Youngest Case of Allergic Broncho Pulmonary Aspergillosis in India: A Case Report from Arid Zone of India
Navgeet Mathur1, Medha Mathur2, Virendra Singh3
1 Senior Resident, Department of General Medicine, Dr. Sampurnanand Medical College, Jodhpur, Rajasthan, India.
2 Senior Resident, Department of Community Medicine and Family Medicine, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
3 Professor, Department of General Medicine, Sawai Man Singh Medical College, Jaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Medha Mathur, 306, PG Hostel, AIIMS, Basni Industrial Area, Phase II, AIIMS, Jodhpur- 342005, Rajasthan, India.
E-mail: drmedhamathur@yahoo.co.in
Allergic Broncho Pulmonary Aspergillosis (ABPA) is an immunological allergic disorder and asthmatic patients are predisposed to ABPA. Although, ABPA commonly develops in the third and fourth decades but no age group is unaffected from the disease. Youngest case of ABPA in India so far reported was four years of age. This case report is about a young child of bronchial asthma with ABPA aged four years and nine days only, from arid zone of country. Her diagnosis of ABPA was supported by clinical, serological and radiological findings. This case report concludes the importance of early diagnosis and treatment of ABPA along with general awareness for the disease.
Aspergillus fumigatus, Bronchial asthma, Immunological allergic disorder
Case Report
A four-year-old female patient presented with complaint of repeated episodes of dry cough, shortness of breath and whistle like breath sounds. She had similar episodes for last three years aggravated by cold weather and also had history of reversibility of symptoms by some inhalation medication on previous medical consultation. She was diagnosed as bronchial asthma on the basis of clinical symptoms, clinical examination and pulmonary function test. Patient was the only child of her parents and had no significant family history of similar illness. She was born by uncomplicated normal vaginal institutional delivery and had history of proper immunization according to her age. She was having normal development milestones with normal school performance. After her first episode of breathlessness, at the age of nearly one year she frequently visited Paediatrics Department for similar illness. For her present illness of dry cough, shortness of breath and whistle like breath sounds she was referred by Paediatric Department to Division of Allergy and Respiratory Medicine under General Medicine Department for further evaluation. There was no history of fever, weight loss, palpitation, chest pain, drug abuse, bluish discolouration of body parts or any blood loss. Routine investigations like haemoglobin, total leucocytes count, platelet count, blood sugar, liver function tests, renal function tests were within normal limits.
After consent of her parents she became part of study in which 300 bronchial asthma patients were evaluated to know the prevalence of ABPA in asthmatic patients [1]. She was subjected to detail history and clinical examination. On respiratory examination she was having tachypnoea, bilateral vesicular breath sounds with inspiratory and expiratory wheeze on lung auscultation. No significant abnormality was found on examination of other systems. She was then screened for ABPA through Skin Prick Test (SPT) for five common fungal antigens namely Aspergillus fumigatus, Aspergillus flavus, Aspergillus niger, Aspergillus tamarii, and Aspergillus versicolor. The patient was not allowed to use antihistamines and steroids by oral or parenteral route in the preceding 72 hours. Credisol Aspergillus antigens manufactured by Creative Diagnostic Medicare Pvt. Ltd. Mumbai was used. Histamine 0.1% w/v and normal saline 0.9% w/v were used as a control for SPT. The mean wheal diameter was measured after 20 minutes. The result of the test was measured according to Shivpuri’s criteria of grading positive skin prick reactions [2]. A wheel >2 mm than the size of the negative control was considered as positive result for SPT. This young patient was found SPT positive for A. fumigatus.
Further evaluation was done through serum total IgE level, pulmonary function test, chest roentgenogram, High Resolution Computed Tomography (HRCT) of thorax. The total serum IgE was assessed by the ELISA method and total IgE level >1000 ng/ml was taken as positive result. Easy One NDD spirometer was used for spirometry along with bronchodilator reversibility test. Reversibility was defined according to the American Thoracic Society (ATS) guidelines as 12% and 200 ml increase in the FEV1 following bronchodilator (200 μg of inhaled Salbutamol) as compared to the pre-bronchodilator value [3]. All recent and previous chest radiographs were reviewed for the presence of fleeting opacities, tooth-paste and gloved finger shadows, ring shadows, tramline or for evidence of fibrosis. HRCT scan of the chest was done to look for any bronchiectasis (central=if confined to the inner 2/3 of the lung field on either side), parenchymal fibrosis and mucous plug. A 128-Slice Phillips imaging CT scan machine was used with a slice thickness of 1.25 mm.
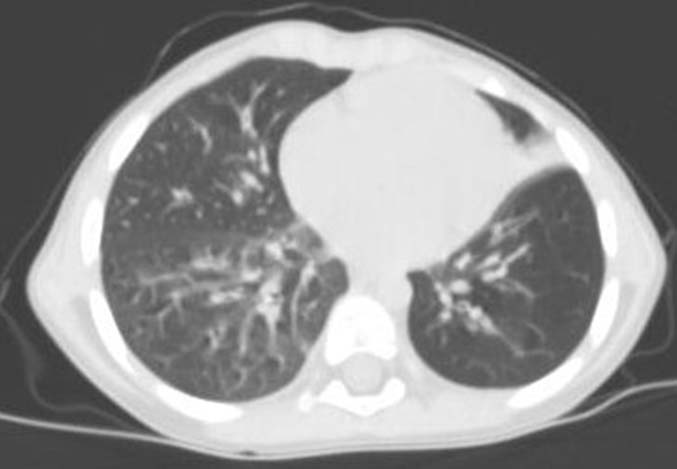
On investigation, serum total IgE level was found 2233.8 IU/ml, there were presence of perihilar opacities on chest roentgenogram [Table/Fig-1]. HRCT thorax showed central bronchiectasis, perihilar areas of infiltration, tree in bud nodules with perihilar ground glass haziness [Table/Fig-2]. Diagnosis of ABPA was made on the basis of bronchial asthma history and evident findings of SPT, total serum IgE level, chest roentgenogram, HRCT thorax. At the time of diagnosis she was only four years and nine days of age. Patient was treated for ABPA with methylprednislone 0.75 mg/kg/day for six weeks followed by 0.5 mg/kg/day for six weeks then tapered by 5 mg every six weeks to continue for a total period of six months. It led to significant clinical and radiological improvement. There was no episode of similar illness during the period of steroid therapy. After further follow up for one and a half year it was found that she was benefited as no significant episodes of shortness of breath occurred, although there were few episodes of coryza without breathlessness and were easily treated by antihistaminics. There was decline in hospital visits for acute illness.
Chest X-Ray showing perihilar opacities.

HRCT thorax showing central bronchiectasis, perihilar areas of infiltration and tree in bud nodules.
Discussion
ABPA was first described by Hinson KF et al., and first reported in India by Shah JR [4,5]. As the name signifies, ABPA is an allergic disorder most commonly involves respiratory system and Aspergillus fungi is most common allergen responsible for it. Patients of bronchial asthma and cystic fibrosis are typically predisposed to ABPA. In due course of time, ABPA can worsen the course of pre-existing asthma or cystic fibrosis and can lead to irreversible lung damage. It can lead to bronchiectasis, lung cavitations, collapse, consolidation, pulmonary fibrosis and pulmonary hypertension by its own course. Steroids and antifungal drugs, mainly itraconazole are the main line of treatment for this disease. Early diagnosis and treatment can prevent a variety of complications [6,7].
ABPA can develop at any age but it most commonly develops in the third and fourth decades of life [6,8]. In most of the Indian studies mean age of ABPA was found to lie between 30 to 37 years like Agarwal R et al., (33.4 years), Behera D et al., (34.3 years), Kumar R and Gaur SN (34 years), Chakrabarti A et al., (36.4 years), Agarwal R et al., (34.4 years), Prasad R et al., (33.5 years) and Sarkar A et al., (33.1 years) [8-14]. So far the youngest case of ABPA in India was reported by Gaur SM et al., in 2006 and that patient was a four years old female although exact age was not mentioned in months and days [15]. But the confirmed age of our patient was four years and nine days at the time of the diagnosis. Probably she is the youngest case of ABPA so far reported in India. The presence of ABPA in such younger age warrants the necessity of screening of every asthmatic patient for ABPA at early age. It is necessary to diagnose the disease entity timely to avoid irreversible complications.
The prime studies conducted so far in India like Kumar R and Gaur SM, Maurya V et al., Agarwal R et al., and Agarwal R et al., had high prevalence of ABPA of 16%, 7.6%, 27.2%, and 20.5% respectively in asthmatic patients [8,10,12,16]. Although, few literatures and studies found these prevalence much higher than actual, due to referral and selection bias of the subjects to the tertiary level institutes [1,6,14,17].
SPT for Aspergillus can play role in screening of asthmatic patients. SPT and chest roentgenogram should be done in every patient having bronchial asthma. These tests carry the benefit of being cost effective and can help in further evaluation and diagnosing suspected cases.
It is also important that such cases should not be misdiagnosed as pulmonary tuberculosis. It can be concluded that there is inevitable need of sensitizing doctors regarding early diagnosis and proper treatment of the ailment. Up to 50% cases of ABPA are initially misdiagnosed as having pulmonary tuberculosis [12] due to similarity in radiographic features of both diseases and a tendency of Indian health care providers to over diagnose tuberculosis as abnormalities in chest radiographs are usually considered to be tuberculosis unless proven otherwise.
Conclusion
All the asthmatic patients should under go screening for ABPA as early as possible. Screening programme for ABPA should be started, targeting asthmatic preschool and school children to prevent irreversible lung damage in later age. Effort should be made about knowledge and awareness of the disease in general population as well as in medical practitioners to prevent overuse of anti-tubercular medication.
[1]. Mathur N, Mathur M, Prevalence of allergic broncho pulmonary aspergillosis in patients with asthma attending allergy clinic in a north-west Indian tertiary care instituteInternational Journal of Biomedical and Advance Research 2016 7(5):230-34. [Google Scholar]
[2]. Shivpuri DN, Comparative evaluation of sensitivity of common methods of diagnostic antigen tests in patients of respiratory allergyIndian J Chest Dis 1962 4:102 [Google Scholar]
[3]. American Thoracic SocietyStandardization of spirometry:1994 updateAm J Respir Crit Care Med 1995 152:1107-36. [Google Scholar]
[4]. Hinson KF, Moon AJ, Plummer NS, Broncho pulmonary Aspergillosis; a review and a report of eight new casesThorax 1952 7:317-33. [Google Scholar]
[5]. Shah JR, Allergy pulmonary aspergillosisJ assoc. Physicians India 1971 19:835-41. [Google Scholar]
[6]. Agarwal R, Allergic bronchopulmonary aspergillosisCHEST 2009 135:805-26. [Google Scholar]
[7]. Gupta RK, Chandr A, Gautam PB, Allergic bronchopulmonary aspergillosis: A clinical reviewJ Assoc Physicians India 2012 60:46-51. [Google Scholar]
[8]. Agarwal R, Gupta D, Aggarwal AN, Saxena AK, Chakrabarti A, Jindal SK, Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: an analysis of 155 patientsChest 2007 132(4):1183-90. [Google Scholar]
[9]. Behera D, Guleria R, Jindal SK, Chakrabarti A, Panigrahi D, Allergic bronchopulmonary aspergillosis: a retrospective study of 35 casesIndian J Chest Dis Allied Sci 1994 36(4):173-79. [Google Scholar]
[10]. Kumar R, Gaur SN, Prevalence of allergic bronchopulmonary aspergillosis in patients with bronchial asthmaAsian Pac J Allergy Immuno 2000 18:181-85. [Google Scholar]
[11]. Chakrabarti A, Sethi S, Raman DS, Behera D, Eight-year study of allergic bronchopulmonary aspergillosis in an Indian teaching hospitalMycoses 2002 45(8):295-99. [Google Scholar]
[12]. Agarwal R, Gupta D, Agarwal AN, Behera D, Jindal SK, Allergic bronchopulmonary aspergillosis: lesson from 126 patients attending a chest clinic in north IndiaChest 2006 130:442-48. [Google Scholar]
[13]. Prasad R, Garg R, Sanjay Dixit RP, A study on prevalence of allergic bronchopulmonary aspergillosis in patients of bronchial asthma[Internet] J Pulmonary Med 2014 9(2)[Cited 2014 Feb 22] Available from: http://connection.ebscohost.com/c/articles/30030236/study-prevalence-allergic-bronchopulmonary-aspergillosis-patients-bronchial-asthma [Google Scholar]
[14]. Sarkar A, Mukherjee A, Ghoshal AG, Kundu S, Mitra S, Occurrence of allergic bronchopulmonary mycosis in patients with asthma: An Eastern India experienceLung India 2010 27(4):212-16. [Google Scholar]
[15]. Gaur SN, Khan ZU, Kumar R, Youngest patient of ABPA in Indian subcontinent – A case reportIndian J Allergy Asthma Immunol 2006 20:37-40. [Google Scholar]
[16]. Maurya V, Gugnani HC, Sarma PU, Madan T, Shah A, Sensitization to Aspergillus antigens and occurrence of allergic bronchopulmonary aspergillosis in patients with asthmaChest 2005 127(4):1252-59. [Google Scholar]
[17]. Denning DW, Pleuvry A, Cole DC, Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adultsMed Mycol 2013 51(4):361-70. [Google Scholar]