As per the World Health Organization’s estimation the annual incidence of TB in India accounts to 2.0 million - 2.3 million and about 1.5 million - 3.5 million deaths per year thus, making India as the highest contributor of TB burden in the world [1]. In addition to the burden of this disease the economic damage owing to this disease is equally disastrous with an estimated economic loss of $23 bn (£14.9 bn; €20.3 bn) each year [2]. The control of TB primarily depends on early diagnosis of pulmonary TB cases and their treatment with a full course of anti-tuberculosis drugs [3]. Thus, for early diagnosis all the suspected TB symptomatics with cough of two weeks should be referred for TB evaluation. Subsequently the correct treatment requires adherence to standard treatment protocols recommended by World Health Organization and other pertinent standards of TB care such as International Standards for TB Care (ISTC) and the Standards for TB Care in India (STCI) [4,5].
One of the recent systematic reviews reveal that delays in diagnosis can be up to two months in Indian settings and patients are seen by several providers before getting diagnosed with TB [6,7]. Furthermore drug prescription audits reveal irrational and inappropriate use of anti-tuberculosis drugs in various instances [8]. Moreover, these studies also report that the quality of TB care in India is a matter of great concern [9]. Given this context health education and awareness programmes can play a major role in creating awareness and help in changing behaviour and mobilize communities towards TB care in right direction. Several studies have shown different level of impact in changing behaviour and mobilizing the community towards TB care in different parts of India and outside as well [10–14]. In this study the impact of a structured and predesigned health awareness strategy on families in a slum area is assessed.
Materials and Methods
The study was a prospective interventional study conducted over a period of one month from 1st July 2016 to 31st July 2016. A structured and predesigned TB awareness intervention was implemented in terms of informing the houses of marginalized and vulnerable communities about TB, its symptoms, diagnosis, treatment and RNTCP services and the impact of the same was assessed through a survey questionnaire before and after the implementation of the intervention. After obtaining both of these survey the data analysis was then carried out to assess the level of impact. The questionnaire used in this study is mentioned in annexure-1. The questionnaire was translated in to Hindi by the first author and latter checked and validated by both the authors and a local language expert and then used for data collection.
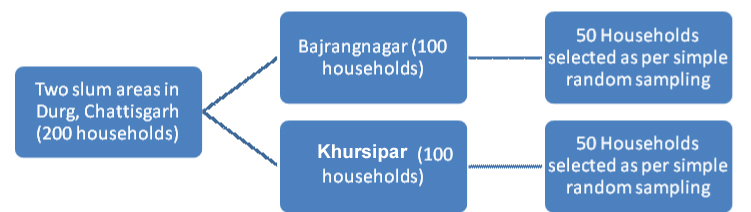
Sampling frame and technique: Simple random sampling technique was used to obtain the desired number of households in two different slums in Durg district of Chhattisgarh. The selected area was initially looked into for the feasibility of the study in terms of number of households and then a list of hundred households was obtained as per serial numbers from one end to the other from each of these sites; Bajranganagar and Khursipar. These numbers were written in small pieces of papers and kept in two different bowls and named as Bajranganagar and Khursipar. From each of these two bowls 50 chits were picked up and kept separately for each of these two sites which finally formed the sample of this study [Table/Fig-1].
Sampling frame and sampling technique.
Determination of sample size: As a cross-sectional study the sample size was determined based on an estimated prevalence rate of knowledge among the slum population by using the formula 4PQ/L2 however, the same could not be arrived at owing to unavailability findings in similar areas in Chhattisgarh, India. Thus, the sample size was deliberately chosen and was kept to 100 households.
Data collection tool (the questionnaire): The tool used in this study was a structured questionnaire. The questionnaire was translated in to Hindi and then used to suite the local needs. Of the total 11 questions asked to assess the knowledge and behaviour, eight questions were asked to assess the knowledge of the people before and after the implementation of the awareness strategy. Similarly of the 11 questions three questions were asked to assess the behaviour regarding TB care before and after the implementation of the awareness strategy.
Implementation strategy: The health awareness strategy in this study was implemented after obtaining baseline information regarding the knowledge and attitude of the household members about TB and its services. Four trained community volunteers implemented the awareness intervention in two slum areas, each conducting 25 households, in both the phases. These community volunteers were previously trained on TB and are currently working in a similar project headed by the first author. After one month of the implementation of this awareness strategy the second round of survey was carried out among same households using the same questionnaire. The volunteers filled the questionnaire by asking questions to the available family members. Here the question was not targeted to a single family member rather the same was asked in front of all the available family in order to understand the knowledge and attitude and impart awareness among the family group. Each of these four volunteers spent at least 15 to 20 minutes in imparting awareness about TB, its symptoms, diagnosis, treatment and RNTCP services. The awareness was imparted orally and IEC materials were distributed containing similar information.
Results
The results of this research are presented in two different sections; assessment of knowledge and assessment of behaviour.
Assessment of knowledge: The knowledge section consists of eight questions which assessed the knowledge of household members regarding TB, its diagnosis and treatment facilities and preventive measures. The [Table/Fig-2] depicts the level of knowledge regarding TB, its diagnosis, treatment and preventive measures. Major improvements were observed on three knowledge indicators such as transmissibility, curability and preventability of TB which accounts to 17%, 16% and 25% respectively.
Impact of health awareness on knowledge level of participants.
| Sl No | Questions | Correct Responses (n=100) | Improvement of knowledge level (%) |
|---|
| Pre-Implementation | Post-Implementation |
|---|
| 1 | What Causes TB? | 95% | 95% | 0% |
| 2 | Does TB transmit from one person to other? | 82% | 99% | 17% |
| 3 | What are the modes of TB transmission? | 63% | 76% | 13% |
| 4 | What are the symptoms of TB? | 97% | 100% | 3% |
| 5 | Is TB curable? | 76% | 92% | 16% |
| 6 | Is TB treatment if free of cost at public health facilities? | 75% | 89% | 14% |
| 7 | Can TB be prevented? | 68% | 93% | 25% |
| 8 | What are the preventive measures of TB? | 91% | 97% | 6% |
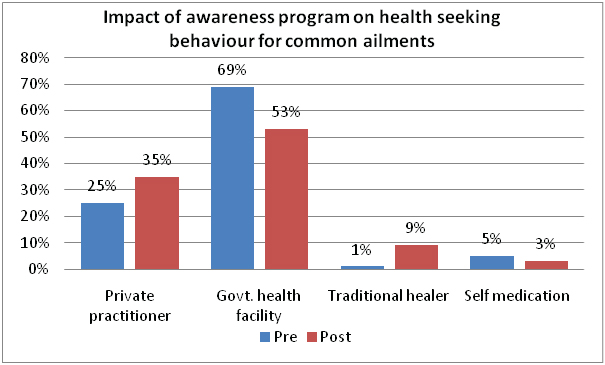
Assessment of behaviour: The health seeking behaviour of the household members was assessed by asking three behaviour related questions. The first question and second question elicited the health seeking behaviour of the household members regarding general ailment and TB respectively. The third question was asked to assess the factors behind not approaching government health facilities for TB care. The [Table/Fig-3] depicts the impact of awareness on health seeking behaviour of households for common ailments.
Impact of awareness program on health seeking behaviour for common ailments.
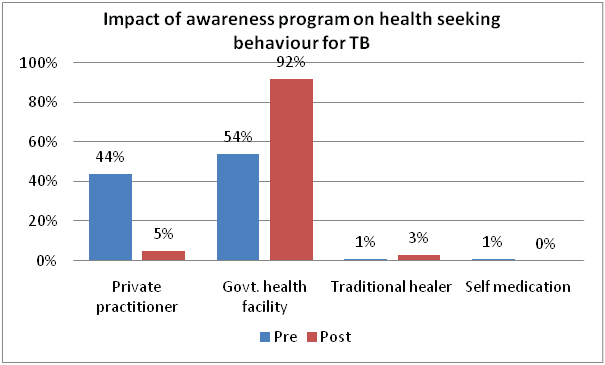
The [Table/Fig-4] depicts the impact of awareness program on health seeking behaviour of the household members for TB. After the implementation of the awareness strategy 44% of the participants agreed not to visit a private facility for TB treatment and 92% of the participants reported to visit government health facility for TB treatment.
Impact of awareness program on health seeking behaviour for TB.
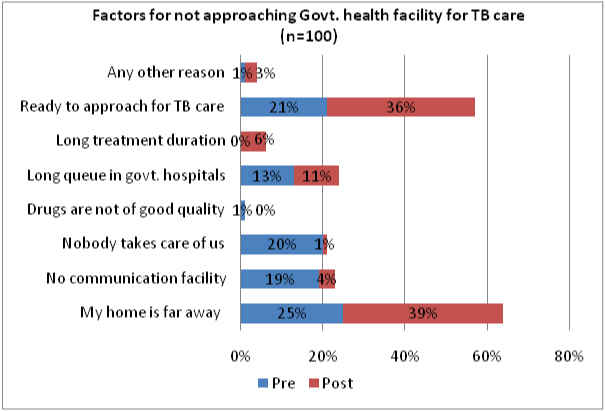
In the behaviour section the last question was asked to assess the factors behind not accessing government health facility for TB care, as TB control program being a freely available centrally sponsored program. The [Table/Fig-5] depicts several factors for not accessing the government health facility for TB care. Distance (25%), lack of communication facility (19%) and poor caring nature of government health staff (20%) were main stated reasons for not approaching government health facility. After the implementation of health awareness strategy 36% of the participants reported to approach government health facility for TB care.
Factors of not approaching the government health facility for TB care.
Discussion
The study was carried out in a slum area in order to understand the knowledge and behaviour of slum dwellers for TB care and thereby imparting a structured awareness strategy to increase their knowledge regarding TB and bring change in their behaviour for TB care.
Different studies reveal that people are aware of free treatment services of TB however, the score for this knowledge indicator is relatively poor compared to other knowledge indicators [10–14]. The knowledge level regarding the preventability of TB and preventive measures of TB got increased by 25% and 6% respectively among the respondents. Of the knowledge components the improvement was incurred above 90% among the respondents except in two components such as modes of TB transmission and availability of free treatment facilities. These two components are of paramount importance from the public health perspective. The correct knowledge regarding the modes of transmission can make people stay away from those practices which make them vulnerable for TB transmission.
Similarly, the knowledge regarding the availability of free treatment services is important from two perspectives. This, at one end will restrain people from accessing TB care services from private health facilities as free treatment is only available in public sector health facilities thus preventing them from poverty trap and treatment default after few weeks of treatment [15]. One of the research papers published in 2006 reveals that a TB patient spends 5,986 rupees out of his pocket for TB treatment resulting in a total spending of 13,000 crores per year in the country. The situation is further coupled with 11% of school dropout and 20% entry of children in to labour force in order to support the family if the breadwinner of the family is a TB victim [16].
In addition, a recent study reported that the estimated annual market for TB diagnostics in India is US$ 222 million, both the public and private sector, of which the private sector accounts to 62% [17]. Similarly, the consumption of anti-TB drugs is also huge in private sector. Of the total market of US$ 94 million for first line anti-TB drugs the private sector only consumes US$ 61 million [18]. Despite this more than half (50%-80%) of the TB patients seek medical care at private health facilities and TB treatment at private health facilities remains substandard [19–21]. Thus, the knowledge in both these components is of utmost importance which will help them in getting the right quality treatment and prevent them from impoverishment. Furthermore, the end TB strategy of World Health Organization also emphasizes that by 2035 no family should face catastrophic economic damage owing to TB [22,23]. The universal health coverage also envisages the removal of financial barrier and prevention of catastrophic economic damage [24].
Several studies have been carried out in different Indian communities and other parts of the globe regarding the impact of health education methods on TB [10–14]. One of the studies conducted among the high school children in Vellore, India, assessed the impact of a simple education method (audio visual/power point presentation) on TB. The mean pre-test score was 7.05 (64%) and the mean post test score was 9.15 (83.2%). Students attained significant knowledge in subjects related to treatment [10]. In another study in North India the impact of an IEC campaign undertaken by Government of India was studied. The core message regarding symptoms, diagnosis, treatment center, and free treatment was recalled correctly by 14.3%, 44.5%, 65.4%, and 89.2% of the respondents, respectively [11]. This indicates that simple IEC campaigns can impact greatly on families and help the family members take right preventive measures and take right decision for taking treatment help. A similar study in Mangaluru district of Karnataka, India, through a quasi experimental design assessed the impact of an intensive health education conducted at the District Tuberculosis Center (DTC) and at a private hospital. The study unraveled statistically significant impact on the health status of the patients after receiving the intensive health education between first and 30th day, 30th and 60th day, 60th and 90th day, and first and 90th day. Higher mean post-test knowledge scores, and a highly significant association between sputum conversion and adherence to treatment was reported [12]. Another school based interventional TB awareness programme in Pune city of India assessed the associated change in knowledge level among 135 secondary school students. The reported mean pre-test score was 6.31 (52.58%), and the mean post-test score was 10.20 (85%) [13]. A prospective interventional study in Tamil Nadu assessed the impact of a structured health education method among TB patients. The mean percentage change in knowledge, attitude and practice level was 41.32%, 21.61% and 18.94% respectively [14].
In the behavioural segment, regarding the health seeking behaviour of general health problems, significant level of behaviour change was not observed after the implementation of the awareness strategy as evident from the [Table/Fig-3] which shows that people said that they will visit more private practitioner and less public health facilities for general health problems. This might be due to two reasons; usually people presume that a private practitioner is the preferred choice for general health problems compared to TB for obvious reasons (protracted treatment duration) associated with both these conditions. Secondly, as awareness program was directed toward TB thus people would have presented their own preference of general health problems which is independent of TB awareness. However, this situation is opposite with the health seeking behaviour regarding TB among the same respondents, as depicted in [Table/Fig-4]. The behaviour changed in favour of the public health facilities and against the private health facilities which is a welcome move among these slum dwellers. This is utmost important owing to the above mentioned facts; it would protect households from impoverishment [16], prevent from treatment default [15] and protect them from substandard treatment at private health facilities [19–21].
In the third question, in behavioural component, the factors behind not accessing government health services for TB care were elicited. [Table/Fig-5] depicts the factors for not approaching government health facility for TB care. The study identified three important factors for not approaching the government health facility; communication problem, distance from home and dissatisfaction (nobody takes care of us) with the government health facility. Other studies conducted in different Indian communities also reveal similar factors for not accessing care for TB at government health facility; distance from home [25,26], lack of communication facility [27,28] and dissatisfaction with government health facility [27].
Limitation
The study was carried out in two different slums in Chhattisgarh. Moreover, the slum inhabitants have different socio-economic status compared to mainstream population. The knowledge and attitude of this population is also different from the mainstream counterpart thus, the results cannot be extrapolated to general population.
Conclusion
The study assessed the impact of a structured TB awareness program on the knowledge and behaviour among the slum dwellers in two of the slums of Durg District in Chhattisgarh. A considerable level of improvement was observed among the slum dwellers and a change in behaviour for accessing public health facilities for TB care could also be observed. Despite this, in the knowledge segment two important components have low level of improvement which requires further improvement. Thus, health education activities should be directed to improve the knowledge of slum dwellers regarding the modes of TB transmission and availability of free treatment at public health facilities.
| Annexure-1 |
| QUESTIONNAIRE: |
| Knowledge: |
| 1. How does TB spread? (Bacteria, Past deed/sin, effect of demon, all of these) |
| 2. Does TB transmit from one person to another? (Yes, No, May or may not, Do not know) |
| 3. How does TB transmit? (Cough/breath, sharing cups, sharing feeding materials, through body contact or sharing clothes, All of these, None of these) |
| 4. What are the symptoms of TB? (Persistent cough for two or more weeks, sputum with blood, chest pain, weight loss, loss of appetite, fever with sweating, All of these, None of these) |
| 5. Is TB treatable? (Yes, No, May or May not, Do not know) |
| 6. TB treatment is free of cost at public health facilities. (Yes, No, May or May not, Do not know) |
| 7. Can TB be prevented? (Yes, No, May or May not, Do not know) |
| 8. What are the preventive measures of TB? (Covering mouth and nose when coughing or sneezing, avoid sharing cups, using separate rooms, early treatment, avoiding body contact/hand shaking, All of these, None of these) |
| Behaviour: |
| 1. Where do you seek treatment when you fall sick? (Private practitioner, government health facility, traditional healer, self medication/over the counter purchase of medicine) |
| 2. What will you do if someone in your family or neighborhood develops TB symptoms? (Private practitioner, government health facility, traditional healer, self medication/over the counter purchase of medicine) |
| 3. Why should not you visit government health facility as TB treatment is free of cost? |
| a. My home is far away from government health facility |
| b. There is no communication facility |
| c. In government hospital nobody takes care of us |
| d. The government medicines are not of good quality |
| e. There is long queue in government hospital |
| f. Govt. staff ask money for treatment |
| g. The treatment duration is long in government hospital |
| h. Ready to approach government hospital for TB care |
| i. Any other reason |