Efficacy of Structured Yoga Intervention for Sleep, Gastrointestinal and Behaviour Problems of ASD Children: An Exploratory Study
Kumar Narasingharao1, Balaram Pradhan2, Janardhana Navaneetham3
1 Research Scholar, Department of Yoga and Humanities, S-VYASA University, Bengaluru, Karnataka, India.
2 Assistant Registrar, Department of Academics, S-Vyasa University, Bengaluru, Karnataka, India.
3 Associate Professor, Department of Psychiatric Social Work, NIMHANS, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kumar Narasingharao, # 974, ITI Layout, 2nd Cross, Papareddypalya, Near Old Outer Ring Road, Nagarabhavi 2nd Stage, Bengaluru-560072, Karnataka, India.
E-mail: nknrao2007@gmail.com
Introduction
Autism Spectrum Disorder (ASD) is a neuro developmental disorder which appears at early childhood age between 18 and 36 months. Apart from behaviour problems ASD children also suffer from sleep and Gastrointestinal (GI) problems. Major behaviour problems of ASD children are lack of social communication and interaction, less attention span, repetitive and restrictive behaviour, lack of eye to eye contact, aggressive and self-injurious behaviours, sensory integration problems, motor problems, deficiency in academic activities, anxiety and depression etc. Our hypothesis is that structured yoga intervention will brings significant changes in the problems of ASD children.
Aim
The aim of this study was to find out efficacy of structured yoga intervention for sleep problems, gastrointestinal problems and behaviour problems of ASD children.
Materials and Methods
It was an exploratory study with pre-test and post-test control design. Three sets of questionnaires having 61 questions developed by researchers were used to collect data pre and post yoga intervention. Questionnaires were based on three problematic areas of ASD children as mentioned above and were administered to parents by teachers under the supervision of researcher and clinical psychologists. Experimental group was given yoga intervention for a period of 90 days and control group continued with school curriculum.
Results
Both children and parents participated in this intervention. Significant changes were seen post yoga intervention in three areas of problems as mentioned above. Statistical analysis also showed significance value of 0.001 in the result.
Conclusion
Structured yoga intervention can be conducted for a large group of ASD children with parent’s involvement. Yoga can be used as alternative therapy to reduce the severity of symptoms of ASD children.
Anxiety, Attention, Depression, Physiological, Psychological, Sameness, Social communication
Introduction
ASD is a complex neuro developmental disorder which manifest at early childhood age between 18 and 36 months [1]. ASD symptoms remains throughout life span of an individual unless an early and proper intervention is provided [2]. ASD children are categorized as verbal and non-verbal who suffer from impaired language like initiating communication, use of inappropriate words and repetitive language, non-compliance, irritability, learning disability, etc. Most of the children suffer from disturbed sleep due to not following routine bed time like going to bed in the night and getting up from bed in the morning, awaking in between sleep, snoring and breathing from mouth during sleep etc., which also influences different behavioural problems [3]. ASD children with GI problems may suffer from different digestion problems like bloating, food intolerance, inflammation in intestinal tract, irritable bowel syndrome, diarrhoea, flatulence, urine and faecal incontinence problems, etc., [4]. Autism is one among spectrum disorders, others being Asperger’s syndrome, pervasive Developmental Disorder- Not Otherwise Specified (PDD-NOD), Rett’s syndrome and childhood disintegrative [5]. Autism children suffer from multiple deficiencies in social communication and interaction, social skills, repetitive and restrictive behaviour, attention deficit, sensory integration problems, motor problems, aggressive or self-injurious behaviour, self-stimulation (finger flapping or head movement), lacking in academic activities etc. ASD children are also prone to anxiety and depression (psychiatric disorder) which deters them to mingle or interact with other children of their age [6]. Children face difficulty in initiating peer communication and may exhibit repetitive motor behaviour [7]. In 1940s, Kanner first identified a group of children who were totally different from other normal children - studied and published a paper on their behaviour pattern [8]. Traditionally it is considered a disorder without any specific cure from pharmacological medicine or with a very few biomedical intervention [9]. Identifying at early age of childhood and giving proper intervention can prevent long term negative effect on ASD children [10].
It is known that an individual with autism has higher comorbidity burden than the general paediatric population with higher rate of psychiatric illness, seizures and GI disorder [11,12]. ASD children who suffer from persistent GI problems may not respond to any type of behavioural intervention unless GI problems resolved [13]. According to recent studies up to 80% of the ASD children suffer from sleep and gastrointestinal dysfunction which is not well understood by parents [14,15]. Prevalence of autism remained as high as one in 68 children between 2010 to 2016 period in US according to CDC report 2016 [16]. Causative factor can be due to environment, genetic factors, family history of having ASD children previously, older age of mother or father, due to single gene defect, family history of immune associated conditions such as thyroid disease or rheumatoid arthritis, or due to pregnancy related complications [17].
Complementary and alternative medical treatment or therapies like yoga is most commonly used for ASD children [18]. Yoga found to bring positive effect on both physical and mental level as well as useful for neuro-behavioural problems [19,20]. Yoga is being used as an effective therapy in mental health [21]. In this study we are testing efficacy of structured yoga intervention for sleep, gastrointestinal and behaviour problems of ASD children.
Materials and Methods
This was an exploratory study with pre-test and post-test control design arranged by school authorities to encourage parents and teachers participation. Academy for Severe Handicap and Autism (ASHA) a special school for differently abled children with assessment, training and guidance centre. The study was conducted from January 2016 to April 2016 for a period of three months continuously between 9.30 am to 10.45 am. Project was approved by the Institutional Ethics Committee of Swami Vivekananda Yoga Anusandhana Samsthana, Bengaluru (IEC SVYASA). Sample size was as per the IEC guideline which stipulated not less than 30 each group (n=60 for two groups combined) for this study {IEC Ref: RES/IEC-SVYASA/56/2015}.
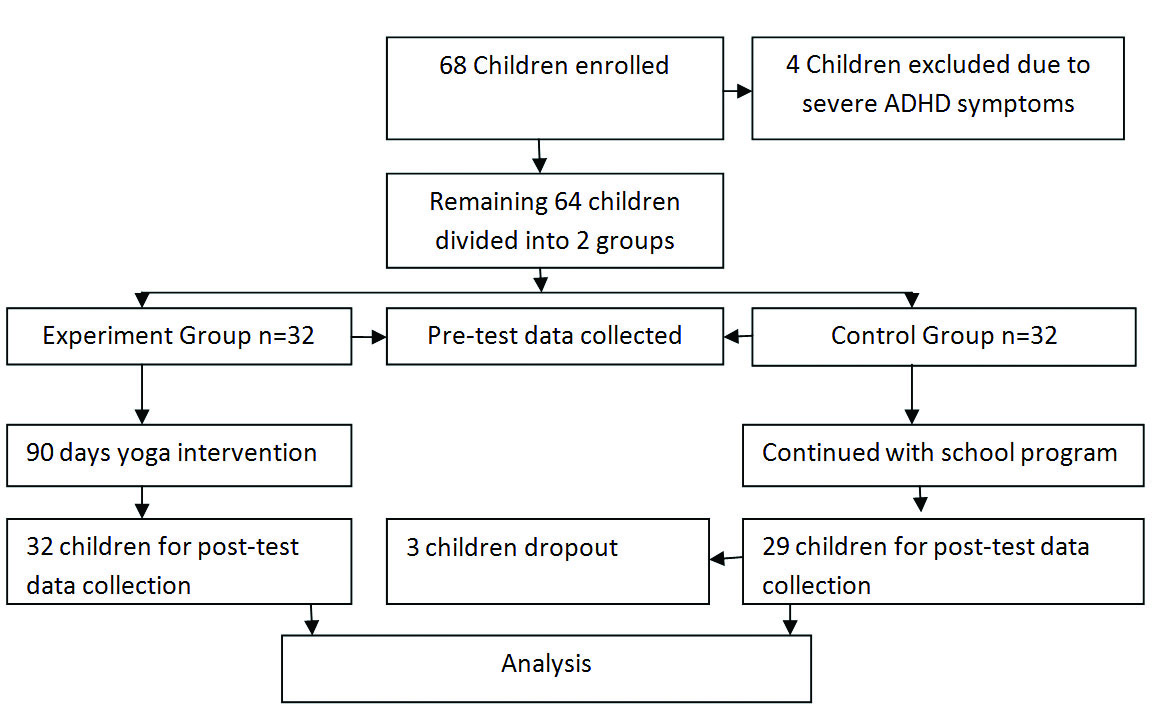
A total of 68 children were recruited between the age group 5-16 years. Both male and female children were considered and one of the parents who agreed to participate with children only selected for this program. Four children were excluded from the group due to Attention Deficit and Hyperactive Disorder (ADHD) symptoms. Children were previously diagnosed as autistic as per school records under the International Classification for Diseases, Tenth Edition [22]. Assent and consent forms were signed by the participant, parents and teachers wherever applicable. Children with severe physical problems or other serious health problems were excluded from this study. The process was as per chart shown in [Table/Fig-1] below.
A sixty one item questionnaires developed by researchers based on the problematic area of ASD children were administered to parents’ pre and post yoga intervention by teachers under the guidance of clinical psychologist and researcher. Questions included sleep disorder 15 questions (SQ1-SQ15) [Table/Fig-2], GI disorder (food and digestion) 16 question (FQ1-FQ16) [Table/Fig-3] and behaviour problems 30 questions (BQ1-BQ30) [Table/Fig-4]. A yoga therapist having master’s degree in yoga therapy with several years of teaching experience was appointed to teach yoga to the children.
| Questionnaire for ParentsName of the Child:_____________________________________________________SECTION-I: SLEEP |
|---|
| S.N. | STATEMENT | Agree | Rarely | Some times | Disagree | Strongly disagree |
|---|
| | 1 | 2 | 3 | 4 | 5 |
|---|
| SQ-1 | Your child sleeps more than eight hours at a stretch in the night. | | | | | |
| SQ-2 | Your child does not sleep in the day time. | | | | | |
| SQ-3 | Your child’s behaviour will not change if do not sleep well in the night. | | | | | |
| SQ-4 | When others in the family go to bed, normally your child sleeps without much effort. | | | | | |
| SQ-5 | When others in the family are awake, your child goes to sleep as usual. | | | | | |
| SQ-6 | You do not struggle much to make your child to sleep. | | | | | |
| SQ-7 | Your child do not wake up from sleep due to any activities in the house by others | | | | | |
| SQ-8 | Your child does not watch TV more than three hours in a day or at a stretch. | | | | | |
| SQ-9 | You do not give medicine to make your child sleep. | | | | | |
| SQ-10 | Your child do not snores during sleep. | | | | | |
| SQ-11 | Your child breaths from mouth during sleep. | | | | | |
| QS-12 | Your child wakes up early in the morning normally without effort. | | | | | |
| SQ-13 | Your child wake up and walk around when others are sleeping in the night. | | | | | |
| SQ-14 | Your child’s behaviour will not be disturbed if you wake him/her up forcibly. | | | | | |
| SQ-15 | Your child does not suffer from bed wetting problem. | | | | | |
Food and digestion questionnaire.
| Questionnaire for ParentsName of the Child:_____________________________________________________SECTION-II: FOOD AND DIGESTION |
|---|
| S.N. | STATEMENT | Agree | Rarely | Some times | Disagree | Strongly disagree |
|---|
| | 1 | 2 | 3 | 4 | 5 |
|---|
| FQ-1 | Your child does not over eat food. | | | | | |
| FQ-2 | You do not force your child to eat food every time. | | | | | |
| FQ-3 | Your child asks or indicates the need for food when hungry. | | | | | |
| FQ-4 | Your child eats all types of food (fruits, nuts, vegetables, cereals etc). | | | | | |
| FQ-5 | Your child does not ask for a particular type food every time. | | | | | |
| FQ-6 | Your child chews food properly and swallows. | | | | | |
| FQ-7 | Your child does not eat food more than three times in a day. | | | | | |
| FQ-8 | Your child do not demands more and more food every time during meal. | | | | | |
| FQ-9 | Your child does not like to eat fast food/hotel or readymade food. | | | | | |
| FQ-10 | Your child does not have digestion or bowel movement problems. | | | | | |
| FQ-11 | Your child does not have bloating or flatulence problems. | | | | | |
| FQ-12 | Your child does not go to toilet more than twice in a day for bowel movement. | | | | | |
| FQ-13 | Your child does not have urine or foecal incontinence problems. | | | | | |
| FQ-14 | You do not give medicine to your child for any digestion related problems. | | | | | |
| FQ-15 | Your child do not vomit sometimes if over eat food. | | | | | |
| FQ-16 | Your child is not over weight for his age? | | | | | |
| Questionnaire for ParentsName of the Child:_____________________________________________________SECTION - III : BEHAVIOUR |
|---|
| S.N. | STATEMENT | Agree | Rarely | Some times | Disagree | Strongly disagree |
|---|
| | 1 | 2 | 3 | 4 | 5 |
|---|
| BQ-1 | Your child sits at a place for more than 30 minutes without any activity. | | | | | |
| BQ-2 | Your child’s eye contact is normal and does not stare from unusual angle. | | | | | |
| BQ-3 | Your child’s attention span is normal as other children. | | | | | |
| BQ-4 | Your child does not run/walk around in the house without reason. | | | | | |
| BQ-5 | Your child adjusts to any changes made in the house without reaction. | | | | | |
| BQ-6 | Your child receives guests with a smile. | | | | | |
| BQ-7 | Your child communicates with guests normally like others in the house. | | | | | |
| BQ-8 | Your child shows curiosity about surroundings/objects and asks questions. | | | | | |
| BQ-9 | Your child does not cry or laugh without reason. | | | | | |
| BQ-10 | Your child expresses happiness and sorrow according to situation (emotion). | | | | | |
| BQ-11 | Your child responds and turns to you, when called by name. | | | | | |
| BQ-12 | Your child plays with toys appropriately according to age. | | | | | |
| BQ-13 | Your child picks objects, if asked by you. | | | | | |
| BQ-14 | Your child does not smell or lick objects or things when picked. | | | | | |
| BQ-15 | Your child has normal speech and does not produce unusual or meaningless sounds. | | | | | |
| BQ-16 | Your child use appropriate words during communication. | | | | | |
| BQ-17 | Your child does not show anxiety at any situation or depression. | | | | | |
| BQ-18 | Your child does not behave aggressively at any time during day. | | | | | |
| BQ-19 | Your child does not injure self by indulging in head bang, biting or hitting. | | | | | |
| BQ-20 | Your child does not injures others by pushing, pinching, biting or by hitting. | | | | | |
| BQ-21 | Your child does not have difficulty in processing and integrating sensory information or stimuli like seeing, hearing, smell, tasting and movements. | | | | | |
| BQ-22 | Your child do not involve in self stimulatory behaviours viz., finger flapping or head movement. | | | | | |
| BQ-23 | Your child do not swing mood suddenly due to some reason. | | | | | |
| BQ-24 | Your child plays and mingles with other children. | | | | | |
| BQ-25 | Your child is not afraid of or adversely reacts to loud sounds. | | | | | |
| BQ-26 | Your child does not have savant ability (extra ordinary skill in specific area). | | | | | |
| BQ-27 | Your child do not lacking in cognitive ability. | | | | | |
| BQ-28 | Your child will imitate most of your actions. | | | | | |
| BQ-29 | Your child’s hearing is normal as others. | | | | | |
| BQ-30 | Your child does not repeat the words instead respond with appropriate words. | | | | | |
Yoga intervention: Yoga module was prepared by researchers based on problematic area of ASD children for 75 minute duration held between 9.30 am and 10.45 am just before the school opening. Yoga practices were selected from S-VYASA Integrated Application of Yoga Therapy (IAYT) yoga modules used in Arogyadhama for different ailments and Bihar School of Yoga. Yoga module was as shown in the [Table/Fig-5] [23]. To make it easy for children entire yoga module was divided into two groups and each of the asana assigned with number 1 and/or 2. Asanas with number 1 and 2 were practiced on alternate days. Some of the asanas assigned with both 1 and 2 were practiced on all days. Parents were instructed to practice the asanas at home not practiced during sessions along with children and also in case they were unable to practice themselves in the process of helping their children during yoga sessions.
| S.N | Asanas | Time |
|---|
| 1 | Starting prayer | |
| 2 | Breathing Exercises | 2 Min |
| 3 | Preparatory/Dynamic Practice | 8 Min |
| 4 | Wind Releasing Practices | 7 Min |
| 5 | Sun Salutation (10 step and 12 step) | 6 Min |
| Relaxation | 1 Min |
| 6 | Standing asana | 8 Min |
| 7 | Sitting asana | 11 Min |
| 8 | Prone Posture | 2 Min |
| 9 | Supine Posture | 5 Min |
| 10 | Breathing Practices (Pranayama) | 8 Min |
| 11 | Relaxation | 8 Min |
| 10 | Chanting sloka | 9 Min |
| 11 | Ending Prayer | |
Statistical Analysis
SPSS-21.0 analytic software was used to find descriptive statistics of pre-test and post-test values. Since the sample size was small and data not normally distributed we have used Wilcoxon signed rank test to find significance in the post yoga intervention.
Results
All the 64 children were present during pre-test data collection from two groups. During post yoga intervention all the children from experiment group attended, but three from control group did not attend due to health reason and was considered as dropout. After analysis in [Table/Fig-6] which refers to sleep problems we found significance of 0.001 in almost all areas except SQ-7 which shows 0.002. Looking at mean values and standard deviations post data shows reduced values. In control group most of the pre and post values more or less remained same as this group continued with same activities other than yoga. We heard from parents’ about improved and uninterrupted sleep of children within one month of yoga intervention which helped family members and particularly mothers in managing child better way during day time.
| Statement | Yoga Group Pre Values | Yoga Group Post Values | Z-Score | Asymp. Sig (2-tailed) |
|---|
| Mean | ±Std. Deviation | Mean | ±Std. Deviation |
|---|
| Intervention Group |
| SQ-1 | 3.38 | 1.10 | 1.03 | 0.177 | -4.810c | 0.001 |
| SQ-2 | 3.63 | 1.10 | 1.38 | 0.554 | -4.695c | 0.001 |
| SQ-3 | 4.78 | 0.49 | 1.69 | 0.644 | -5.033c | 0.001 |
| SQ-4 | 4.13 | 1.16 | 1.47 | 0.567 | -4.760c | 0.001 |
| SQ-5 | 3.97 | 1.00 | 1.31 | 0.471 | -4.878c | .001 |
| SQ-6 | 4.00 | 1.02 | 1.13 | 0.336 | -5.139b | 0.001 |
| SQ-7 | 3.63 | 1.07 | 1.34 | 0.483 | -4.828c | 0.002 |
| SQ-8 | 1.97 | 1.33 | 1.34 | 0.483 | -2.271c | 0.001 |
| SQ-9 | 3.06 | 1.56 | 1.22 | 0.420 | -4.404c | 0.001 |
| SQ-10 | 3.50 | 1.11 | 1.59 | 0.499 | -4.703c | 0.001 |
| SQ-11 | 3.69 | 0.97 | 1.56 | 0.564 | -4.824c | 0.001 |
| SQ-12 | 4.22 | 1.26 | 1.13 | 0.336 | -4.824c | 0.001 |
| SQ-13 | 3.91 | 1.12 | 1.63 | 0.833 | -4.494c | 0.001 |
| SQ-14 | 4.59 | 1.19 | 1.47 | 0.567 | -4.833c | 0.001 |
| SQ-15 | 2.97 | 1.60 | 1.06 | 0.246 | -4.339c | 0.001 |
| Control Group |
| SQ-1 | 3.62 | 0.862 | 3.83 | 0.759 | -0.513c | 0.608 |
| SQ-2 | 3.62 | 1.115 | 3.93 | 0.961 | -1.127c | 0.260 |
| SQ-3 | 3.52 | 0.949 | 4.59 | 0.501 | -0.632c | 0.527 |
| SQ-4 | 4.52 | 0.574 | 4.21 | 0.620 | -0.277c | 0.782 |
| SQ-5 | 4.69 | 0.541 | 4.24 | 0.636 | -0.535b | 0.593 |
| SQ-6 | 4.83 | 0.384 | 4.38 | 0.728 | 0.000d | 1.000 |
| SQ-7 | 3.93 | 0.884 | 4.24 | 0.739 | -1.265c | 0.206 |
| SQ-8 | 3.52 | 1.326 | 3.00 | 1.363 | -2.124c | 0.034 |
| SQ-9 | 4.66 | 0.670 | 3.55 | 1.617 | -1.059c | 0.289 |
| SQ-10 | 3.79 | 0.819 | 4.07 | 0.842 | -0.905b | 0.366 |
| SQ-11 | 3.69 | 0.761 | 4.10 | 0.673 | -0.500b | 0.617 |
| SQ-12 | 3.83 | 0.711 | 4.38 | 0.862 | -0.486c | 0.627 |
| SQ-13 | 3.14 | 1.156 | 4.21 | 1.013 | -0.711c | 0.477 |
| SQ-14 | 3.14 | 1.302 | 4.66 | 0.670 | -0.431b | 0.666 |
| SQ-15 | 3.45 | 1.183 | 2.83 | 1.627 | -1.378c | 0.168 |
SQ = Sleep questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
[Table/Fig-7] FQ series questions refer to food and digestion problem which arises due to gastrointestinal problems. In this section also Wilcoxon signed rank test showing significant values of 0.001. After three months of yoga practice we found significant positive results in physiological problems like sleep and gastrointestinal problems. In this also, control group did not show any improvement.
Food and digestion questionnaires.
| Statement | Yoga Group Pre Values | Yoga group Post Values | Z Score | Asymp. Sig.(2-tailed) |
|---|
| Mean | ±Std. Deviation | Mean | ±Std. Deviation |
|---|
| Intervention Group |
| FQ-1 | 3.28 | 1.114 | 1.56 | 0.669 | -4.510b | 0.001 |
| FQ-2 | 2.69 | 1.281 | 1.22 | 0.491 | -4.060b | 0.001 |
| FQ-3 | 2.47 | 1.319 | 1.25 | 0.440 | -3.836b | 0.001 |
| FQ-4 | 4.22 | 1.184 | 1.47 | 0.507 | -4.743b | 0.001 |
| FQ-5 | 4.44 | 1.045 | 1.88 | 0.421 | -5.010b | 0.001 |
| FQ-6 | 4.31 | 1.424 | 1.66 | 0.483 | -4.729b | 0.001 |
| FQ-7 | 3.53 | 1.047 | 1.38 | 0.660 | -4.636b | 0.001 |
| FQ-8 | 2.78 | 1.289 | 1.56 | 0.716 | -3.433b | 0.001 |
| FQ-9 | 4.75 | .508 | 3.41 | 1.292 | -4.086b | 0.001 |
| FQ-10 | 3.56 | 1.045 | 1.09 | 0.296 | -4.874b | 0.001 |
| FQ-11 | 3.44 | 1.045 | 1.13 | 0.336 | -4.764b | 0.001 |
| FQ-12 | 3.31 | 1.203 | 1.19 | 0.397 | -4.651b | 0.001 |
| FQ-13 | 3.06 | 1.390 | 1.25 | 0.440 | -4.414b | 0.001 |
| FQ-14 | 3.13 | 1.212 | 1.13 | 0.336 | -4.589b | 0.001 |
| FQ-15 | 2.88 | 1.040 | 1.22 | 0.420 | -4.602b | 0.001 |
| FQ-16 | 3.03 | 1.769 | 1.53 | 0.842 | -3.917b | 0.001 |
| Control Group |
| FQ-1 | 3.62 | 0.862 | 3.72 | 0.751 | -0.905c | 0.366 |
| FQ-2 | 3.62 | 1.115 | 3.76 | 0.988 | -1.000c | 0.317 |
| FQ-3 | 3.52 | 0.949 | 3.86 | 0.915 | -3.162c | 0.002 |
| FQ-4 | 4.52 | 0.574 | 4.62 | 0.561 | -1.342c | 0.180 |
| FQ-5 | 4.69 | 0.541 | 4.52 | 0.688 | -2.236b | 0.025 |
| FQ-6 | 4.83 | 0.384 | 4.76 | 0.435 | -0.707b | 0.480 |
| FQ-7 | 3.93 | 0.884 | 4.00 | 0.886 | -0.384c | 0.701 |
| FQ-8 | 3.52 | 1.326 | 3.34 | 1.173 | -0.852b | 0.394 |
| FQ-9 | 4.66 | 0.670 | 4.66 | 0.614 | 0.000d | 1.000 |
| FQ-10 | 3.79 | 0.819 | 4.00 | 0.707 | -1.100c | 0.271 |
| FQ-11 | 3.69 | 0.761 | 3.97 | 0.680 | -1.886c | 0.059 |
| FQ-12 | 3.83 | 0.711 | 3.97 | 0.823 | -0.875c | 0.382 |
| FQ-13 | 3.14 | 1.156 | 3.52 | 1.153 | -1.950c | 0.051 |
| FQ-14 | 3.14 | 1.302 | 3.79 | 1.207 | -3.497c | 0.000 |
| FQ-15 | 3.45 | 1.183 | 3.83 | 1.071 | -1.915c | 0.056 |
| FQ-16 | 1.83 | 1.197 | 2.28 | 1.533 | -1.916c | 0.055 |
FQ=Food and digestion questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
In the [Table/Fig-8a,b] BQ series of questionnaires related to behaviour problems shows significance of 0.001 except BQ-26. BQ-26 refers to savant ability of children (extraordinary intelligent in specific area) may require longer period of yoga intervention to see changes. Other than this most of the mean and standard deviation values have shown lesser values in post data. Looking at all the three tables we have found significant changes in all areas of problems of ASD children after yoga intervention. In control group the severity of problems more or less remains same.
Behaviour questionnaire - yoga group. BQ=Behaviour.
| Statement | Yoga Group Pre Values | Yoga group Post Values | Z Score | Asymp. Sig. (2-tailed) |
|---|
| Mean | ±Std. Deviation | Mean | ±Sth. Deviation |
|---|
| BQ-1 | 4.79 | 0.412 | 1.94 | 0.878 | -5.000c | 0.001 |
| BQ-2 | 4.66 | 0.614 | 1.69 | 0.896 | -4.842c | 0.001 |
| BQ-3 | 4.48 | 0.738 | 2.16 | 0.574 | -4.983c | 0.001 |
| BQ-4 | 4.52 | 0.688 | 1.50 | 0.718 | -4.880c | 0.001 |
| BQ-5 | 4.17 | 0.805 | 1.47 | 0.671 | -4.776c | 0.001 |
| BQ-6 | 4.31 | 0.761 | 1.94 | 0.801 | -4.304c | 0.001 |
| BQ-7 | 4.52 | 0.634 | 2.56 | 0.840 | -4.593c | 0.001 |
| BQ-8 | 4.62 | 0.903 | 2.28 | 0.991 | -4.975c | 0.001 |
| BQ-9 | 4.52 | 0.738 | 1.41 | 0.665 | -4.786c | 0.001 |
| BQ-10 | 4.48 | 0.634 | 1.88 | 0.871 | -4.394c | 0.001 |
| BQ-11 | 3.38 | 1.015 | 1.13 | 0.336 | -4.140c | 0.001 |
| BQ-12 | 4.21 | .902 | 2.16 | 0.920 | -4.760c | 0.001 |
| BQ-13 | 3.93 | 1.132 | 1.34 | 0.653 | -4.239c | 0.001 |
| BQ-14 | 3.90 | 1.047 | 1.75 | 0.842 | -4.425c | 0.001 |
| BQ-15 | 4.34 | 1.078 | 3.06 | 1.134 | -4.588c | 0.001 |
| BQ-16 | 4.52 | .785 | 3.00 | 1.016 | -4.214c | 0.001 |
| BQ-17 | 4.03 | .906 | 1.41 | .615 | -5.024c | 0.001 |
| BQ-18 | 4.21 | 0.861 | 1.41 | 0.665 | -4.863c | 0.001 |
| BQ-19 | 3.72 | 1.032 | 1.38 | 0.554 | -4.639c | 0.001 |
| BQ-20 | 3.97 | 1.052 | 1.34 | 0.483 | -4.650c | 0.001 |
| BQ-21 | 4.69 | 0.712 | 2.19 | 0.535 | -4.963c | 0.001 |
| BQ-22 | 4.00 | 1.035 | 1.28 | 0.523 | -5.013c | 0.001 |
| BQ-23 | 4.10 | 0.618 | 1.31 | 0.592 | -4.735c | 0.001 |
| BQ-24 | 4.31 | 0.850 | 1.97 | 0.647 | -4.881c | 0.001 |
| BQ-25 | 3.34 | 1.289 | 1.38 | 0.751 | -4.019c | 0.001 |
| BQ-26 | 1.41 | 1.150 | 1.28 | 0.888 | -.659c | 0.510 |
| BQ-27 | 4.38 | 1.321 | 3.00 | 0.842 | -4.779c | 0.001 |
| BQ-28 | 3.93 | 1.280 | 1.28 | 0.457 | -4.470c | 0.001 |
| BQ-29 | 1.38 | 0.942 | 1.03 | 0.177 | -4.538c | 0.001 |
| BQ-30 | 4.48 | 1.243 | 2.72 | 0.924 | -5.000c | 0.001 |
questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
Behaviour questionnaire-control group.
| Statement | Control Group Pre Values | Control Group Post Values | Z Score | Asymp. Sig. (2-tailed) |
|---|
| Mean | ±Std. Deviation | Mean | ±Std. Deviation |
|---|
| BQ-1 | 4.79 | 0.412 | 4.83 | 0.384 | -0.577c | 0.564 |
| BQ-2 | 4.66 | 0.614 | 4.72 | 0.528 | -0.632c | 0.527 |
| BQ-3 | 4.48 | 0.738 | 4.62 | 0.561 | -0.905c | 0.366 |
| BQ-4 | 4.52 | 0.688 | 4.55 | 0.572 | -0.302c | 0.763 |
| BQ-5 | 4.17 | 0.805 | 4.45 | 0.572 | -1.809c | 0.070 |
| BQ-6 | 4.31 | 0.761 | 4.45 | 0.632 | -1.069c | 0.285 |
| BQ-7 | 4.52 | 0.634 | 4.62 | 0.561 | -1.000c | 0.317 |
| BQ-8 | 4.62 | 0.903 | 4.66 | 0.553 | 0.000d | 1.000 |
| BQ-9 | 4.52 | 0.738 | 4.41 | 0.682 | -0.832b | 0.405 |
| BQ-10 | 4.48 | 0.634 | 4.48 | 0.688 | 0.000d | 1.000 |
| BQ-11 | 3.38 | 1.015 | 3.69 | 0.891 | -1.631c | 0.103 |
| BQ-12 | 4.21 | 0.902 | 4.34 | 0.670 | -0.741c | 0.458 |
| BQ-13 | 3.93 | 1.132 | 4.00 | 0.926 | -0.259c | 0.796 |
| BQ-14 | 3.90 | 1.047 | 4.17 | 1.002 | -1.327c | 0.185 |
| BQ-15 | 4.34 | 1.078 | 4.41 | 1.086 | -0.816c | 0.414 |
| BQ-16 | 4.52 | 0.785 | 4.59 | 0.682 | -0.632c | 0.527 |
| BQ-17 | 4.03 | 0.906 | 4.24 | 0.689 | -1.511c | 0.131 |
| BQ-18 | 4.21 | 0.861 | 4.14 | 0.833 | -0.576b | 0.564 |
| BQ-19 | 3.72 | 1.032 | 3.90 | 0.900 | -1.051c | 0.293 |
| BQ-20 | 3.97 | 1.052 | 4.00 | 0.707 | -0.330c | 0.741 |
| BQ-21 | 4.69 | 0.712 | 4.83 | 0.602 | -0.330c | 0.395 |
| BQ-22 | 4.00 | 1.035 | 4.14 | 0.789 | -0.728c | 0.467 |
| BQ-23 | 4.10 | 0.618 | 4.21 | 0.726 | -0.728c | 0.467 |
| BQ-24 | 4.31 | 0.850 | 4.48 | 0.738 | -1.127c | 0.260 |
| BQ-25 | 3.34 | 1.289 | 3.52 | 1.184 | -0.771c | 0.441 |
| BQ-26 | 1.41 | 1.150 | 1.28 | 1.032 | -0.552b | 0.581 |
| BQ-27 | 4.38 | 1.321 | 4.79 | 0.491 | -1.294c | 0.196 |
| BQ-28 | 3.93 | 1.280 | 4.07 | 1.163 | -0.388c | 0.698 |
| BQ-29 | 1.38 | 0.942 | 1.45 | 1.242 | -0.172c | 0.863 |
| BQ-30 | 4.48 | 1.243 | 4.79 | 0.412 | -0.866c | 0.386 |
BQ = Behaviour questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
Discussion
Parents and teachers involvement made this intervention most effective. After pilot study we decided to involve teacher in this program and ten teachers volunteered to participate in this project. The yoga module was prepared keeping in mind sleep, gastrointestinal and behavioural problems of ASD children and to see its effects after yoga intervention. It was proved previously that yoga brings positive changes initially at physical level, then at mental level [24]. Most of the children’s imitating skills increased during the first few days of intervention which was essential for learning process and this helped children to practice asanas looking at their parents. Yoga helps ASD children to increase imitating skill was proved in one of previous study also [25]. According to parent’s feedback after one month of intervention most of the children improved in sleep and digestion related problems. During night children slept without any interruption for longer period compared to pre-intervention, going to bed in the night and getting up from bed in the morning not sleeping during day time were some of the improvements observed and this helped parents and other family members to have good sleep themselves during night. Some children who were snoring and breathing from mouth during sleep also stopped. Many children started taking balanced food instead of over eating every time. We advised parents to try with all types of food to provide balanced nutrition as it was proved in previous study that yoga helps in proper absorption of nutrients [26]. On behavioural part body awareness and body balancing increased which was reflected in children’s ability to remain in different postures for more than 30 seconds, which was proved in previous study also [27]. Children’s sitting tolerance and attention span increased significantly as per feedback received from parent and teachers. Three months of continuous yoga intervention reduced the severity of ASD symptoms according to parents. Children were very eager to come to yoga centre and they enjoyed sessions. In one of the previous study significant results were found after three months of yoga intervention [28]. Before yoga intervention most of the children were not making eye to eye contact, hence to improve this we made children to sit facing their mothers during sloka chanting as well as yoga practice, which helped children to improve in this area. Previous studies also indicate that yoga helps in psychological wellbeing and mood changes [29–31]. Post yoga intervention children’s aggressiveness and self-injurious behaviour reduced which had also been proved in previous study [32].
Limitation
Finding subjects and making parents to participate in such studies is very difficult. Both parents and teachers have their own limitation for participating in the study. We have to totally depend on parents for data collections.
Conclusion
This experiment proved that a structured yoga intervention can be conducted for a large group of ASD children in special schools with involvement of parents and teachers. Yoga intervention will improve sleep problems, gastrointestinal problems and behaviour problems of ASD children thereby reducing the severity of symptoms.
SQ = Sleep questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
FQ=Food and digestion questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
BQ = Behaviour questionnaire, a. Wilcoxon signed rank-test, b. Based on positive ranks, c. Based on negative ranks, d. The sum of negative ranks equals the sum of positive ranks
[1]. Xiao Z, Qiu T, Ke X, Xiao X, Xiao T, Liang F, Autism spectrum disorder as early neuro developmental disorder: evidence from the brain imaging abnormalities in 2-3-year-old toddlersJ Autism Dev Disord 2014 (44):1633-40. [Google Scholar]
[2]. Malhotra S, Rajender G, Bhatia MS, Singh TB, Effects of picture exchange communication system on communication and behavioural anomalies in autismIndian J Psychol Med 2010 32(2):141-43. [Google Scholar]
[3]. Miano S, Bruni O, Elia M, Trovato A, Smerieri A, Verrillo E, Sleep in children with autistic spectrum disorder: A questionnaire and polysomnographic studySleep Med 2007 9(1):64-70. [Google Scholar]
[4]. Rao PA, Beidel DC, Murray MJ, Social skills interventions for children with Asperger’s syndrome or high-functioning autism: a review and recommendationsJ Autism Dev Disord 2008 38:353-61. [Google Scholar]
[5]. American Psychological Association. Diagnostic and statistical manual of mental disorders-DSM-IV. 1994 [Google Scholar]
[6]. Lever AG, Geurts HM, Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorderJ Autism Dev Disord 2016 46:1916-30. [Google Scholar]
[7]. Loftin RL, Odom SL, Lantz JF, Social interaction and repetitive motor behavioursJ Autism Dev Disord 2008 38(6):1124-35. [Google Scholar]
[8]. Kanner L, Autistic disturbances of affective contactPathology 1943 [Google Scholar]
[9]. Kumar B, Prakash A, Sewal RK, Medhi B, Modi M, Drug therapy in autism: a present and future perspectivePharmacol Reports 2012 64:1291-304. [Google Scholar]
[10]. Khan NZ, Gallo LA, Arghir A, Budisteanu B, Budisteanu M, Dobrescu L, Autism and the grand challenges in global mental healthInt Soc Autism Res Wiley Period Inc 2012 5:156-59. [Google Scholar]
[11]. Klukowski M, Wasilewska J, Lebensztejn D, Sleep and gastrointestinal disturbancesDev Period Med 2015 :XIX.2 [Google Scholar]
[12]. Doshi-Velez F, Ge Y, Kohane I, Comorbidity clusters in autism spectrum disorders : an electronic health record time-series analysisPediatrics 2014 133:e54-e63. [Google Scholar]
[13]. Jyonouchi H, Geng L, Davido AL, Cytokine profiles by peripheral blood monocytes are associated with changes in behavioural symptoms following immune insults in a subset of ASD subjects: an inflammatory subtype ?Journal of Neuroinflammation 2014 11:187 [Google Scholar]
[14]. Gorrindo P, Williams KC, Lee EB, Walker LS, McGrew SG, Levitt P, Gastrointestinal dysfunction in autism: parental report, clinical evaluation, & associated factorsAutism Res 2012 5(2):101-08. [Google Scholar]
[15]. McElhanon BO, McCracken C, Karpen S, Sharp WG, Gastrointestinal symptoms in autism spectrum disorder: A meta-analysis abstractPediatrics 2014 133(5):872-83. [Google Scholar]
[16]. CDC 2016Community Report on AutismCDC Community Rep Autism 2016 65(No. SS-3):1-23. [Google Scholar]
[17]. Christensen DL, Baio J, Van Naarden Braun K, Community Report on AutismCDC Community Rep Autism 2016 65:01-23. [Google Scholar]
[18]. Levy SE, Mandell DS, Schultz RT, AutismLancet 2009 374(9701):1627-38. [Google Scholar]
[19]. Porter J, Yoga as an effective behavioural intervention for children diagnosed with an autism spectrum disorderGrad Annu 2013 1(9) [Google Scholar]
[20]. Satishchandra P, Yoga and neurobehavioural sciences: Indian perspectiveIndian J Psychiatry 2015 2013:332-33. [Google Scholar]
[21]. KeshavanM S, Rao NP, Rao TSS, Yoga and mental health : Promising road ahead, but proceed with cautionIndian J Psychiatry 2013 55:S329-31. [Google Scholar]
[22]. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research. WHO. 1993 [Google Scholar]
[23]. Koenig KP, Reen AB, Garg S, Get Ready to Learn classroom yoga program for children with autism spectrum disorders on decreasing maladaptive behaviours and improving educational outcomes?American Journal of Occupational Therapy 2012 66:538-46. [Google Scholar]
[24]. Büssing A, Michalsen A, Khalsa SBS, Telles S, Sherman KJ, Effects of yoga on mental and physical health: a short summary of reviewsEvidence-based complementary and alternative medicine 2012 Volume 2012:165410 [Google Scholar]
[25]. Radhakrishna S, Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorderInt J Yoga 2010 3:26-30. [Google Scholar]
[26]. Verma A, Shete SU, Thakur GS, Bhogal RS, Effect of yoga practices on micronutrient absorption and physical fitness in rural residential school children: a randomized controlled trialInt J Ayurveda Pharma 2014 5(2):179-84. [Google Scholar]
[27]. Radhakrishna S, Nagarathna R, Nagendra HR, Integrated approach to yoga therapy and autism spectrum disordersJ Ayurveda Integr Med 2010 1(2):120-24. [Google Scholar]
[28]. Deorari M, Bhardwaj I, Effect of yogic intervention on autism spectrum disorderYoga Mimamsa 2014 46(3):81-84. [Google Scholar]
[29]. Koenig KP, Buckley-reen A, Garg S, Efficacy of the get ready to learn yoga program among children with autism spectrum disorders: a pretest – posttest control group designAm J Occup Ther 2012 66(5):538-46. [Google Scholar]
[30]. Noggle JJ, Steiner NJ, Minami T, Khalsa SBS, Benefits of yoga for psychosocial well-being in a US high school curriculum: a preliminary randomized controlled trialJ Dev Behav Pediatr 2012 33(3):193-201. [Google Scholar]
[31]. Narasingharao K, Pradhan B, Navaneetham J, Sleep disorder, gastrointestinal problems and behaviour problems seen in autism spectrum disorder children and yoga as therapy: a descriptive reviewJ Clin Diagn Res 2016 10(11):VE01-VE03. [Google Scholar]
[32]. Sharma N, Sharma N, Effect of yogic and recreational activities for improving self- injurious and aggression behaviour of autistic children objectives: rupkathaJournal on Interdisciplinary Studies in Humanities 2016 VIII(2) [Google Scholar]