Introduction
Colorectal cancer is cancer of the large intestine, the lower part of digestive system which includes the sigmoid colon and rectum.
Aim
To study the relation of incidence of colorectal cancer with previous gall bladder disease or post-cholecystectomy status, a relation between gall bladder disease and smoking in particular and the most common region of colon involved in colorectal cancer in gall bladder disease and non-gall bladder disease patients.
Materials and Methods
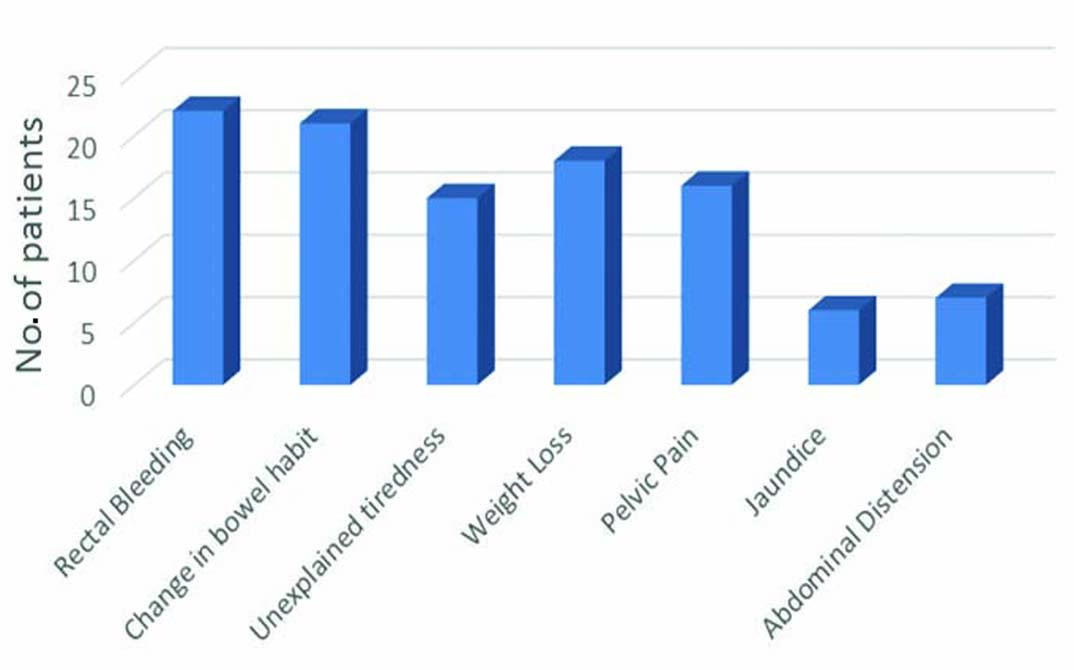
A total of 256 patients with symptoms of rectal bleeding, change in bowel habit, unexplained tiredness, weight loss, pelvic pain, jaundice and abdominal distension were screened by using colonoscopy among whom 30 patients were diagnosed with colorectal cancer. Detailed history was taken with the help of a modified questionnaire and the patients were assessed, examined and the list of investigations such as faecal occult blood test, ultrasound of abdomen and pelvis, colonoscopy, sigmoidoscopy, barium enema, Computed Tomography (CT), Magnetic Resonance Imaging (MRI) of the abdomen and pelvis, tumour markers like Carcinoembryonic Antigen (CEA) and biopsy were collected. Patient pool was categorized into Gall Bladder Disease (GBD) and Non Gall Bladder Disease (NGBD). Proportions test and Fisher’s-Exact test were used to calculate the p-values.
Results
Ten patients had previous gall bladder disease (33%) which was significant with a p-value of 0.016 by proportions test. Two patients underwent cholecystectomy, two patients underwent Endoscopic Retrograde Cholangio Pancreatography (ERCP) and the remaining six patients did not take any treatment for their gall bladder disease. Five patients with previous gall bladder disease were found to be smokers with a p-value of 0.091. The average age was 47.2 years in males and 42.2 years in females. Males constituted 66.6% (20 males) of the diseased population whereas, females constituted 33.4% (10 females). Rectal bleeding and altered bowel habits were the commonest symptoms. Confirmation of the disease was proven using CT abdomen and biopsy. Right sided colorectal cancer was common in GBD patients. Left sided colon cancer was common in NGBD patients.
Conclusion
This study established a statistically significant risk of colorectal cancer following cholelithiasis though no risk was apparent following cholecystectomy.
Introduction
Colorectal cancer is the third most common cancer in men (663000 cases, 10% of all cancer cases) and the second most common in women (5710000 cases, 9.4% of all cancer cases). In India, the annual incidence rates for colon cancer in men are 4.4 per 100,000 and in women it is 3.9 per 100000 [1]. Genetic factors play a major role in the development of colorectal cancer. Among the colonic polyposis syndromes, Familial Adenomatous Polyposis (FAP) and its variants like Turcot’s syndrome, Gardner syndrome and attenuated FAP and MYH-associated polyposis are the most common. Hereditary non-polyposis colon cancer or Lynch syndrome comprises the non-colonic polyposis category [1].
Gallstones are strongly associated with increased risk of colorectal cancer through diet. Gallstones are largely made up of cholesterol therefore any link between gallstones and colorectal cancer lends an argument to the hypothesis for the causation of bowel cancer. The presence or absence of gallstones proves to be a reliable indication of cholesterol burden and has been earlier positively correlated with colon cancer [2]. A diet high in red meat and animal fat, low-fibre diets, and low overall intake of fruits and vegetables are linked with increased risk of colorectal cancer [3]. Gallstones can lead to inflammation of the gallbladder, biliary tract ducts, liver and pancreas therefore the link between inflammation and cancer is well established, hence, gallstones could increase the risk of a number of different digestive system cancers. Cholecystectomy, though it reduces the inflammatory state associated with gallstones also increases the exposure of the small intestine, stomach and oesophagus to bile. This changes the metabolic hormone levels and increases the cancer risk in digestive system organs like colon and rectum [4].
The risk for colorectal cancer is explained by the higher turnover of bile acids and its bacterial degradation which increases the proportion of secondary bile acids in the bile and thus in the large intestine. The mitotic index of colonic mucosa, as indicator of cell proliferation increases after cholecystectomy. People seeking medical care for gall stone disease are more likely to undergo a cholecystectomy and also tend to visit a doctor earlier for symptoms of colorectal cancer [5].
Ulcerative colitis, long term immunosuppression following organ transplantation, diabetes mellitus, alcohol consumption, obesity, cigarette smoking, use of androgen deprivation therapy, acromegaly and ureterocolic anastomosis are also some of the aetiological factors [1].
Clinical symptoms include a change in bowel habit for left-sided colorectal cancer because faecal contents are liquid in the proximal colon and lumen calibre is larger and therefore less likely to be associated with obstructive symptoms. Haematochezia is more often caused by rectosigmoid than right sided colon cancer. Iron-deficiency anaemia is common with right sided colorectal cancer [6]. Abdominal pain can be caused by partial obstruction, peritoneal dissemination and intestinal perforation leading to generalized peritonitis. Rectal cancers also cause tenesmus, rectal bleeding, and rectal pain and diminished stools [6].
Once a colorectal cancer is suspected, next test can be a colonoscopy, barium enema or CT colonoscopy. Colonoscopy is a fairly accurate test used for detection and biopsy of lesions throughout the large bowel. When viewed through the scope, most colorectal cancers are endoluminal masses that arise from the mucosa and protrude into the lumen. Masses may be exophytic or polypoid. Bleeding may be seen with lesions that are friable, necrotic or ulcerated. Circumferential involvement of the bowel correlates with the apple core description on radiologic imaging. CT colonography has superior patient acceptability compared with colonoscopy in the short term but the benefits of colonoscopy become apparent after long term follow up. Hence, colonoscopy remains the gold standard for investigation of symptoms suggestive of colorectal cancer. Serum levels of CEA have prognostic utility in patients with newly diagnosed colorectal cancer. Patients with preoperative serum CEA>5 ng/ml have a worse prognosis [6].
No Indian study with a similar outlook has been done in the past which makes this endeavour significant. Hence, the present study aimed to analyze the relation of incidence of colorectal cancer with previous gall bladder disease or post-cholecystectomy status, to study a relation between gall bladder disease and smoking in particular and to study the most common region of colon involved in colorectal cancer in both gall bladder disease and non-gall bladder disease patients.
Materials and Methods
The study was a prospective clinical study conducted on patients present in the inpatient wards of medical gastroenterology, surgical oncology, surgical gastroenterology, medical oncology and radiation oncology at Vydehi Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India, during the period from July 2016 to October 2016. The study was conducted after obtaining an informed and understood consent from all the patients. Two hundred and fifty six patients were screened for the following inclusion and exclusion criteria:
Inclusion Criteria
Patients presenting with abdominal and bowel symptoms like rectal bleeding, change in bowel habit, unexplained tiredness, weight loss, pelvic pain, jaundice and abdominal distension who have undergone colonoscopy [Table/Fig-1].
Age 25-80 years.
Common symptoms-from left to right.
Exclusion Criteria
Patients diagnosed with colon polyp.
Family history of colorectal cancer.
Those who fulfilled the criteria and volunteered to participate, after giving written informed and understood consent were enrolled in the study. The study was started after obtaining approval from Institutional Ethics Committee. Detailed history was taken with the help of a modified questionnaire prepared by the authors based on their clinical experience and the patients were assessed, examined and the list of investigations such as faecal occult blood test, ultrasound abdomen and pelvis, colonoscopy, sigmoidoscopy, barium enema, CT and MRI of the abdomen and pelvis, tumour markers like carcinoembryonic antigen and biopsy were collected. The study was conducted based on the following parameters:
Abdominal and bowel symptoms, time period of symptoms, reports of patients who have undergone investigations were collected. History of previous gall bladder disease, family history of cancer, history of cholecystectomy or ERCP procedure, history of current or past treatment, history of diabetes mellitus Type-II, history of hypertension, history of smoking and history of alcoholism was elicited. General physical examination and systemic examination were performed on all patients.
Statistical Analysis
Patient pool was categorized into GBD and NGBD. Proportions test and Fisher’s-Exact test were used to calculate the p-values.
Results
Two hundred fifty six patients underwent colonoscopy/sigmoidoscopy of which 30 patients were diagnosed with colorectal cancer. Only 10 out of 30 patients had previous gall bladder disease (33%) which was found to be significant with a p-value of 0.016 by proportions test (assuming a population prevalence of 50%).
Five out of 10 patients with previous gall bladder disease were found to be smokers. Six out of 20 patients with non-gall bladder disease were found to be smokers. Fisher’s-Exact test was used to determine any association between gall bladder disease and smoking. The p-value was found to be 0.091 and hence, it was concluded that there is no association between gall bladder disease and smoking.
The commonest time period in which patients presented with symptoms were two to five months and 6-12 months.
All the patients underwent colonoscopy, ultrasound, Contrast Enhance Computed Tomography (CECT) abdomen, biopsy, complete blood count and electrolytes whereas, very few patients underwent sigmoidoscopy and MRI abdomen.
Most of the patients underwent surgery or chemotherapy.
Ten patients had gall bladder disease. Two patients underwent cholecystectomy. Two patients underwent ERCP.
Discussion
Many studies have shown an association between colorectal cancer and gall bladder disease but not with cholecystectomy. This study intended to identify such an association in the Indian population.
In our study, the average age was 47.2 years in males and 42.2 years in females. This is in accordance with a study conducted by Yamaji Y et al., where the mean age was 46.1 years [7]. The inference is that old age is not the only reason responsible for colorectal cancer. It can occur in middle age too.
In our study, 20 males (66.6%) had the disease and 10 females (33.4%) had the disease [Table/Fig-2]. This is in accordance with a study conducted by Seydaolu G et al., in which 55.5% of colorectal cancer patients were males and 44.5% of patients were females [8].
Baseline characteristics.
| Criteria | Number of patients |
|---|
| Age (years) |
| 25-55 | 21 |
| 56-80 | 9 |
| Sex |
| Males | 20 |
| Females | 10 |
| Region involved |
| Ascending and transverse colon | 11 (7 had previous gall bladder disease) |
| Descending colon and rectum | 19 (3 had previous gall bladder disease) |
In a study conducted by Hamilton W et al, positive predictive value for rectal bleeding was 2.4% (1.9, 3.2). Diarrhoea and constipation had lesser positive predictive value but when combined with one more symptom significantly increased the risk of colorectal cancer. In our study, 22 patients presented with rectal bleeding and 21 patients presented with altered bowel habit. The studies suggest that these two symptoms are mainly noticed by the patients and can be considered as warning symptoms [9].
In a study conducted by Boyle P et al, the inference is that colonoscopy is a strong screening tool compared to investigations like faecal occult blood test for reducing the incidence of colorectal cancer. In our study, the commonest investigation was colonoscopy, CT abdomen and biopsy [10].
In a study conducted by Chiong C and Cox MR et al., they studied the relationship between cholelithiasis, cholecystectomy and colorectal cancer using a random effects model. This study established that there was a statistically significant risk of rectal cancer following cholelithiasis though no risk was apparent following cholecystectomy [11].
Results of our study suggest an increased incidence of colorectal cancer in patients of previous gall bladder disease. Also, right sided colorectal cancer is commoner in the previous GBD patient group and in NGBD the left side of the colon is more commonly involved.
In a study conducted by Jorgensen T et al., a non-significant trend was also established toward more right-sided cancers in patients with gallstones than in patients without. These results gave substantial evidence for an association between gallstones and colorectal cancer, an association which is not due to cholecystectomy being a predisposing factor to colorectal cancer [12].
Studies conducted by Lin HL et al., showed that patients with cholecystitis and cholangitis had a significantly higher risk of contracting colorectal cancer compared to patients without them. They concluded that excessive production of bile acid during the inflammatory process in the gall bladder and bile duct played an important role in colorectal carcinogenesis. Also, no significant difference in the risk of colorectal cancer between biliary tract inflammation patients who did and did not undergo cholecystectomy was observed [13].
Colorectal cancer was confirmed in all the 30 cases by colonoscopy and biopsy. Necessary investigations as and when required needs to be done for staging and treatment.
Limitation
Detailed history was taken with the help of a modified questionnaire prepared by the authors based on their clinical experience. No specific validation was done. Also, the sample size is small. More studies have to be done with a larger sample size to establish a causal association.
Conclusion
This study established that there was a statistically significant risk of colorectal cancer following cholelithiasis though no risk was apparent following cholecystectomy.
The fact that most studies concur with our study inferring that right sided colorectal cancer is commoner in GBD patients, it is prudent to hypothesise a causal association between the two.
Whether the finding is attributable to the gall bladder disease itself or is just an associated finding is difficult to be commented on as the sample size is small. More studies have to be done with a larger sample size to establish a causal association.
Through this study, we propose routine follow up of patients with gall bladder disease for early detection and appropriate treatment of incident colorectal cancer.
Abbreviations
ERCP-Endoscopic Retrograde Cholangiopancreatography
GBD-Gall Bladder Disease
NGBD-Non Gall Bladder Disease
FAP-Familial Adenomatous Polyposis
MYH-Mutations in MYH Gene
CEA-Carcinoembryonic Antigen
CECT-Contrast enhanced computed tomography
CT-Computed Tomography
MRI-Magnetic Resonance Imaging
[1]. Indian Council of Medical Research. Consensus document for management of colorectal cancer. [cited 2015 Sep 2] Available from: http://www.icmr.nic.in/guide/cancer/Colorectal/Colorectal%20Cancer.pdf [Google Scholar]
[2]. Lowenfels AB, Gallstones and the risk of cancerGut 1980 21:1090-92. [Google Scholar]
[3]. Aune D, Chan DS, Lau R, Vieira R, Greenwood DC, Kampman E, Dietary fibre, whole grains and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studiesBMJ 2011 343:d6617 [Google Scholar]
[4]. Nogueira L, Freedman ND, Engels EA, Warren JL, Castro F, Koshiol J, Gallstones, cholecystectomy and risk of digestive system cancersAm J Epidemiol 2014 179(6):731-39. [Google Scholar]
[5]. Goldbohm RA, van den Brandt PA, van’t Veer P, Dorant E, Sturmans F, Hermus RJ, Cholecystectomy and colorectal cancer: Evidence from a cohort study on diet and cancerInt J Cancer 1993 53(5):735-39. [Google Scholar]
[6]. Finlay A Macrae, Johanna Bendell. Clinical presentation, diagnosis, and staging of cancer. [cited 2015 Oct 15] Available from: http://www.uptodate.com/contents/clinical-presentation-diagnosis-and-staging-of-colorectal-cancer. Accessed on October 15th, 2015 [Google Scholar]
[7]. Yamaji Y, Okamoto M, Yoshida H, Kawabe T, Wada R, Mitsushima T, Cholelithiasis is a risk factor for colorectal adenomaAm J Gastroenterol 2008 103(11):2847-52. [Google Scholar]
[8]. Seydaolu G, Özer B, Arpacı N, Parsak CK, Eray IC, Trends in colorectal cancer by subsite, age, and gender over a 15-year period in Adana, Turkey: 1993-2008Turk J Gastroenterol 2013 24(6):521-31. [Google Scholar]
[9]. Hamilton W, Round A, Sharp D, Peters TJ, Clinical features of colorectal cancer before diagnosis: A population-based case–control studyBr J Cancer 2005 93(4):399-405. [Google Scholar]
[10]. Boyle P, Leon ME, Epidemiology of colorectal cancerBr Med Bull 2002 64(1):1-25. [Google Scholar]
[11]. Chiong C, Cox MR, Eslick GD, Gallstone disease is associated with rectal cancer: A meta-analysisScand J Gastroenterol 2012 47(5):553-64. [Google Scholar]
[12]. Jorgensen T, Rafaelsen S, Gallstones and colorectal cancer-there is a relationship, but it is hardly due to cholecystectomyDis Colon Rectum 1992 35(1):24-28. [Google Scholar]
[13]. Lin HL, Lin HC, Lin CC, Lin HC, Increased risk of colorectal cancer among patients with biliary tract inflammation: A 5-year follow-up studyInt J Cancer 2010 28(2):447-52. [Google Scholar]