Posterior ethmoid and sphenoid sinuses are grouped as posterior paranasal sinuses. These sinuses show various degrees of pneumatization and so does the ONC relation. The most common position of the ONC with the sphenoid sinus is superolateral position [1]. Depending on the degree of the sinus pneumatization, varied protrusion of ONC into the sinuses may occur. Occasionally, it may completely pass through the sinus. ON may be covered by a thin bony layer or without bone by periosteum & sinus mucosa. Injury to the optic nerve may occur due to extensive pneumatization and when the nerve lacks the supporting surrounding structures. The posterior ethmoid cell namely the Onodi cell is of great surgical importance when the optic nerve is along its lateral wall and surrounds the nerve [2]. These varied relations imply that a detailed knowledge of the intimate relationship of ONC with the posterior paranasal sinuses is necessary to avoid unintentional complications during the endoscopic sinus surgery.
It is generally known that skull shape varies in different ethnic groups and so the paransal sinus pneumatization. Hence we need to understand these variations in sinus pneumatisation and ONC relation pattern in our population.
The aim of the study was to assess relationship of ONC to the posterior paranasal sinuses in our study group of Indians, comprising mixture of Indo-Aryans and Dravidians of varied linguistic subgroups.
Materials and Methods
Hundred CT scans of paranasal sinuses were reviewed retrospectively, from April 2014 to March 2016. Scans were acquired on 64 rows MDCT on helically mode employing default 0.65 mm slice thickness, 120 kV and Auto mAs. Multiplanar reconstructions were analysed on a dedicated workstation. Scans of 18 to 67 year subjects were included in the study.
Total 200 ONCs were evaluated for their relationship with posterior paranasal sinuses. Two radiologists interpreted the images independently with blind folding of the results. The results were corroborated subsequently with both agreeing upon the nerve types in grey zones. Absent bony layer between the nerve and sinus was considered as dehiscence. Less than or more than 50% circumferential ON protrusion, and the presence of Onodi cells were considered to redefine the ONC types. Presence of dehiscence and pneumatization of anterior clinoid process were estimated separately. Statistical analysis was performed using specialized statistical software (SPSS package ver 10.5). Chi-square test was used and a p-value less than 0.05 was considered to be statistically significant.
Optic nerve canals were categorized into four Types [Table/Fig-1] by our classification system based on improvisation of Delano et al., classification [3]. In Type-1 canal there is no protrusion of optic nerve into the canal [Table/Fig-2]. Degree of optic nerve protrusion into the canal was taken into consideration for better objective classification of Type-2 and Type-3 canals [Table/Fig-3,4]. Type-4 canal is posteriorly displaced in ethmoidal air cell (Onodi cell or spheno–ethmoidal air cell), projecting superolateral to sphenoid sinus and forming medial boundary of optic nerve canal. In this type the optic nerve is in close relationship with ethmoid cell [Table/Fig-5].
Our Institute classification of ONC based on Delano et al., classification – “Sagar Classification”.
| Type of ONC | Description |
|---|
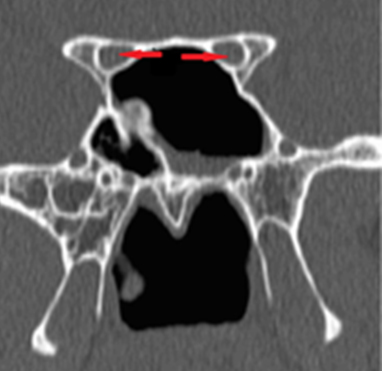
| 1 | Canal superolateral to the sphenoid sinus without indentation on the sinus wall on coronal CT sections [Table/Fig-2]. |
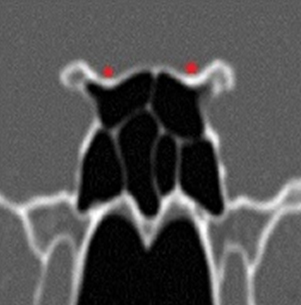
| 2 | Indentation on sphenoid sinus contour with less than 50% protrusion of nerve circumference on coronal view [Table/Fig-3]. |
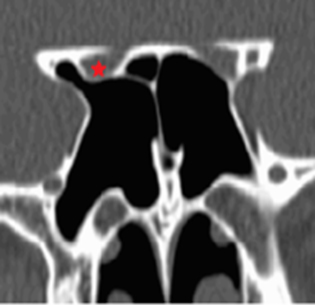
| 3 | Optic nerve traversing through sphenoid sinus with coronal view showing more than 50% protrusion of nerve circumference into sinus [Table/Fig-4]. |
| 4 | Canal is adjacent to sphenoid and posterior ethmoid sinuses/presence of Onodi cell [Table/Fig-5]. |
Coronal CT section showing bilateral Type-1 ONC (red arrows) without indentation on the sinus wall;
Coronal CT section showing Type-2 ONC on both sides (red asterisk) with optic nerve protrusion of less than half of its circumference into the sinus.
Coronal CT section showing Type-3 ONC on right side (red asterisk) with more than half of the circumference of the optic nerve protruding into the sinus;
Coronal CT section showing the presence of Onodi cells (white asterisk) representing Type-4 ONC.

Results
Two hundred optic nerve canals among 100 subjects including 66 males and 34 females were assessed. A total of 72 of them had sinusitis radiologically. Our study group result for ON types is shown in [Table/Fig-6]. Type-1 ONC was the most common of all and seen in 60%. Followed by Type-2 ONC in 15%, and Type-3 ONC in 14%. Type-4 ONC were noted in 11%. The canals were fairly similar in type on both sides in any particular subject, except in 8 subjects (16 sides) showing difference in types.
Prevalence of ONC types in the study group.
| Type of ONC | Right | Left | Total | Percentage |
|---|
| 1 | 59 | 61 | 120 | 60% |
| 2 | 16 | 14 | 30 | 15% |
| 3 | 15 | 13 | 28 | 14% |
| 4 | 10 | 12 | 22 | 11% |
Dehiscence was defined as absent bony coverage over the ON [Table/Fig-4]. There were 12 ONC which were dehiscent on right side, 11 on the left side and 12 bilaterally making a total of 35(17.5%). Bony dehiscence was also calculated for each ONC type separately [Table/Fig-7]. Dehiscence was seen in 64.3% of Type-3 canals, in 33.3% of Type-2 canals and in 27% of Type-4 canals. Dehiscence was very uncommon in Type-1 canals seen in only 0.8%. It is evident that dehiscence is very common in Type-3 canals, followed by Type-2 canals and least common in Type-1 canals. Out of 35 dehiscent ONCs, 13 were in females (38.3%) and the 22 were in males (33.3%). There is no sex predilection for dehiscence.
Prevalence of bony dehiscence and PACP in respective ONC types and total prevalence.
| ONC Type | Number of canals | BoneDehiscence | % of bone dehiscence | PACP | % of PACP |
|---|
| 1 | 120 | 1 | 0.8% | 0 | 0% |
| 2 | 30 | 10 | 33.3% | 2 | 7% |
| 3 | 28 | 18 | 64.3% | 26 | 93% |
| 4 | 22 | 6 | 27% | 2 | 9% |
| Total | 200 | 35 | 17.5% | 30 | 15% |
Pneumatization of anterior cliniod processes [Table/Fig-7] was seen in 30 canals [Table/Fig-8]. It was seen bilaterally in 8 subjects, only on right side in 8 subjects and only on left side in 6 subjects. It was observed that 93% of Type-3 canals were associated with PACP and only 7% of Type-2 canals and 9% of Type-4 canals had PACP. No PACP was seen in Type-1 canals. The frequency of PACP is statistically significant in Type-3 ONC with p-value < 0.0001
Coronal CT section showing pneumatization of bilateral anterior clinoid processes (red arrows) and bony dehiscence of the optic canal on right side (yellow arrow).

Discussion
CT of paranasal sinus is the best technique to evaluate a living subject’s morphology to assess the morphological relationship of ONCs to posterior ethmoid and sphenoid sinuses. It is important to know the relation of ON to these sinuses to prevent any complication during sinus surgeries. Damage to the ON is one of the major complications of endoscopic sinus surgeries. The ON, as they course medially towards the optic chiasma, tends to bulge into the lumen of the sphenoid sinus for varying extent. The ON is usually protected by the bony covering of sphenoid greater wing [2].
Another important risk factor is the excessive pneumatization of sphenoid sinus which can extend into the adjacent structures including anterior and posterior clinoid processes and pterygoid process. Excessive aeration of the sphenoid and surrounding structures can lead to the indentation of ONC into the sphenoid sinus and bony dehiscence. Increased pneumatization of posterior ethmoidal air cells may form part of boundary of ONC (Onodi cell) and may predispose to injury during Funtional Endoscopic Sinus Surgery (FESS) [3]. Size of the sphenoid sinus volume is also taken into consideration in endoscopic surgeries as the surgeons should be cautious as high sphenoid sinus volume is a predisposing factor for optic nerve injury [4].
Delano et al., classified the relation of ONC to the posterior ethmoid and sphenoid sinus into four categories [3]. In this classification Type-1 was the most common variety in which the ON courses adjacent to the sphenoid cell without indentation on the wall or contact with the posterior ethmoid sinuses. Type-2 nerves course adjacent to the sphenoid sinuses, with indentation of the sinus wall, without contacting any posterior ethmoid cell. Type-3 nerves course through the sphenoid sinus. Type-4 nerves course immediately adjacent to sphenoid and posterior ethmoid cells (presence of Onodi cell) [3]. In our study, Delano’s classification was modified with a better objective criteria. The first and the fourth type are similar to Delano’s categories, whereas, our Type-2 and Type-3 ONC were classified depending on the degree of projection into sphenoid sinus as less than 50% of circumference or more than 50% respectively [Table/Fig-1]. Coronal reformatted CT images were considered to define these variations [Table/Fig-2]. In Delano et al., classification, Type-1 ONC occurred in 76% of patients. In our study too, Type-1 ONC was the most common with 60% prevalence. In Delano study, 15% showed Type-2, 6% showed Type-3 and Type-4 among 3% [3]. Our study found that Type-2 and Type-3 ONCs to be almost equally prevalent with marginally more common Type-2. However, Type-4 ONC (11%) prevalence in our study was higher compared to Delano et al., Greater degree of protrusion is seen in Type-3 than Type-2 which indicated Type-3 is more dangerous than Type-2 ON. Higher prevalence of bony dehiscence was also seen in Type-3 ONC in our study.
As the optic nerve traverses through the sphenoid sinus, the optic nerves tend to be more exposed without bony covering. Delano also found that likelihood of bony dehiscence is high whenever there is more indentation on the lateral wall of the sphenoid sinus by ONC [3]. Manipulation of ONC during sinus surgery may result in Optic Nerve injury [5]. Dessi et al., defined protrusion as more than 50% circumferential ONC bulge into the sphenoid sinus on the coronal sections which pose the high risk for surgery [6].
Onodi cell, defined by Rice and Schaefer and Lang, is a posterior ethmoid cell which is in contact with the ON medially, superiorly and inferiorly [5]. Onodi cell has also been specified as sphenoethmoidal cell [7]. Occasionally, these cells may completely encircle the ON. Our study showed presence of Onodi cells in 22 canals. The presence of these Onodi cells is best seen on axial sections by tracing the ON beyond the orbital apex. Onodi cells increases the likelihood of ON as well as internal carotid artery injury during the sinus surgery [7-9].
PACP limits the superior course of ON and may cause medial displacement of ON indicating the vulnerability during endoscopic sinus surgeries. PACP forms a small space on the lateral wall of sphenoid sinus between the optic canal superiorly and the carotid prominence inferiorly which is known as opticocarotid recess. This may result in ON protrusion into the sphenoid sinus [10]. PACP is often associated with Type-2 and Type-3 ON and also with bony dehiscence [2]. Our study showed PACP prevalence in 15%, very commonly associated with Type-3 ONC (in 93%), less commonly associated with Type-4 and Type-2 ONC.
Cadaveric dissection studies have been carried out on paranasal sinuses. Manisha et al., in their study found optic nerve bulging in 10% of cadaver dissesctions, whereas prior CT scan in the same cadavers showed 35.6% protrusions and 30.6% dehiscence of optic nerves [11]. Further they also observed that CT is more sensitive than cadaveric dissection for evaluation of pneumatisation of anterior clinoid process [11]. Girish M et al., in their study of imaging of paranasal sinuses found that although CT is ideal for assessing the osseous margins of paranasal sinuses, MRI is superior for assessment of soft tissue masses and extension of infectious/malignant disease processes beyond the paranasal sinuses [12]. Less sample size is a limitation of the present study.
Conclusion
CT scan is the best tool to assess ONC relation to posterior paranasal sinuses, as it can demonstrate bone, soft tissue, air and accurately depict the anatomy. Our classification of ONCs defines Type-2 and Type-3 canals more objectively. Though sample size is limited in comparison to huge Indian population, albeit Type-1 canal was found to be most common in our study group of Indians, as elsewhere in world. Similarly, Type-2 and Type-3 are less common, with Type-2 canals slightly more common among the Indians. Type-4 canal are very uncommon. Type-3 ONC shows greater degree of protrusion, more prevalence of dehiscence and high association with PACP making it highly prone for surgical injury. Existence of PACP, Onodi cell and bone dehiscence are the dangerous anatomic variations which predispose to the iatrogenic ON injury.