Ultrasound Guided Percutaneous Injection of Thrombin: Effective Technique for Treatment of Iatrogenic Femoral Pseudoaneurysms
Atul Mishra1, Akhilesh Rao2, Yayati Pimpalwar3
1 Interventional Radiologist, Department of Radiodiagnosis and Interventional Radiology, Military Hospital (Cardio Thoracic Centre), Pune, Maharashtra, India.
2 Radiologist, Department of Radiodiagnosis and Interventional Radiology, Command Hospital (CC), Lucknow, Uttar Pradesh, India.
3 Radiologist, Department of Radiodiagnosis and Interventional Radiology, Command Hospital (CC), Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Atul Mishra, Interventional Radiologist, Department of Radiodiagnosis and Interventional Radiology, Military Hospital (Cardio Thoracic Centre), Pune, Maharashtra, India.
E-mail: atul_mish12@hotmail.com
Introduction
Arterial pseudoaneurysms are well known iatrogenic complication of percutaneous angiographic or interventional vascular procedures. In the past, the definitive treatment option was open surgical repair which is a relatively invasive procedure. In the last few years, Ultrasound (US) guided percutaneous thrombin injection has been gaining popularity as definitive treatment of pseudoaneurysms.
Aim
To evaluate efficacy and safety of US guided percutaneous injection of thrombin for treatment of iatrogenic femoral pseudoanurysms at a tertiary care interventional radiological and cardiology centre.
Materials and Methods
A retrospective analysis was conducted on 38 consecutive patients, diagnosed to have iatrogenic femoral artery pseudoaneurysms by Doppler study, in the period from Jan 2013 to Jun 2016. All these patients were treated by US guided percutaneous injection of thrombin solution inside the pseudoaneurysm sac till contents became echogenic and flow inside the pseudoaneurysm stopped completely. One month further follow up in all these patients was done.
Results
The dose of thrombin injected varied from 200-1000 IU (mean 300 IU). Immediate thrombosis was seen in all the pseusdoaneurysms. Follow up at 24-48 hours showed complete thrombosis and regression of pseudoaneurysm in all the patients except one in whom a small residual sac was seen which thrombosed completely on second thrombin injection. Further follow up at one month showed regression of aneurysms in all the cases. No significant post procedural clinically significant complications were seen in any of the patients.
Conclusion
US guided percutaneous thrombin injection is a highly successful and safe procedure for the treatment of iatrogenic femoral pseudoaneurysms.
Endovascular procedure, Femoral artery, Interventional radiology
Introduction
A pseudoaneurysm is a contained rupture of an artery into the surrounding tissue. It is characterized by lack of true vascular wall and is surrounded by connective tissue. Post angiographic iatrogenic pseudoaneurysms are becoming increasingly common due to increasing use of endovascular diagnostic and interventional procedures. The prevalence rates has been variously described in literature, ranging from approximately 0.2 to 5% [1,2]. If untreated, the pseudoaneurysms may cause various complications; the most dreaded being rupture [3-5]. Previously, open surgical repair was the gold standard of treatment. Ultrasound-guided (US) compression was introduced as a treatment option and more recently, US-guided percutaneous thrombin injection is becoming popular for treatment of pseudoaneurysms. However, there is lack of conclusive data to assess its relevants. The aim of this study was to evaluate safety and efficacy of this relatively new treatment option.
Materials and Methods
This study was undertaken at a tertiary care interventional and cardiology centre where interventional cardiology and radiology procedures are performed daily. This was a descriptive study based on retrospective analysis of cases and included 38 patients who underwent treatment of iatrogenic pseudoaneurysms during the period from January 2013 to June 2016.
All these patients had undergone angiogram/ vascular intervention through femoral arterial access and were treated by US guided percutaneous thrombin injection. An approval of Institutional Ethics Committee was taken and an informed consent was taken from all these patients. No patient refused the procedure. Based on clinical suspicion, the patients underwent Doppler imaging which confirmed the diagnosis of pseuodaneurysm in all these cases.
The Procedure
The procedure was performed in the Doppler room/bedside under all the aseptic precautions. A Doppler scan was done with 5 MHz or 7.5 MHz transducer to confirm the pseudoaneurysm, locate its neck and target the part of pseudoaneurysm for thrombin injection. Before giving injection, any contraindications such as gross superficial infection, co-existent arteriovenous fistula and known severe allergic reaction to thrombin/other drugs were assessed. The assessment of distal flow was documented before injection by clinical (palpation of distal pulses) and radiological (Doppler flow characteristics) assessment.
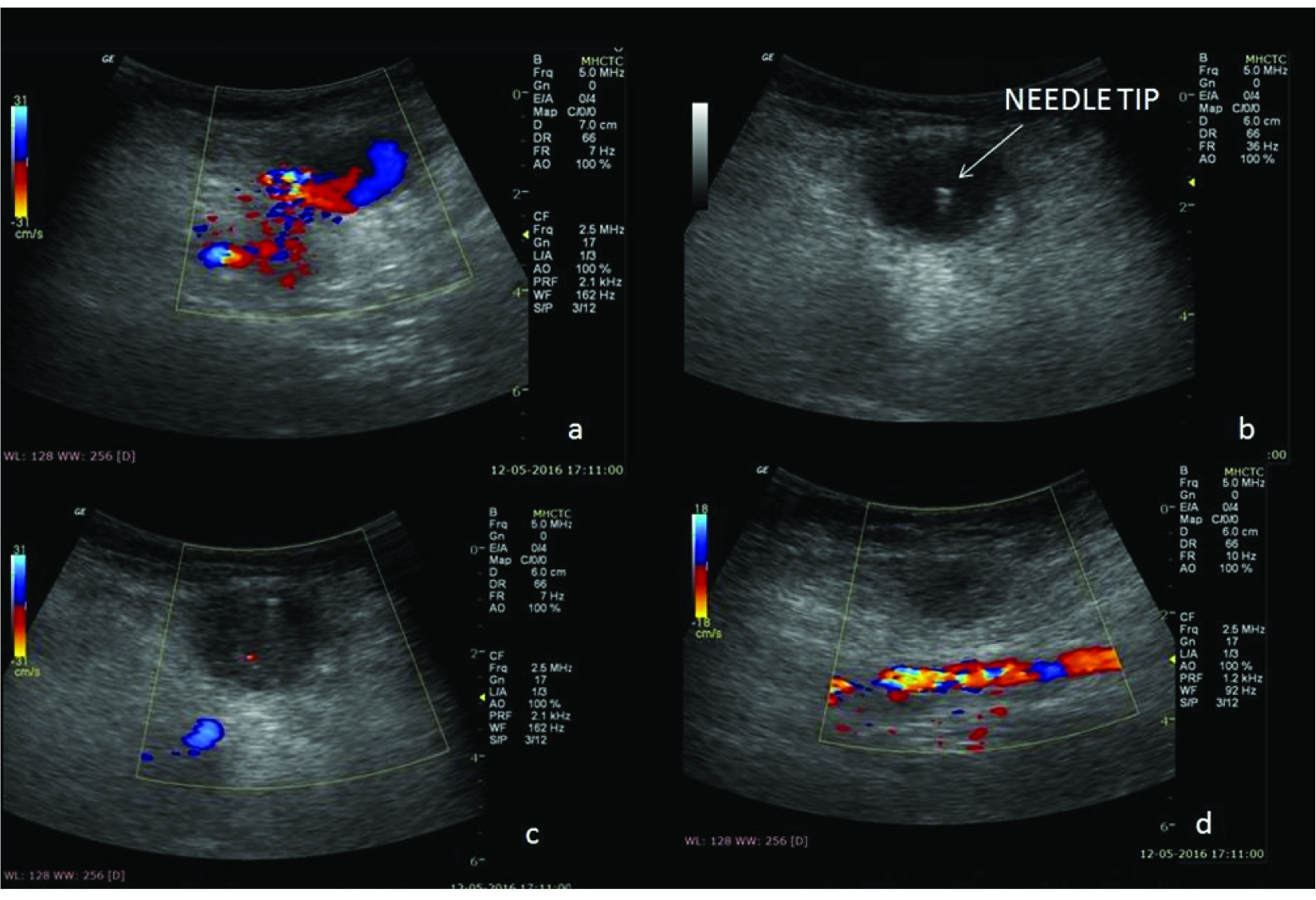
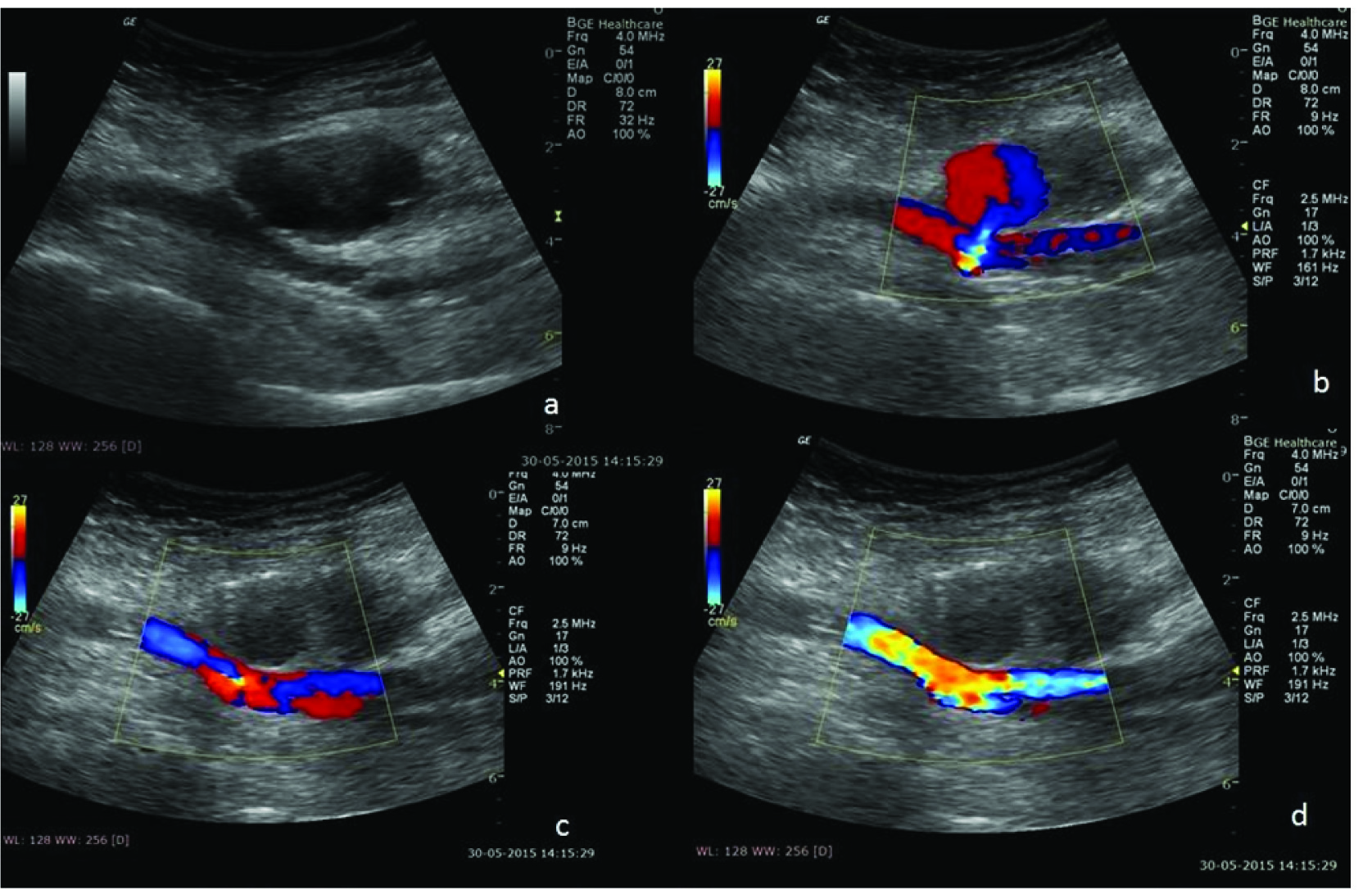
The thrombin solution used was either from the Reliseal (Reliance Life Sciences, Mumbai, India) or Tissel (Baxter, Gurgaon, India) kit. The thrombin solution had to be reconstituted before using the CaCl2 solution in the kit. The reconstituted solution had strength of 500 units of thrombin per ml. The reconstituted solution was drawn into a 1-ml syringe and the needle was changed to a 22G needle. After cleaning the local region, with an antiseptic (Betadine and alcohol), the tip of the needle was moved inside the sac of the pseudoaneurysm under US visualization. Thereafter, a small volume of thrombin solution was injected in incremental doses (0.1-0.2 ml) under image guidance. The appearance of sac (change from hypoechic to hyperechoic contents) and flow in the sac was checked on color Doppler US and if there was persistent flow in the sac, the injection was repeated till complete obliteration of flow in the sac was seen [Table/Fig-1,2]. Also, thrombin was injected in incremental small doses as mentioned above in order to avoid accidental injection into the femoral artery. In cases where neck was relatively short, manual compression of femoral artery superior to the pesudoaneurysm in neck was done by second operator to reduce to and fro flow into the pseudoaneurysm. This compression was maintained till contents of sac appeared completely echogenic and further for another 4-5 minutes to allow the thrombus to stabilize. The compression was then slowly released under real time US guidance. Doppler assessment was done for patency of underlying native artery and the peripheral blood flow was confirmed by Doppler assessment. Patients were advised bed rest for 6 hours post procedure. A follow up Doppler was then done after 24-48 hours. Patient was then called up for follow up after one month of the procedure when Doppler scan was repeated.
(a) Doppler image shows pseudoaneurysm communicating with underlying femoral artery; (b) Needle is then advanced inside the sac; Post thrombin injection images; (c,d) showing increased echogenicity inside the pseudoaneurysm (due to thrombus formation) and no flow within.
B-mode (a) and Doppler images (b) showing pseudoaneurysm communicating with underlying femoral artery. Post procedure images (c, d) showing increased echogenicity inside the pseudoaneurysm (due to thrombus formation) and no flow within.
Results
A total of 38 patients underwent the procedure from January 1, 2013 to June 30, 2016. The mean (±SD) age was 58 years ±12. Twenty two patients were males and 16 were females. The most common aetiology was femoral vascular access for coronary interventions [Table/Fig-3]. The arterial sheath used was 6F in 13 patients, 7F in 22 patients and 8F in 3 patients.
Aetiology of femoral pseudoaneurysm.
| Aetiology | n= 38 | % |
|---|
| Diagnostic coronary angiography | 12 | 38.7 |
| Coronary Interventions | 21 | 55.2 |
| Peripheral Angiograms | 1 | 2.6 |
| Peripheral interventions | 2 | 5.2 |
| Cerebral angiograms | 1 | 2.6 |
| Neuro-interventions | 1 | 2.6 |
The origin of the pseudoaneurysm was from the common femoral artery in 29 patients and superficial femoral artery in 9 patients. The aneurysm was unilobulated in 24 patients, bilobulated in 11 patients and more complex in 3 patients. The mean largest diameter of the pseudoaneurysm was 3.4 cm (range 1.8-4.1cm).
The mean volume of thrombin injected was 300 IU (range 200-1000 IU). Single session of thrombin injection was successful in 37 patients. One patient who had a residual sac, required second session after which it thrombosed completely. Immediate success was seen in 38 patients; early (24 hours) partial re-canalization was seen in one patient with large pseudoaneurysm who required second injection of thrombin [Table/Fig-4].
Outcome of the procedure (percutaneous thrombin injection).
| Outcome | n= 38 |
|---|
| Primary success | 37 |
| Early recurrence | 1 |
| Success after second injection | 1 |
| Complications | 0 |
The procedures were done without local anaesthesia and were associated with mild pain during and after procedure in all the patients. Two patients showed minimal extension of thrombus from the pseudoaneurysm into the underlying femoral artery on post procedure Doppler. However, no clinically detectable ischemic event happened in these patients and follow up Doppler showed clearance of thrombus from the femoral artery. No neuralgic symptoms or infection was noted in any of the cases.
Discussion
Vascular injury and iatrogenic pseudoaneurysms after percutaneous vascular interventions are one of the established complications. These are reported more often recently due to increase in interventional vascular procedures worldwide. The incidence is more in presence of underlying heavily calcific arteries, presence of underlying hypertension and aggressive post intervention heparinisation and when improper technique of puncture or compression is used [3,4]. Though small pseudoaneurysms may thrombose spontaneously [6,7], most of the pseudoaneurysms need to be treated because they can cause various complications, such as neuropathy, deep vein thrombosis or skin necrosis, progressive increase in size and more catastrophic rupture [4,5].
Surgical repair had been the primary recommended treatment for the pseudoaneurysms till the 1990s. However, it is an invasive procedure and is associated with morbidity and complications and requires relatively prolonged hospital stay [8]. Ultrasound and Doppler guided compression also gained popularity in the last two decades and has been shown to be a safe and cost-effective method for achieving pseudoaneurysm thrombosis [4,9,10]. However, it has disadvantages such as long procedure time, significant pain during compression, higher incidence of failure in large, complex pseudoaneurysms and higher recurrence rate in patients receiving anticoagulant therapy [11,12].
Ultrasound guided percutaneous injection of thrombin was first described in 1980s by Cope et al., [13]. The procedure started gaining popularity in only late 1990s after which various reports have been made describing it to be a simple and effective procedure [14-19]. The primary success rate in these studies varied from 93-100% and recurrence rates of 6-14 %. Pinton et al., mentioned in their study that the result of this technique in patients with Acute Coronary Syndrome (ACS) may be compromised by the use of concomitant anticoagulant and antithrombotic drugs [20]. The complication rate in various studies has also been low (1-2%) and included allergic reactions to bovine thrombin, distal embolism and neuralgic symptoms due to adjoining nerve compression.
In present study, the immediate (primary) success rate was 100%. Early recurrence was seen in only one patient (2.6%) who was successfully treated by second injection of thrombin. No clinically evident complications were there in any of the patients.
The present study thus strengthens the increasing evidence that the procedure is simple, safe and has highly successful clinical outcome. The procedure is an effective alternative to open surgical repair which may be avoided in most cases.
Limitation
The limitations of present study were relatively small sample size and retrospective nature of the study.
Conclusion
The study shows US-guided thrombin injection for femoral pseudoaneurysm treatment to be a safe, quick, painless and effective technique. It is simpler and more effective than US guided compression and has lesser complications and morbidity as compared to surgical treatment. Wherever feasible, US guided thrombin injection should therefore be the initial treatment of choice for femoral pseudoaneurysms.
[1]. Kresowik TF, Khoury MD, Miller BV, Winniford MD, Shamma AR, Sharp WJ, A prospective study of the incidence and natural history of femoral vascular complications after percutaneous transluminal coronary angioplastyJ Vasc Surg 1991 13:328-33. [Google Scholar]
[2]. Katzenschlager R, Ugurluoglu A, Ahmadi A, Hiilsmann M, Koppensteiner R, Larch E, Incidence of pseudoaneurysm after diagnostic and therapeutic angiographyRadiology 1995 195:463-66. [Google Scholar]
[3]. Messina LM, Brothers TE, Wakefield TW, Zelenock GB, Lindenauer SM, Greenfield LJ, Clinical characteristics and surgical management of vascular complications in patients undergoing cardiac catheterization: interventional versus diagnostic proceduresJ Vasc Surg 1991 13:593-600. [Google Scholar]
[4]. Fellmeth BD, Roberts AC, Bookstein JJ, Freischlag JA, Forsythe JR, Buckner NK, Postangiographic femoral artery injuries: nonsurgical repair with US-guided compressionRadiology 1991 178:671-75. [Google Scholar]
[5]. Kang SS, Labropoulos N, Mansour MA, Baker WH, Percutaneous ultrasound guided thrombin injection: a new method for treating postcatheterization femoral pseudoaneurysmsJ Vasc Surg 1998 27:1032-38. [Google Scholar]
[6]. Johns JP, Pupa Jr LE, Bailey SR, Spontaneous thrombosis of iatrogenic femoral artery pseudoaneurysms: documentation with color Doppler and two-dimensional ultrasonographyJ Vasc Surg 1991 14:24-29. [Google Scholar]
[7]. Rivers SP, Lee ES, Lyon RT, Monrad S, Hoffman T, Veith FJ, Successful conservative management of iatrogenic femoral arterial traumaAnn Vasc Surg 1992 6:45-49. [Google Scholar]
[8]. Lumsden AB, Miller JM, Kosinski AS, Allen RC, Dodson TF, Salam AA, A prospective evaluation of surgically treated groin complications following percutaneous cardiac proceduresAm Surg 1994 60:132-37. [Google Scholar]
[9]. Kumins NH, Landau DS, Montalvo J, Zasadzinski J, Wojciechowski J, Jovanovich BD, Expanded indications for the treatment of postcatheterization femoral pseudoaneurysms with ultrasound-guided compressionAm J Surg 1998 176:131-36. [Google Scholar]
[10]. Luedde M, Krumsdorf U, Zehelein J, Ivandic B, Dengler T, Katus HA, Treatment of iatrogenic femoral pseudoaneurysm by ultrasound-guided compression therapy and thrombin injectionAngiology 2007 58:435-39. [Google Scholar]
[11]. Stone PA, AbuRahma AF, Flaherty SK, Bates MC, Femoral pseudoaneurysmsVasc Endovascular Surg 2006 40:109-17. [Google Scholar]
[12]. Morgan R, Belli AM, Current treatment methods for postcatheterization pseudoaneurysmsJ Vasc Interv Radiol 2003 14:697-710. [Google Scholar]
[13]. Cope C, Zeit R, Coagulation of aneurysms by direct percutaneous thrombin injectionAJR Am J Roentgenol 1986 147:383-87. [Google Scholar]
[14]. Krueger K, Zaehringer M, Strohe D, Stuetzer H, Boecker J, Lackner K, Postcatheterization pseudoaneurysm: Results of US-guided percutaneous thrombin injection in 240 patientsRadiology 2005 236:1104-10. [Google Scholar]
[15]. Schneider C, Malisius R, Kuchler R, Lampe F, Krause K, Bahhnann E, A prospective study on ultrasound-guided percutaneous thrombin injection for treatment of iatrogenic post-catheterisation femoral pseudoaneurysmsInt J Cardiol 2009 131:356-61. [Google Scholar]
[16]. Khoury M, Rebecca A, Greene K, Rama K, Colaiuta E, Flynn L, Duplex scanning-guided thrombin injection for the treatment of iatrogenic pseudoaneurysmsJ Vasc Surg 2002 35:517-21. [Google Scholar]
[17]. Grewe PH, Mugge A, Germing A, Harrer E, Baberg H, Hanefeld C, Occlusion of pseudoaneurysms using human or bovine thrombin using contrast-enhanced ultrasound guidanceAm J Cardiol 2004 93:1540-42. [Google Scholar]
[18]. Sheiman RG, Mastromatteo M, Iatrogenic femoral pseudoaneurysms that are unresponsive to percutaneous thrombin injection: Potential causesAJR Am J Roentgenol 2003 181:1301-04. [Google Scholar]
[19]. Calton WC Jr, Franklin DP, Elmore JR, Han DC, Ultrasound-guided thrombin injection is a safe and durable treatment for femoral pseudoaneurysmsVasc Surg 2001 35:379-83. [Google Scholar]
[20]. Pinton FA, Spósito AR, de Andrade Vahle V, Soares PR, Zalc S, Perin MA, Ultrasound-guided thrombin injection in the treatment of femoral artery pseudoaneurysm after percutaneous procedures in patients with acute coronary syndromeRevista Brasileira de Cardiologia Invasiva (English Edition) 2013 21(1):18-22. [Google Scholar]