Thallium was once commonly used as a household rodent or ant killer, but many countries have banned such use due to unintentional or criminal poisonings of humans. A common initial clinical manifestation of thallium poisoning is gastrointestinal symptoms followed by delayed onset of neurological symptoms and alopecia. These clinical characteristics can provide important diagnostic clues regarding thallium poisoning. Here, we report a 23-year-old woman who was poisoned by a business colleague when she unknowingly drank tea containing the toxic substance several times. The patient was treated with multi-dose activated charcoal with airway protection and Prussian blue.
Alopecia, Haemodialysis, Neuropathy, Prussian blue
Case Report
A 23-year-old woman presented to the emergency department due to fatigue and unexplained muscle pain starting seven days before the hospital visit. The patient had no history of depression or mood disorders and was not taking any medications for mood disorders. She drank tea at school and noticed that the taste was different from ordinary tea eight days before she reported to us.
On the next day, she felt muscle pain in both thighs that spread gradually to the lower legs. On the seventh day, the patient suffered from plantar numbness and gastrocnemius muscle pain, with nausea, abdominal pain, and hair loss in her temporal region.
On examination, her blood pressure was 114/78 mmHg and her pulse rate was 65 beats per minute. Initial routine laboratory test results were unremarkable. Audiological examination revealed no symmetrical hearing loss. Ophthalmological examination demonstrated no loss of function or vision. The nerve conduction velocity of the lower legs were normal.
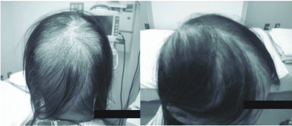
On the 10th day, a business associate of the patient, surrendered herself to the police and reported that she had put thallium sulphate into the patient’s tea cup on several occasions. Based on the report given by the police department, we made the diagnosis of thallium intoxication by unknowingly drinking tea containing thallium. The regional poison centre requested a medical toxicology consultation, which resulted in the recommendation to give the patient multi-dose activated charcoal with airway protection and Prussian blue. Multi-dose activated charcoal, intravenous fluids, vitamin B12, and an intravenous lorazepam infusion were administered to the patient. After obtaining information on thallium intoxication, two weeks after poisoning, urine and blood samples obtained on admission were sent for quantitative thallium level testing. Alopecia in the parietal region of the head started in the first week and became more prominent in the next few weeks [Table/Fig-1].
The blood and urine thallium levels measured on day 10 were 223 μg/L and 351 μg/L, respectively. Brain MRI images were performed, which showed no abnormal findings. In the six month follow up, neurological examination of factors including pain, sensory disturbance, and abnormal tendon reflex revealed improvement of polyneuropathy.
Discussion
Thallium is a colourless, water-soluble, tasteless heavy metal. Recently, reports concerning homicidal poisoning with thallium salt solutions have increased [1]. As in the present case, thallium poisoning victims usually do not know that they have consumed or have been exposed to the substance, so the particular symptoms of thallium poisoning are imperative for diagnosis. Thallium poisoning is rare and often misdiagnosed until it is confirmed by increased concentration of thallium in the urine and blood, resulting in delay of appropriate treatment [2].
Clinical manifestation varies according to the route of exposure and the victim’s dose and age. Nonspecific but typical clinical manifestations of thallium toxicity consist of quickly progressing, increasing, severely painful sensory polyneuropathy, hair loss, and visual impairment [3].
As in the present case, initial symptoms develop one to two days after ingestion. The biological half-life of thallium has a wide range of 1 to 30 days and depends on the entry route into the body, initial constipation, and enterohepatic circulation [4].
Acute thallium poisoning in the first few hours after ingestion occurs due to intravascular distribution of thallium. The symptoms are initially indistinguishable from those produced by other causes of acute gastrointestinal toxicity and can produce gastrointestinal symptoms and signs such as acute abdominal pain and vomiting.
The intermediate stage, the distribution of thallium into the central nervous system within several days of exposure, causes paraesthesia, lethargy, myocardial abnormalities, and coma. After a latency period of about three to seven days, the main target becomes the nervous system, in which hyperalgesia gradually develops, especially in the legs, followed by muscle weakness ascending from the lower extremities, indicative of heavy metal toxicity [5]. Thallium poisoning victims often lose their hair and develop cranial nerve impairment. Botulism, Guillain-Barre syndrome, and lead or arsenic intoxication should especially be mentioned as differential diagnostic options [6,7]. Elevated thallium levels in the urine or in other biologic materials such as hair confirms the diagnosis of poisoning.
Managing neuropathic pain involves the use of a combination of antidepressants, anticonvulsants, and opiates. Prussian blue is a sequestering agent for certain heavy metal ions and a thallium poisoning antidote. Treatment with Prussian blue (or activated charcoal) interrupts the enterohepatic cycling of thallium, thus enhancing faecal elimination of the metal. These evidences are based on results from case reports or animal studies, however, Prussian blue is recommended in acute thallium poisoning because of its safety [8]. Urinary thallium excretion is enhanced by forced diuresis with potassium repletion, which should be undertaken cautiously due to precipitation of neurological and cardiac toxicity [4]. Because of its small size and its lack of protein binding, thallium is considered dialyzable [8]. Therefore, haemodialysis should be considered early in massive toxicities.
The lethal thallium dose in humans is reported to be 10-15 mg/kg; deaths can occur in adults with doses as low as 8 mg/kg [1,9]. Thallium is quickly and almost completely absorbed via all pathways, including through the mucosa and skin; gastrointestinal absorption most commonly causes toxicity. Chronic toxicity usually occurs due to inhalation or skin exposure mostly secondary to chronic occupational exposure. Thallium is distributed to all tissues and becomes most highly concentrated in the muscles, intestines, kidney, liver, brain, and heart.
The mechanisms of thallium intoxication include the substitution of potassium in sodium-potassium-adenosine triphosphatase, as well as a high affinity for the sulfhydryl or thiol group of mitochondrial membranes, resulting in inhibition of energy production at the kreb’s cycle and oxidative phosphorylation [10]. In addition, thallium disrupts calcium homeostasis.
Published data on the prognosis for severe thallium poisoning is limited, especially regarding the reversibility of neurological and vision impairment [6]. However, overall, the long-term prognosis of neurological impairment seems to be relatively good for patients who survive the acute phase of thallium poisoning.
Conclusion
Acute thallium poisoning commonly produces gastrointestinal symptoms, painful polyneuropathy, and significant alopecia. Treatments include Prussian blue and haemodialysis, which are associated with good outcomes. Our experience, encountered in the diagnosis and management of this relatively rare poisoning, can provide helpful information on the clinical features, early diagnosis, and therapy of homicidal thallium poisoning.
[1]. Al Hammouri F, Darwazeh G, Said A, Ghosh RA, Acute thallium poisoning: series of ten casesJ Med Toxicol 2011 7(4):306-11. [Google Scholar]
[2]. Misra UK, Kalita J, Yadav RK, Ranjan P, Thallium poisoning: emphasis on early diagnosis and response to haemodialysisPostgrad Med J 2003 79(928):103-05. [Google Scholar]
[3]. Saddique A, Peterson CD, Thallium poisoning: a reviewVet Hum Toxicol 1983 25(1):16-22. [Google Scholar]
[4]. Mulkey JP, Oehme FW, A review of thallium toxicityVet Hum Toxicol 1993 35(5):445-53. [Google Scholar]
[5]. Cavanagh JB, What have we learnt from Graham Frederick Young? Reflections on the mechanism of thallium neurotoxicityNeuropathol Appl Neurobiol 1991 17(1):3-9. [Google Scholar]
[6]. Pelclova D, Urban P, Ridzon P, Senholdova Z, Lukas E, Diblik P, Two-year follow-up of two patients after severe thallium intoxicationHum Exp Toxicol 2009 28(5):263-72. [Google Scholar]
[7]. Sun TW, Xu QY, Zhang XJ, Wu Q, Liu ZS, Kan QC, Management of thallium poisoning in patients with delayed hospital admissionClin Toxicol (Phila) 2012 50(1):65-69. [Google Scholar]
[8]. Aoyama H, Yoshida M, Yamamura Y, Acute poisoning by intentional ingestion of thallous malonateHum Toxicol 1986 5(6):389-92. [Google Scholar]
[9]. Riyaz R, Pandalai SL, Schwartz M, Kazzi ZN, A fatal case of thallium toxicity: challenges in managementJ Med Toxicol 2013 9(1):75-78. [Google Scholar]
[10]. Galvan-Arzate S, Santamaria A, Thallium toxicityToxicol Lett 1998 99(1):1-13. [Google Scholar]