
Amrit Fernandez1, Sriram Krishnamoorthy2, Susruthan Muralitharan3, Thanka Johnson4, Venkat Ramanan5
1 Registrar, Department of Urology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India.
2 Professor, Department of Urology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India.
4 Professor, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India.
5 Professor, Department of Urology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Krishnamoorthy Sriram, Professor, Department of Urology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu-600116, India.
E-mail: sriramuro@gmail.com
Paratesticular region is an obscure anatomical region that includes spermatic cord and its contents, tunica of the testes, epididymis and appendices of epididymis and testis. Paratesticular tumours may closely resemble and be clinically indistinguishable from testicular tumours, resulting in a diagnostic dilemma. Preoperative distinction between the benign and malignant paratesticular tumour is extremely difficult, resulting in difficulty in diagnosis and management. We hereby present a case of a 56-year-old male who reported with a painless bilateral scrotal mass and underwent surgical excision of the same. The final biopsy report was paratesticular leiomyoma. The main purpose of this manuscript is to emphasize on the fact that it is imperative for the treating urologists to be aware of such potentially benign rare entity. A high index of clinical suspicion is mandatory, as lack of knowledge about this condition would result in an unnecessary radical orchidectomy.
Adenomatoid, Epididymal mass, Orchidectomy
Case Report
A 56-year-old male presented with vague and non-specific scrotal pain, on and off for the past eight months. He also noticed two nodular swellings, one on either side of the lower pole of the testes for the past three months. Both the swellings were insidious in onset, painless and synchronously affecting bilaterally. He gave no history of trauma, fever, dysuria or haematuria. He is hypertensive for the past five years. He had undergone bilateral hernioplasty and haemorrhoidectomy in the past.
Physical examination revealed normal external genitalia. Both testes were palpable and normal in size. Two non tender 3 x 3 cm well circumscribed hard masses were palpable, one each on either side of the scrotum, along the lower pole of the testes and adherent to it. The testis and the epididymis were distinctly palpable well away from the mass. Both the masses were nodular, well circumscribed, non-tender and attached to the testis, but well demarcated from the epididymis and the lower poles of the testes. There were no other intra-abdominal masses or lymphadenopathy.
Blood biochemistry and testicular tumour markers were normal. Scrotal ultrasonography revealed a 3 x 3 cm mass lesion on both sides of the scrotum separate from the testicles but closely adherent to it. Both testes were normal. A clinical diagnosis of bilateral epididymal mass was made and bilateral excision of the mass was done. Intra-operatively, there was a 3 cm firm, well encapsulated solid grey mass arising in the paratesticular region. The mass was separate from the testis and the epididymis.
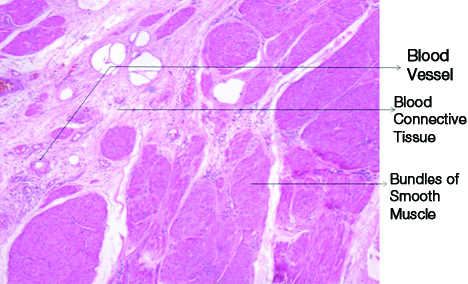
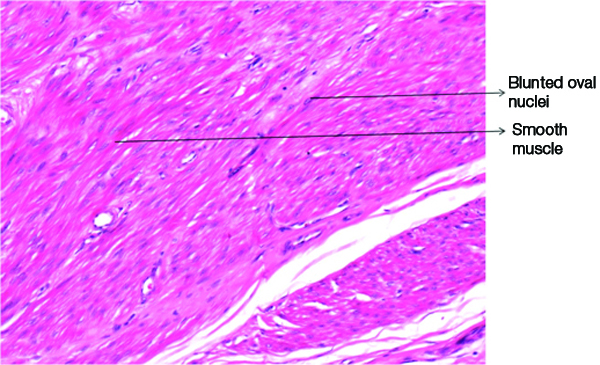
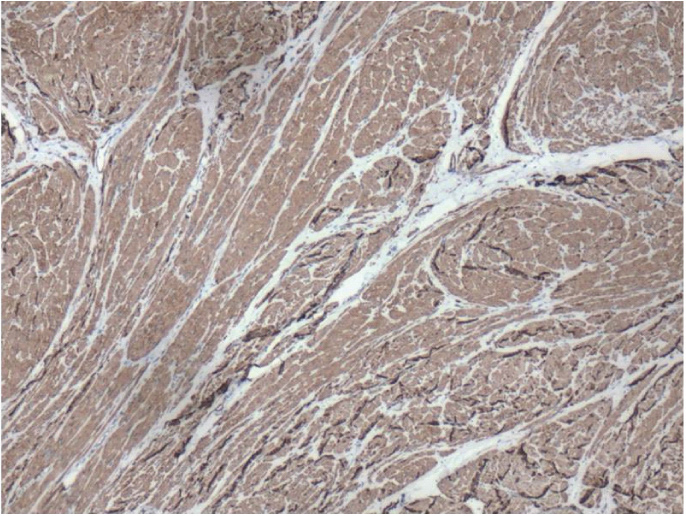
Gross examination showed a solid grey white, circumscribed firm mass. The cut surface revealed a grey white solid mass with whorling pattern [Table/Fig-1]. Microscopic examination revealed fascicles and bundles of spindle-shaped smooth muscle cells with focal degeneration. There was no evidence of atypia, increased mitosis or necrosis [Table/Fig-2,3]. Immuno histochemistry showed smooth muscle actin positivity in the cytoplasm confirming the diagnosis of paratesticular leiomyomas [Table/Fig-4].
Cut surface of the excised paratesticular masses.

Showing the lesion showing smooth muscle bundles arranged in fascicles. (H&E stain, 10X view).
Lesion showing smooth muscle bundles with blunted nuclei. (H&E stain, 40X view).
Immuno histochemical staining for smooth muscle activity, 4X view, showing diffuse positivity by the smooth muscle bundle.
Discussion
Paratesticular leiomyomas are exceedingly rare tumours affecting the genito urinary system. The overall incidence of bilateral paratesticular leiomyomas can be as high as 17.7% [1]. Most of them are synchronous but may occasionally be asynchronous. These tumours mostly occur in the fifth decade of life [2]. Bilateral synchronous leiomyomas are extremely scarce to see in clinical practice. To the best of our knowledge, this is only the second such case being reported in the world literature only after Alasamar et al., had reported a similar case earlier in 2014 [1]. It is very difficult to distinguish the leiomyomas affecting the testis from those of the paratesticular region by simple clinical examination alone [3]. In our manuscript, we describe a case of bilateral synchronous leiomyomas of the paratesticular region without involvement of the testis or the epididymis. To the best of our knowledge, this is the first case to be reported in Indian literature.
Paratesticular region is an intricate anatomical region that includes spermatic cord and its contents, tunica of the testes, epididymis and their vestigial remnants like appendices of epididymis and testis [4]. The most common benign tumours in the paratesticular regions include adenomatoid tumours, leiomyomas and lipomas of which adenomatoid tumours are the commonest and leiomyomas are the second most common tumours [5].
Leiomyomas of the scrotum are benign, smooth muscle tumours. Most of these lesions are indolent, slow growing and are often asymptomatic. Although epididymis is the most common site of scrotal leiomyomas, they can occur in other sites of scrotum as well including spermatic cord, dartos, tunica albuginea and testicular parenchyma as well [6]. They most often manifest between 40 and 50 years of age [7].
Paratesticular masses represent approximately 2% of intrascrotal tumours. These tumours exhibit slow and indolent growth, majority of them (about 70%) being non-malignant in nature [8]. The remaining 30% of paratesticular masses are malignant, the most frequent being sarcomas [9]. Leiomyosarcomas of the paratesticular region is extremely rare and such malignancies constitute only 10% of all paratesticular sarcomas [10].
Our patient had a benign lesion that gradually increased in size over the past three months. Clinically the mass appeared benign and distinct from rest of the testicular and epididymal tissue. Ultrasonologically the mass was distinct from the testis and epididymis and was heterogenous in echotexture. However, since the epididymal tumours are the more common ones that come across in clinical practice, a provisional clinical diagnosis of an epididymal mass was made. A detailed history and a thorough clinical examination are required in order to make a diagnosis of paratesticular tumour. Ultrasound of scrotum is the gold standard investigation that would give us information regarding the nature of the lesion, its size, echogenicity, presence of any necrotic areas and its relation to testis and epididymis [11]. MRI is a complementary test specifically useful in those cases in doubt. Mugilia V et al., in his study demonstrated that MRI can to a large extent distinguish benign from malignant ones with a high degree of precision [12].
The age at the time of presentation as well as symptom duration is helpful in diagnosing these tumours. Physical examination is also helpful in identifying a lump in the scrotal region. Diagnosis is done primarily by high resolution ultrasonography where most of the times, the benign tumours are homogeneous and hyperechoic. Sonography can easily distinguish testicular from paratesticular lesions. Ozden O et al., reported that sonography can distinguish the two conditions with highest degree of accuracy, to the extent of 95 to 100%. They also added that one can differentiate solid from cystic lesions and can also identify pathology in adjacent organs as well [13].
Leiomyomas are usually well circumscribed and are surrounded by a gray – white fibrous capsule. Cut surface shows bulges and exhibits a whorled pattern. Histologically, the tumour consists of smooth muscle cells arranged in interlacing bundles with varying mixtures of fibrous and often hyalinized connective tissue [14]. However, the true identity of epididymal leiomyoma is often masked until histologic study is made. Hence excision of the intrascrotal tumour through inguinal approach is recommended [2,15]. Trans scrotal excision is also done if an absolute certainty of its benign nature is made clinically and biochemically. Hence, proper preoperative evaluation of the patient is mandatory, as paratesticular leiomyomas are rare benign tumours which sometimes have the same presentation as testicular tumours. Testis sparing procedures should be the goal in such circumstances.
Conclusion
Paratesticular leiomyomas are extremely uncommon tumours affecting the male genitalia. Most of such tumours run a benign course and are indolent showing a slow growth and are non-invasive. A high index of clinical suspicion is required in making an accurate diagnosis of this rare entity. Timely diagnosis and appropriate treatment would largely preclude the need for orchidectomy in most of the patients.
[1]. Alasmar A, Alkaabna A, Aljader K, Alsaaydah N, Waqfi O, Bilateral synchronous paratesticular leiomyoma: A case reportJRMS 2014 21(2):60-63. [Google Scholar]
[2]. Chiong E, Tan KB, Siew E, Rajwanshi A, See H, Esuvaranathan K, Uncommon benign intrascrotal tumoursAnn Acad Med Singapore 2004 33(3):351-55. [Google Scholar]
[3]. Tammela TL, Karttunen TJ, Mäkäräinen HP, Hellström PA, Mattila SI, Kontturi MJ, Intrascrotal adenomatoid tumoursJ Urol 1991 146(1):61-65.Review [Google Scholar]
[4]. Yamamoto M, Miyake K, Mitsuya H, Intrascrotal extratesticular neurofibromaUrology 1982 20:200-01. [Google Scholar]
[5]. Lioe TF, Biggart JD, Tumours of the spermatic cord and paratesticular tissue. A clinicopathological studyBr J Urol 1993 71:600-06. [Google Scholar]
[6]. Leonhardt WC, Gooding GA, Sonography of epididymal leiomyomaUrology 1993 41(3):262-64. [Google Scholar]
[7]. Hertzberg BS, Kliewer MA, Hertzberg MA, Distell BM, Epididymal leiomyoma: sonographic featuresJ Ultrasound Med 1996 15(11):797-99. [Google Scholar]
[8]. Roman Birmingham PI, Navarro Sebastian FJ, Garcia Gonzalez J, Romero Barriuso G, Guijarro Espadas A, Paratesticular tumours. Description of our case series through a period of 25 yearsArch Esp Urol 2012 65(6):609-15. [Google Scholar]
[9]. Celik O, Unlu G, A rare case: paratesticular leiomyosarcomaAsian J Androl 2013 15(6):843-44. [Google Scholar]
[10]. Lopes R, Leite KR, Lopes RN, Paratesticular leiomyosarcoma treated by enucleationInt Braz J Urol 2006 32:66-67. [Google Scholar]
[11]. Khoubehi B, Mishra V, Ali M, Motiwala H, Karim O, Adult paratesticular tumoursBJU Int 2002 90(7):707-15. [Google Scholar]
[12]. Muglia V, Tucci S, Elias J, Simao C, Bilbey J, Cooperberg P, Magnetic Resonance imaging of scrotal disease: when it makes the differenceUrology 2002 59(3):419-23. [Google Scholar]
[13]. Ozden O, Orhan D, Karnak I, Epididymal leiomyoma: an unusual intrascrotal tumour in a childJ Pediatr Surg 2009 44(9):e5-7. [Google Scholar]
[14]. Akbar SA, Sayyed TA, Jafri SZ, Hasteh F, Neill JS, Multimodality imaging of paratesticular neoplasms and their rare mimicsRadiographics 2003 23(6):1461-76. [Google Scholar]
[15]. Cakiroglu B, Ozcan F, Ates L, Aksoy SH, Leiomyoma of the epididymis treated with partial epididymectomyUrol Ann 2014 6(4):356-58. [Google Scholar]