Thromboangitis Obliterans involving Bilateral Upper limb Extremities - A Rare Case Report from Malaysia
Uthamalingam Murali1, Mohammad Azhar Anis Ahmad2, Fatin Najihah3
1 Professor, Department of Surgery, IMS / Management and Science University, Shah Alam, Selangor, Malaysia.
2 Specialist, Department of Surgery, HTAR - Hospital, Shah Alam, Selangor, Malaysia.
3 Student, Department of Surgery, IMS / Management and Science University, Shah Alam, Selangor, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Uthamalingam Murali, Professor, Department of Surgery, International Medical School, Management and Science University, Malaysia, Shah alam-40150, Selangor, Malaysia.
E-mail: srimuralihospital2012@gmail.com
Thromboangitis Obliterans (TAO) or Buerger’s disease is a non-atherosclerotic, occlusive, progressive and highly inflammatory disorder of distal arteries seen predominantly affecting the lower limb in smokers. TAO presenting itself in upper limb or bilaterally involving the upper limb is a very rare entity. We report on a rare case of TAO in a 46-year-old gentleman who presented with bilateral upper extremity digital gangrene with 18 pack-years of smoking. Brachial and radial pulses were palpable bilaterally and were of good volume but right ulnar pulse was faintly felt, while on the left side it was not appreciated due to malunion. Further Computed Tomography (CT)- angiography showed occlusion of distal right ulnar artery, stenosis of distal left ulnar artery with bilateral poor opacification of palmar and digital arteries. This case reports on the unusual and rare presentation of TAO in upper extremity involving both limbs. The case is reported for the first time from Malaysia.
Blackish patchy lesion peripheral pulses, Middle and Index finger, Smoking, Ultrasound doppler, Upper extremity
Case Report
A 46-year-old male presented to the department of surgery with gangrene involving the digits of bilateral upper extremities. He experienced his first episode of fingertip rest pain with multiple blackish discoloration of right middle finger two months prior to his presentation. The pain was progressively worsened, associated with coldness of fingers and numbness of the hand. He also noticed limitation in movements but denied of any bluish discoloration of digits and the pain was not related with coldness. He consulted a local doctor and was prescribed analgesics, Non-Steroidal Anti-Inflammatory (NSAID’s) and broad spectrum antibiotics for his ailment, which made him pain free for quite some time.
However, the blackish discoloration continued to spread further involving the palmar and dorsal aspect of right middle finger extending to the proximal phalanx. He continued tobacco usage and subsequently developed similar episode of rest pain with blackish discoloration of his left index finger two weeks prior to his presentation. He denied of similar complaints over the other fingers as well as both legs and toes. No other symptoms were noted.
He was not suffering from any other co-morbidity such as diabetes or hypertension. He was a chronic and aggressive smoker for more than 20 years with 18 pack-year and an occasional alcohol consumer.
Clinical examination revealed dry gangrenous changes over right middle finger extending from proximal inter-phalangeal joint to the tip of finger with thinning out of distal phalanx and atrophy of the nail [Table/Fig-1]. Proximal to the line of demarcation of gangrene the skin appeared erythematous with diffuse swelling up to the Metacarpo-Phalangeal Joint (MCP) joint. Over the left index finger, 0.5 cmx0.5 cm size patch lesion with blackish discoloration was noted [Table/Fig-2]. Multiple small dotted spotty blackish lesions were seen bilaterally over the rest of the fingers. All fingers were cold, up to the level of distal inter-phalangeal joint except for right middle finger. Sensation was absent over the gangrenous area while the same in other fingers was intact. Brachial and radial pulses were palpable bilaterally and were of good volume, but right ulnar pulse was faintly felt, while left was not appreciated due to malunion. Lower limb examination was unremarkable. His physical examination including the vital signs and other organ system (CVS, CNS, and GIT) evaluation was normal.
Dry gangrene – right middle finger.

Black patchy lesion – left middle finger.

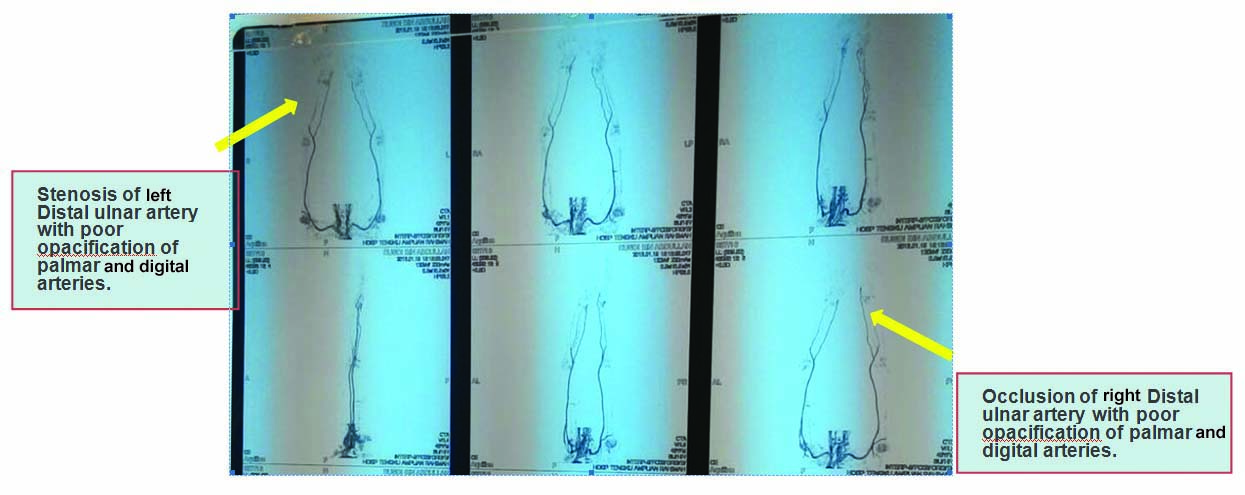
With the diagnosis of upper limb ischemia due to TAO the patient was investigated. His blood investigations were within normal limits. Echocardiogram showed an ejection fraction of 74%. Later the systolic pressure differences in all four limbs were recorded to calculate Ankle Brachial Pressure Index (ABPI), which signifies the nature of ischemia. The ABPI results revealed a total of 1.12 (upper limb: 138 mmHg, Lower limb 148 mmHg) for right extremities and 1.40 (upper limb: 100 mmHg, lower limb: 140 mmHg) for left extremities showing the vascular patency of lower limb. This was further assessed using ultrasound Doppler. Further CT- angiography showed occlusion of distal right ulnar artery, stenosis of distal left ulnar artery with bilateral poor opacification of palmar and digital arteries [Table/Fig-3].
CT angiography showing stenosis of left distal ulnar artery palmar and digital arteries and occlusion of right distal ulnar artery.
He was strongly advised to stop smoking and was treated with vasodilators such as nifedepine 10 mg twice a day, antiplatelet drug such as low dose aspirin-75 mg once a day and statins such as simvastatin-20 mg twice a day. While during hospital stay, certain improvement of patchy lesions of the left digits were seen after he stopped smoking and with the conservative treatment offered. As no surgical intervention facilities were available in current hospital, the patient was referred for further evaluation to vascular team of other hospital. Further follow up of the patient was not done.
Discussion
TAO or Buerger’s disease is a non-atherosclerotic, occlusive, progressive, often segmental and highly inflammatory disorder of small arteries and veins with unknown aetiology, seen predominantly affecting the extremities in smokers [1]. However, studies have shown TAO of lower extremity are much more common than upper extremity [2]. Even though TAO commonly involves the extremities, certain reports show the disease process to affect other sites (such as aorta, cerebral, coronary and intestinal arteries) as well [3]. It is more common in Eastern countries like Middle-East, Asia and South-East Asia compared to Western countries such as United Kingdom and United States [4]. However, the incidence of TAO in upper extremity is rare as compared to lower, the treatment aspect of upper limb TAO is also difficult compared to lower limb. Hence TAO in upper limb or bilaterally involving the upper limb is a very rare entity. This is the first reported case of TAO involving bilateral upper extremities from Malaysia.
The disease is exclusively seen in males aged 40 to 50 years and less seen in women due to genetic reason [5,6] as in our case. But certain studies have reported the male-to-female ratio and age group, considering TAO is changing with an increased incidence in females and also more number of older patients [6]. Although, the aetiology is unknown, Buerger’s disease is a potential complication of chronic smoking, cannabis and tobacco usage in young adults. Autoimmune mechanism, genetic predisposition, immunoglobulin and complement factors have been reported to be associated with the pathogenesis of TAO [5].
Many diagnostic criteria are available to diagnose TAO [7]. Popular among these are the Shionoya and Olin criteria [8,9]. The criteria to diagnose TAO is based upon history of smoking in men of less than 50 years of age with or without thrombophlebitis and involvement of upper or lower extremity without diabetic, hyperlipidemia or thrombo-embolic features [7–9]. The diagnosis of TAO can be made, when patient meets most of the above criteria. The presented case met most of these criteria. However, this criterion is not accepted globally [7].
Studies have shown higher prevalence of ischemic ulcer, paraesthesia with claudication and rest pain in TAO patients with lower prevalence of Raynaud’s phenomenon and thrombophlebitis [2,8]. This was applicable to our case as the patient denied relation to coldness and bluish discoloration. Most literature’s report an incidence of TAO affecting the lower extremity (75%-90%) followed by both upper and lower extremities (10%-20%) with only 2%-5% affecting upper extremity [2,6,10]. No randomized trials or prospective studies were identified with regards to upper limb ischemia. Hence, our case is very rare entity in its presentation.
Although, autoimmune mechanism is considered as one of the aetiological factor, no serological markers or positive diagnostic tests, neither biopsy are available to diagnose TAO [4,7]. However, many criteria along with ABI measurements using Doppler study could often reveal the preliminary diagnosis of limb ischemia due to TAO, echocardiography and CT angiography are the diagnostic method to exclude proximal source of emboli and to confirm the site of lesion either in upper or lower extremity as in our case [6]. Studies have reported that the findings of angiography are helpful but not pathognomonic of the disease [7].
Various medical and surgical treatment options have been proposed in treating TAO but the initial option should be of conservative management. Several studies have shown that no forms of therapy are definitive in stopping the progression of disease until the patients do abstain from smoking [7,11], similar to our case. Medical treatment includes vasodilators and antiplatelet drugs which bring about total relief of pain at rest but the long-term benefit and improvement in quality of life is limited. Surgical treatment may improve the peripheral blood flow whereby promoting healing of the lesions and preventing amputations. [11]. So this type of conservative treatment was effective in certain lesions in our case until he was referred. Later the patient was referred to the vascular team of Hospital Kuala Lumpur (HKL), referral center for vascular problems for further evaluation and management. The final results of treatment measures offered to the patient could not be assessed as we could not follow up the patient.
Conclusion
TAO involving bilateral upper extremity according to the criteria is being reported for the first time from Malaysia. The occurrence of thrombophlebitis and Raynaud’s phenomenon were rather infrequent in the presented case. CT-angiography was the key diagnostic method to confirm the exact site of lesion in guiding the proper management. Abstinence from smoking stopped the progression of the disease in the initial stages of the conservative management of TAO. Proper and accurate referral to vascular center will help in saving the limb and the patient as in our case.
[1]. Robert Sayers, Arterial disorders. In: Williams NS, Bulstrode CJK and Ronan O’Connell P(Ed)Bailey and Love’s Short Practice of Surgery 2013 26th editionBoca Raton, LondonCRC Press:877-900. [Google Scholar]
[2]. Javed S, Hasan T, Ahmad S, Hadi G, Gholamreza H, Amir-ali M, Clinical characteristics of buerger’s disease in IranJ Col Phy Surg Pak 2008 18(8):502-05. [Google Scholar]
[3]. Harten P, Muller-Huelsbeck S, Regensburger D, Loeffler H, Multiple organ manifestations in thromboangiitis obliterans (Buerger’s disease). A case reportAngiology 1996 47:419-25. [Google Scholar]
[4]. Arkkila PE, Thromboangiitis obliterans (Buerger’s disease)Orph J Rare Dis 2006 01:14 [Google Scholar]
[5]. Chochola M, Márová K, Linhart A, Buerger’s diseaseCas Lek Cesk 2006 145:358-62. [Google Scholar]
[6]. Joviliano EE, Dellalibera-Joviliano R, Dalio M, Évora PR, Piccinato CE, Etiopathogenesis, clinical diagnosis and treatment of thromboangiitis obliterans- current practicesInt J Ang 2009 18(3):119-25. [Google Scholar]
[7]. Lazarides MK, Georgiadis GS, Papas TT, Nikolopoulos ES, Diagnostic criteria and treatment of Buerger’s disease: A reviewInt J Low Extrem Wounds 2006 5(2):89-95. [Google Scholar]
[8]. Shionoya S, Diagnostic criteria of Buerger’s diseaseInt J Cardiol 1998 66(1):243-45. [Google Scholar]
[9]. Olin JW, Young JR, Graor RA, Ruschhaupt WF, Bartholomew JR, The changing clinical spectrum of thromboangiitis obliterans. (Buerger’s disease)Circulation 1990 82(5):03-08. [Google Scholar]
[10]. Sasaki S, Sakuma M, Kunihara T, Yasuda K, Distribution of arterial involvement in thromboangiitis obliterans (Buerger’s disease): results of a study conducted by the intractable vasculitis syndromes research group in JapanSurgery Today 2000 30(7):600-05. [Google Scholar]
[11]. Vijayakumar A, Tiwari R, Prabhuswamy VK, Thromboangiitis obliterans (Buerger’s Disease)-Current PracticesInt J Infn 2013 :01-09. [Google Scholar]