BPES is a complex and rare disease characterized by epicanthus inversus, telecanthus, lateral ectropion, narrowed or shortened inter palpebral fissure distance and ptosis [1–3]. It is mostly bilateral and may or may not be symmetrical [Table/Fig-1]. It is typically inherited as an autosomal dominant trait. But in sporadic cases, the disease may occur without family history where genetic mutation from deletion or translocation of the FOXL2 gene which maps to chromosome 3q23 [4,5]. Surgical treatment of this disease poses an oculoplastic challenge due to multiple complex eyelid deformities. Various surgical techniques have been described for treating BPES. They are as follows: V-Y procedure, Mustarde’s double Z-plasty, 5-flap technique, plication of medial palpebral ligaments and trans-nasal wire fixation for epicanthus and telecanthus correction [6–9]. There is no hard and fast rule for surgical correction of the disease. We introduce a unique two-stage correction of BPES.
Materials and Methods
This study was started in Regional Institute of Ophthalmology of Medical College Calcutta from January 2013 to December 2015 for the period of three years. This was a prospective interventional study of 16 patients over a period of three years. All the patients had BPES with prominent epicanthus and telecanthus. A two-staged reconstructive procedure was utilized to correct the BPES. All patients underwent a full ophthalmological evaluation that included visual acuity, ocular motility, slit lamp examination and fundus examination. Eyelid measurements were performed pre and postoperatively and included the IICD, (MRD-1) and HPFL. The HPFL was measured from the precise point of contact of the upper and lower lid medially to the lateral canthus. IICD was measured from the precise point of contact of the upper lid with the lower lid on both sides. All investigators adhered to the principles outlined in the declaration of Helsinki. In addition, the Institutional Ethics Committee at the Medical College Calcutta, in Kolkata, India, approved the study. These values were then statistically analyzed. Data entry was done in epidata version 3.1 and data analysis was done in SPSS version 20. As the number of patient was less number of eyes were counted for statistical analysis. Data are presented as mean±SD.
Inclusion criteria of this study were age between 5 and 45 years, all patients with all the components of BPES and all the patients with moderate (3 mm) and severe (4 mm) ptosis. Patients with vertical squint, poor Bell’s phenomenon, Marcus-Gunn jaw winking phenomenon, mild (2 mm) to moderate (3 mm) ptosis, previous ptosis surgery, corneal anaesthesia and nystagmus were excluded from the study.
Description of Two Staged Surgical Procedure
The reconstructive surgical correction of blepharophimosis was performed in two stages, set three months apart. In the 1st stage, a Mustarde’s rectangular double Z-plasty with trans-nasal fixation with 1-0 prolene was performed. In the 2nd stage, a lateral canthoplasty and tarsofrontalis sling with a silicone rod were performed for moderate to severe ptosis correction. All the procedures were performed under general anaesthesia. In the Mustarde’s double Z-plasty procedure, the epicanthus was marked first, then traction was placed on the skin towards the bridge of the nose. A horizontal line was drawn between the sites of the desired medial canthus and actual present medial canthus. An additional line is drawn from midpoint of the previous line which was angulated 60 degree above and below and slanting towards the eye. These angulated lines are longer than half of the distance of the first drawn line. It was the line joining the actual and desired medial canthus. Incisions were made along these markings, raising four rectangular flaps [Table/Fig-2a]. The soft tissue underneath was dissected, exposing the insertion site of the medial palpebral ligament. The anterior lacrimal crest was identified. A 3.5 mm gauge manual orthopaedic drill was then used to place a hole in the frontal process of the maxilla at the anterior lacrimal crest [Table/Fig-2b]. Both sides of the medial palpebral ligaments were exposed and tacked more towards tarsal attachment with 1-0 prolene suture. The suture was then passed through the intranasal bone tunnel by a Wright fascia needle [Table/Fig-2c]. Tightening of the suture causes close approximation of the two ends of ligament toward the bridge of the nose.
Steps of the multistage correction of blepharophismosis syndrome.
a) Skin marking of Double Z-Plasty in epicanthal area; b) Manual 3.5 gauze orthopaedic drill is used to made hole in a frontal process of the maxilla at the anterior lacrimal crest; c) 1-0 Prolene suture used for intranasal fixation; d) Double Z-Plasty and flap transfer from upper to lower lid lateral ectropion correction; e) Lateral canthoplasty; f) Bilateral tarsofrontalis sling.
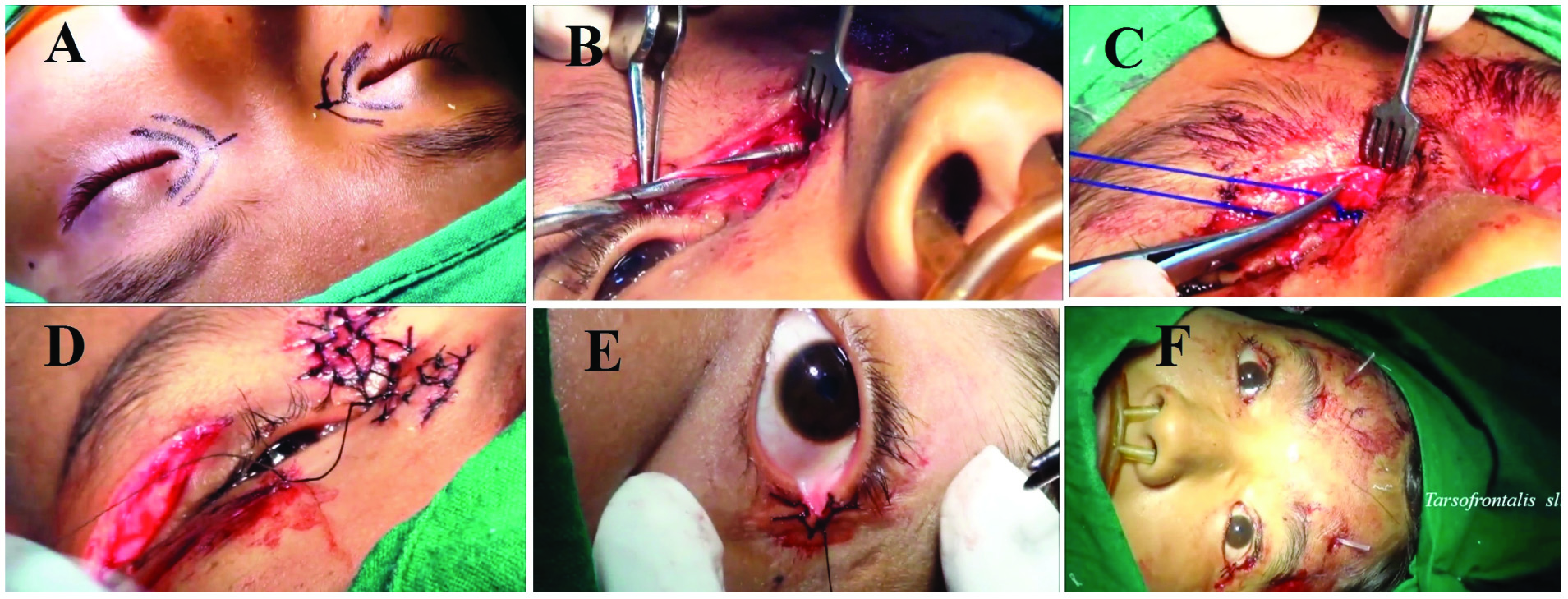
This corrects the deeper component of telecanthus. Two rectangular flaps created at the skin surface are transposed and repaired in a triangular fashion, which was the principal of the double Z-plasty. A 5-0 silk suture was placed to reapproximate the skin edges [Table/Fig-2d]. In this procedure, there was advancement of the medial canthus and simultaneous vertical stretching of skin at canthal region. Thus, telecanthus and epicanthus were corrected. A pressure patch was applied. After three months, a 2nd stage procedure was undertaken. In this stage, a lateral canthoplasty was performed for horizontal lid fissure widening in the usual oculoplastic fashion [Table/Fig-2e]. Further, a tarsofrontalis sling ptosis repair utilizing a silicone rod in the typical fox pentagon formation was performed to correct the moderate to severe ptosis [Table/Fig-2f]. Postoperatively, all patients were continued on a silicone gel to the surgical wounds for six months.
Results
A total of 16 patients with 32 eyes were enrolled in this study, of which 10 (62.2%) were females and 6 (37.5%) were males. All patients had bilateral involvement, with a total number of 32 eyes. The mean age of patient was 11.50 years, ranging from 7 to 15 years. All patients had good postoperative cosmetic and functional outcome. All surgeries were done under general anaesthesia. Preoperative IICD ranged from 38 mm to 42 mm and the mean IICD was 41.2±0.57 mm. Postoperative IICD ranged from 31 to 34 mm and the mean value was 33.25±0.70 mm after correction of telecanthus. The preoperative HPFL ranged from 20 mm to 23 mm with a mean value of 21.50±1.01 mm and postoperatively ranged from 26 mm to 29 mm with a mean value of 28±0.50 mm. The mean preoperative IICD and HPFL ratio was 1.77 preoperatively and 1.2 postoperatively. The preoperative MRD-1 value improved from +1.25 mm to +3.50 mm postoperatively after fox pentagon tarsofrontalis sling with silicone rod [Table/Fig-3]. In this study, two eyes had minimal asymmetric correction but were cosmetically and functionally acceptable [Table/Fig-4]. All patients had minimal visible scarring at their last follow up visit.
Pre- and postoperative measurement of BPES. Variables include Inner Intercanthal Distance (IICD) measured in mm, Horizontal Palpebral Fissure Length (HPFL) measured in mm and Marginal Light Reflex Distance (MRD-1) measured in mm.
| No. of Patient Eye | Preoperative IICD (in mm) | Postoperative IICD (in mm) | Preoperative HPFL (in mm) | Postoperative HPFL (in mm) | Preoperative IICD and HPFL ratio | Postoperative IICD and HPFL ratio | Pre op MRD1 (in mm) | Post op MRD1 (in mm) |
|---|
| 1. | 40 | 32 | 21 | 28 | 1.90 | 1.14 | +1 mm | +4 mm |
| 2. | 41 | 33 | 22 | 27 | 1.86 | 1.22 | +1 mm | +3 mm |
| 3. | 42 | 33 | 24 | 29 | 1.75 | 1.13 | +1.5 mm | +4 mm |
| 4. | 41 | 32 | 23 | 28 | 1.78 | 1.14 | +2 mm | +4 mm |
| 5. | 40 | 33 | 21 | 26 | 1.90 | 1.26 | +1.5 mm | +3 mm |
| 6. | 41 | 34 | 22 | 27 | 1.86 | 1.27 | -1 mn | +4 mm |
| 7. | 41 | 33 | 21 | 29 | 1.91 | 1.13 | +1.5 mm | +3 mm |
| 8. | 42 | 34 | 23 | 28 | 1.82 | 1.21 | +1 mm | +3 mm |
| 9. | 40 | 33 | 23 | 29 | 1.73 | 1.19 | +1.5 mm | +4 mm |
| 10. | 39 | 32 | 22 | 28 | 1.77 | 1.10 | +1 mm | +3 mm |
| 11. | 38 | 32 | 23 | 29 | 1.65 | 1.10 | +1 mm | +4 mm |
| 12. | 39 | 33 | 22 | 28 | 1.77 | 1.17 | +1.5 mm | +3 mm |
| 13. | 40 | 33 | 22 | 27 | 1.81 | 1.22 | +1.5 mm | +4 mm |
| 14. | 41 | 33 | 23 | 28 | 1.70 | 1.17 | 0 mm | +3 mm |
| 15. | 38 | 34 | 23 | 29 | 1.65 | 1.22 | +1 mm | +3 mm |
| 16. | 42 | 33 | 20 | 28 | 1.78 | 1.23 | +1.5 mm | 4 mm |
| 17. | 41 | 32 | 22 | 28 | 1.86 | 1.14 | +1 mm | +4 mm |
| 18. | 42 | 34 | 23 | 29 | 1.82 | 1.17 | +1.5 mm | +3 mm |
| 19. | 39 | 32 | 22 | 28 | 1.17 | 1.14 | +1.5 mm | +4 mm |
| 20. | 40 | 34 | 23 | 29 | 1.73 | 1.17 | +1 mm | +3 mm |
| 21. | 41 | 33 | 23 | 27 | 1.86 | 1.22 | +1.5 mm | +4 mm |
| 22. | 42 | 34 | 23 | 29 | 1.82 | 1.17 | +0 mm | +3 mm |
| 23. | 41 | 32 | 22 | 28 | 1.86 | 1.14 | +1.5 mm | +4 mm |
| 24. | 42 | 33 | 23 | 29 | 1.82 | 1.13 | +1.5 mm | +3 mm |
| 25. | 41 | 34 | 22 | 28 | 1.86 | 1.21 | +0 mm | +3 mm |
| 26. | 42 | 33 | 22 | 29 | 1.90 | 1.13 | +1 mm | +4 mm |
| 27. | 41 | 34 | 21 | 27 | 1.95 | 1.25 | +0 mm | +3 mm |
| 28. | 42 | 33 | 22 | 29 | 1.90 | 1.13 | +1 mm | +4 mm |
| 29. | 41 | 32 | 23 | 29 | 1.78 | 1.10 | +0 mm | + 3 mm |
| 30. | 41 | 33 | 22 | 28 | 1.86 | 1.17 | +0 mm | +3 mm |
| 31. | 42 | 32 | 23 | 29 | 1.82 | 1.10 | +2 mm | +4 mm |
| 32. | 41 | 33 | 23 | 29 | 1.78 | 1.13 | +1 mm | +4 mm |
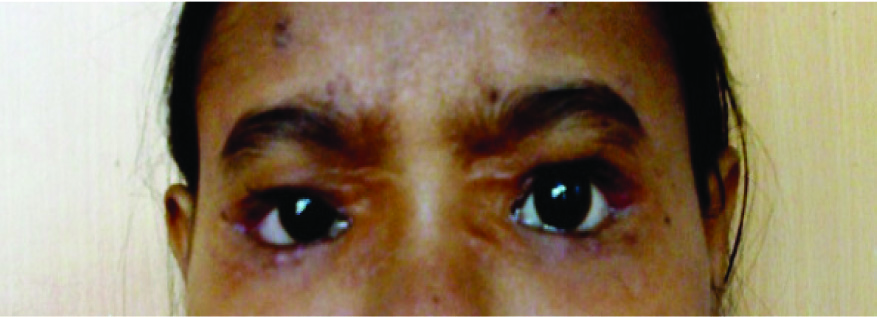
Postoperative images after two stage correction of BPES.
Discussion
BPES is a very uncommon disease. This study was able to include a moderate number of patients which would take most oculoplastic surgeons many years to accumulate. In this study as the number of patient is less, number of eyes was counted for statistical analysis. Because the disease is uncommon and complex, there are multiple procedures described in the literature to correct it. Each has their benefits and shortcomings.
Patients with BEPS require a single or multistage periocular correction during childhood. There is controversy regarding the best modality of surgical management of this condition. Some authors believe that a one stage correction of BPES is effective [9–11] . They believe it requires less surgical time, is cost effective and also avoids additional anaesthetic hazards. Early surgical rehabilitation is possible by avoiding multiple surgical procedures and reducing the patients (and parents) discomfort. There are downsides to this approach. Medial canthoplasty may be unpredictable in a one stage procedure. Further, many surgeons believe that epicanthus inversus and telecanthus should be corrected first before ptosis correction because the tension created by respective surgeries oppose each other [6,12,13]. When ptosis correction and Mustarde’s double Z-plasty performed simultaneously, ptosis generates vertical force and Z-plasty may cause horizontal force. These were antagonists of each other. Thus patient may cause insufficiency and loosening of epicanthal correction and as well as poor elevation of upper eyelid. In regards to correction of telecanthus, Callahan A et al., initially described the use of a transnasal wire fixation of the medial canthus [1]. Wu et al., recommended using a transnasal wiring procedure with an intentional overcorrection of 4 mm to ensure an adequate reduction for telecanthus when accounting for any possible regression to postoperative measurements [11]. Of note, patients with severe ptosis in the study were noted to be poor candidates for a one-stage correction. In this study, all patients had good vision with no amblyopia because all patients maintained their vision by compensatory chin elevation. Regardless, the authors still believe these patients require early ptosis correction due to abnormal head posture.
Our study followed a two stage approach that combined aspects of previously described procedures in a unique way that is very effective. Further, it is the first to describe the use of a 1-0 prolene suture for transnasal fixation. In the first stage of our proposed two-stage correction, telecanthus is corrected by abolishing epicanthal folds and improving the IICD. A Mustarde’s rectangular double Z-plasty, along with trans-nasal fixation with 1-0 prolene suture, yields the highest correction [14,15]. In this study, it was observed that we initially over corrected the IICD by 8 mm or more, but the soft tissue had a tendency to reverse to its previous position. Of note, the palpebral fissure widening was enforced by a lateral canthoplasty performed in the second stage and we gained 4 mm, albeit with mild regression. With this combined procedure, the net result of horizontal lid fissure widening is satisfactory and the average final length is 28.5 mm, a gain of approximately 7 mm. Some surgeons believe in V-Y Plasty and plication of the medial palpebral ligament, but this technique is used in a mild form BPES, whereas in its severe form, this procedure is not effective. Sebastia et al., reported and utilized the Z-epicanthoplasty which is simple and has similar results to the Mustarde’s flaps procedure [9]. Li H et al., reported better results with the Y to V procedure especially in patients older than 10 years of age [7].
Some surgeons believe that plication of the medial palpebral ligament and fixation to subcutaneous tissue alone is effective in correction of telecanthus in BPES [8]. In the long run, the result is not satisfactory in severe telecanthus. Trans-nasal wiring provides a more effective traction of the ligaments and better reduction of the intercanthal distance. In this study, nonabsorbable 1-0 prolene suture was used for trans-nasal fixation, which has not yet been described. Close approximation of the two medial palpebral ligaments is possible using this technique. As the suture is thick and non absorbable, long term tensile strength is well maintained. Prolene suture is easy to introduce as a new surgical material and is cost effective. Stainless steel wire or titanium, as classically utilized in the transnasal wire technique, can be difficult to introduce and tightening of these materials required extra skill and instrumentation. Further, exposure or extrusion of the wire is a known complication. This further argues for the use of prolene suture, which is easily available in the market, provides good tensile strength, is cost effective, is an easy material to introduce, does not create tissue reaction and produces almost no complications. To perform this procedure we used a manual 3.5 mm gauge orthopaedic drill. We avoided the motorized drill, where the control of speed is difficult during the puncture of the outer table of the nasal bone. Using a manual drill for the outer table puncture, we slowed down the drill speed with the metallic guard, thus avoiding the risk of injury to the opposite eye. Additionally, the previously created flaps should be meticulously preserved, which is more achievable with a manual drill. Additionally in BPES, lateral ectropion is observed, which is corrected by a base out flap transfer from the upper eyelid to the lower eyelid for effective correction [Table/Fig-2d]. However, ectropion is not present in all cases. In this study, eight cases had lateral ectropion, which were corrected by this technique with good result. In the second stage of the procedure, we performed a lateral canthoplasty to help widen the palpebral fissure horizontally. This was done with the concurrent placement of a tarsofrontalis sling with silicone rod in a Fox’s Pentagon technique for severe ptosis correction. Additionally, the lateral canthoplasty further aids in effective ptosis correction. We believe that effective ptosis correction with formation of the anatomic eyelid crease and eyelash direction significantly improves the patients cosmetic appearance in addition to the obvious functional improvement in visual field. In this series, preoperative MRD-1 values changed from +1.25 mm to +3.5 mm, creating a very significant elevation of the upper eyelid and resolution of the ptosis. Other techniques for ptosis correction are abundant in the literature. Some author use LPS resection or LPS placation for moderate to severe ptosis correction. Some surgeons use autogenous fascia lata as suspension material for ptosis correction. This technique requires a second surgical site and further surgical counseling for the parents. Furthermore, in patients less than five years of age, it may be difficult to obtain due to insufficient fascia lata for harvesting.
Other authors considered levator resection for ptosis correction in BPES [16]. Several authors advocate for this approach. Blomgren and Holmstrom [17] proposed levator resection for all types of congenital ptosis. Mauriello JA et al., reported that maximal levator resection is indicated for severe congenital ptosis with poor to absent levator function, especially if the ptosis is unilateral [18]. However, with that technique, there is significant scar formation in fact, levator resection using a small skin incision or using a conjunctival approach has lesser scarring than sling procedure and a higher probability of under correction. In this study, we performed a fox’s Pentagon tarsofrontalis sling with silicone rod in all patients for the correction of moderate to severe ptosis. This allowed for one surgical site, provided for good outcomes in the setting of poor levator function and provides an adjustable sleeve with an under correction. In sling surgery, there is a risk of lid lag in down gaze and lagophthalmos, scarring in younger population, loss of lid crease in, unsatisfactory geometric tenting of the preseptal skin and poor tarsocorneal interface on brow elevation and down gaze. The surgical and functional outcome was excellent in this patient population.
Limitation
The patient with broad base of the nose with severe telecanthus and phimosis or short palpebral aperture was poor candidate for transnasal drilling and wire or proline fixation. These patients were excluded in this study.
Conclusion
There are various strategies and techniques described for correcting BPES. The study presented elucidates a proposed two-stage procedure that is very effective, alleviating the functional and cosmetic deficiencies of this complex and rare syndrome. There are dramatic improvements in telecanthus, horizontal fissure length, lateral ectropion and ptosis with this approach.
Video Link
https://youtu.be/iQms-2aO92Y