Osteoporosis is among the most serious health problems. Osteoporosis is a major disease that connected with high trauma and/or fragility fracture in various countries worldwide [1]. The elderly population is increasing. This is attributed to the increasing life span, making this population more vulnerable to bone fracture. The incidence of hip fracture was reported by 1.66 million cases in 1990 and it is estimated to increase to 6.26 million in 2050 [2]. The overall prevalence of osteoporosis in Asian population is higher than the Western countries due to the fact that the Asian population has a lower BMI and shorter height. The prevalence of osteoporosis in Malaysia was reported as 24.1% in 2005, predominantly affecting the hip. According to ethnic background, the rates of hip fracture have been increased in Chinese and Malays compared to Indian people [3]. However, many factors affect the bone health and the anticoagulant drugs such as warfarin is one of them. The mechanisms by which this drug affects the skeleton have been poorly understood [4]. In the elderly, indication of warfarin remains the main prevention of ischemic stroke secondary to atrial fibrillation which has a prevalence of 15% in that population and is an independent risk factor for ischemic stroke [5]. Warfarin is an antagonist vitamin K which acts as a co-factor in the carboxylation of glutamic acid (a specific amino acid) to form a modified amino acid, Gamma Carboxyglutamic Acid (GCGA). In fact, without this step of carboxylation, plasma proteins would not work in their part of regulating calcium fixations in different tissues. There are several types of GCGA proteins including Osteocalcin (OC) which is the most abundant GCGA protein in humans and is synthesised in the bone. The GCGA protein contains blood coagulation factors that are synthesised in the liver and the Matrix GCGA Proteins (MGP) are synthesised in the cartilage and in the vessel walls of the arteries [6]. Previous studies reported controversial results regarding the effect of warfarin on bone health [7], which showed that there was no significant effect of warfarin on lumbar or hip BMD. However, another study reported that warfarin-induced impairment of cortical bone material quality and compensatory adaptation of cortical bone structure to mechanical stimuli [8]. On the other hand, another study showed that there was no significant association between long-term warfarin use and fracture risk, despite the biological plausibility [9]. This study used a Quantitative Ultrasound (QUS) technology which was less expensive and more portable than Dual-energy X-ray Absorptiometry (DXA) and it also had the advantage of the unnecessary use of ionizing radiation, so it was safer. Moreover, there was strong evidence that QUS measurements were useful indicators of bone structure [10]. Historically, calcaneus was the first site to be investigated through QUS [11]. Researchers investigating osteoporosis by means of using QUS and they have reported favourable results [10].
This study aimed to use the QUS as an alternative approach for bone health assessment. The goals of this study were to assess the osteoporotic conditions in warfarin users using QUS, and to assess the risk factors influencing the BMD such as the demographic data and the current treatment.
Materials and Methods
A case-control study was conducted, from November 2013 to July 2014, to assess the risk factors of osteoporosis in warfarin users and non-users. The QUS method has been developed and introduced in the recent years for the assessment of skeletal status. Patients who reported, using warfarin for at least one year were selected from Hospital Pulau Pinang and the control group was healthy volunteers (non-users of warfarin). This study included participants who are more than 18-year-old for both groups. All respondents must be able to read and write in Bahasa Malaysia to answer the questionnaire. For both men and women, the exclusion criteria were: prolonged immobility (one-two year), chronic diseases for the control group, gastrointestinal/nutritional conditions, cancer or history of chemotherapy or radiation therapy, endocrine disorders like hyperparathyroidism, hypogonadism, hyperthyroidism, Cushing’s disease, prolactinoma, acromegaly, adrenal insufficiency and prolonged secondary amenorrhea, psychiatric diseases, haematological diseases, recent surgery and bone fracture, rheumatologic diseases, patients on chronic medications with drugs known to interfere with calcium metabolism such as corticosteroids, thyroid hormone, or active vitamin D3, bisphosphonates, calcitonin injection, oestrogens, steroids, thyroid hormone, Hormone Replacement Therapy (HRT) or anticonvulsants, nursing or pregnant women, patients with history of osteoporosis and/or use of medications for osteoporosis. The ethical approval was granted from the National Institutes of Health (NIH), Ministry of Health Malaysia. The number of research is NMRR-13-1281-18077 (IIR).
Sampling and Sample Size
A convenience sampling method was used to obtain the required sample size for this study. For the warfarin users, the sample was conveniently selected from the outpatients clinic at Hospital Pulau Pinang. While the control group (non-users warfarin) was selected from the community for being a part of this study. The sample size was calculated based on the sample size of unmatched case-control studies [11]. According to previous study, the prevalence of osteoporosis in warfarin users was 13.9% and the non-users was 9.2% [12]. While, the hip fracture was estimated to be 16% in women and 6% in men [13], which is similar to Malaysia in 2005 that was 24%. The level of statistical significance (α) and power of study (1-β) used were 0.05 and 0.8, respectively. The sample size was calculated according to unmatched case-control sample size calculator indicated that the required sample size is 128 in each group. In addition, 20% was added to study sample in case of missing or incomplete data. In total, the sample size was 151 in each group.
Quantitative Ultrasound and Socio-demographic Data
In fact, the QUS methods have been proposed as an alternative in the evaluation of bone status. The Speed of Sound in meters per second (SOS m/s) and Broadband Ultrasound Attenuation (in BUA decibels per megahertz), was used as a measure of frequency-dependent attenuation of the ultrasound wave passing through the heel [14]. The Stiffness Index (SI), a variable derived from a combination of SOS and BUA, was calculated by the analysis software according to the equation below:
SI= 0.67 BUA + 0.28 SOS – 420
Higher SI indicates higher BMD [15]. Quality control measurements of the QUS device will be carried out daily by means of a phantom provided by the manufacturer according to World Health Organization (WHO) criteria with regard to T-score and analyses of BMD (g/cm2). T-score is defined as the number of Standard Deviations (SD) above or below the mean using young-adult reference data. Normal BMD with T-score greater than –1, osteopenia with T-score of –1 to –2.5 and osteoporosis with T-score of less than –2.5 were considered as the measurement basis [16], while Z-score expressed relative to normal people of the same age, or compared with young normals. It is the latter comparison (frequently designated the T-score) which relates more closely to fracture risk. Medicare rebate eligibility is related to both T and Z score, after the QUS parameters measured the background questionnaire including demographic questions on race, gender, age, employment status, marital status, education level, family history of osteoporosis or fractures, and financial status were included in the current study.
Statistical Analysis
The data were analyzed by using SPSS software (version 20.0 for Windows). The results were expressed as a mean with 95% confidence limits or SD. A p-value of <0.05 was considered significant. The association between categorical variables was analyzed by using Chi-square test. Pearson’s correlation coefficient used to describe continues risk factors. An independent sample t-test was used for comparing two means variables that were normally distributed. Logistic regression analysis was used to find the Odd Ratio (OR). Two-way ANOVA test was used to find factors that were affected due to interaction between the categorical variables [17].
Results
QUS parameters were performed on 130 patients who were using warfarin more than one year. The sample consisted of 52% females and 48% males with the mean age of 65.06±11.37 years old. The mean duration of treatment with warfarin was 46.32±43.032 months with a range between 13–264 months. The daily dose of warfarin ranged from 1.0–7.0 mg with a mean of 2.91±1.32 mg/day. The INR ranged from 1.1-7.3 with a mean of 2.52±0.82. In addition, the control group included 140 subjects as non-users of warfarin. The control group consisted of 58% females and 42% males with a mean age of 46.65±14.551-year-old. The prevalence of the abnormal BMD for both groups was 76.7% as having a high risk of abnormal BMD which includes osteopenia and osteoporosis. On the other hand, 23.3% were identified as having a low risk of abnormal BMD. There were significant differences of the mean values for BMI, T-score, SI, and Z-score between warfarin users and non-users as shown in [Table/Fig-1].
Characteristics of study sample in both groups (270 participants).
| Warfarin users(n = 130)mean±SD | Non warfarin users(n = 140)mean±SD | Sig |
|---|
| Age (years) | 65.06±11.370 | 46.65±14.551 | |
| BMI (kg/m2) | 24.49±4.626 | 26.86±5.168 | 0.001* |
| Warfarin dose (mg/day) | 2.91±1.327 | - | |
| Warfarin duration (months) | 46.32±43.032 | - | |
| INR | 2.522±0.824 | - | |
| T-score | -1.81±0.890 | -1.55±0.994 | 0.025* |
| Z-score | -0.78±1.401 | - 1.28±2.532 | 0.050* |
| SI-score | 58.99±17.74 | 49.86±19.36 | 0.001* |
*t-test Significant (p-value <0.05); BMI, body mass index; INR, international normalization ratio; SI, stiffness index
From [Table/Fig-2], it was found that there was no significant association in both groups with the gender and race, p>0.05. This means that this study has no bias of selecting group (warfarin users and non-users) regarding the gender and race.
Risk factors of OP among users and non users warfarin according to demographic characteristics of respondents (n=270).
| Risk factors | | Non-users140 | Users130 | p-value |
|---|
| Race | Malay | 37.1% | 41.5% | NS |
| Chinese | 27.9% | 34.6% |
| Indian | 35.0% | 23.8 % |
| Family history of OP | No | 89.3% | 76.9% | 0.006* |
| Yes | 10.7% | 23.1% |
| Age group | ≥50years | 55.0% | 9.2% | 0.001* |
| <50 years | 45.0% | 90.8% |
| Menstrual period | Pre | 56.8% | 11.8% | 0.001* |
| Post | 56.8% | 88.2% |
| Family history fracture | No | 86.4% | 70.8% | 0.002* |
| Yes | 13.2% | 29.2% |
| Gender | Male | 42.1% | 47.7% | NS |
| Female | 57.9% | 52.3% |
* Chi-square significant (p-value <0.05); OP - osteoporosis; NS - not significant
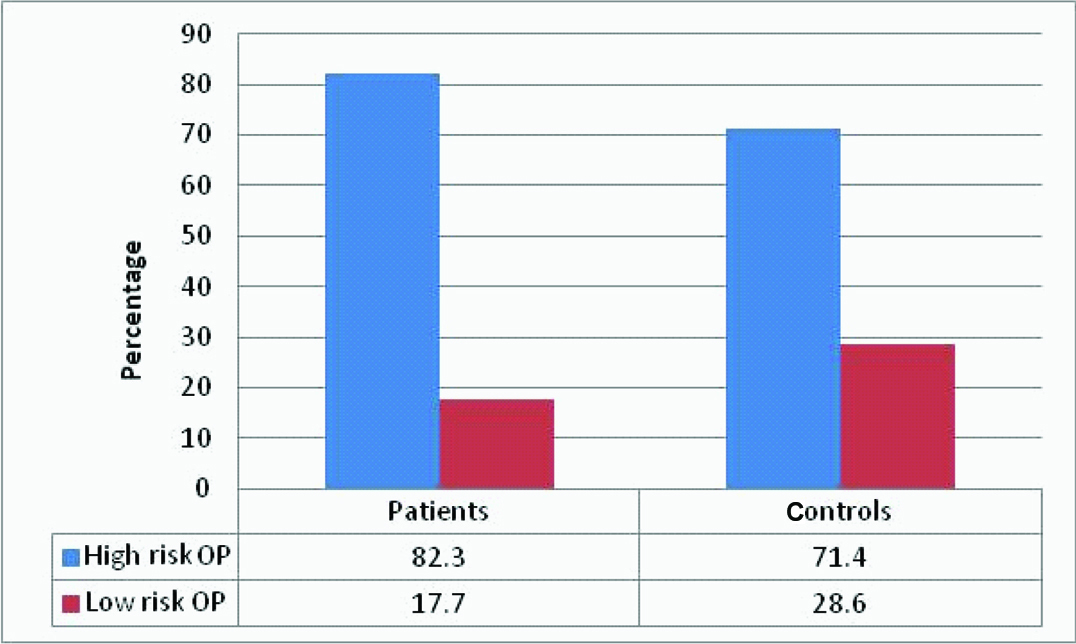
From [Table/Fig-3] the incidence of the risk of osteoporosis showed that 82.3% of warfarin users and 71.4% of non-users at higher risk of OP. While only 28.6% of the non-users have a lower risk of osteoporosis.
Incidence of osteoporotic condition among warfarin and non warfarin users (n=270).
OP= Osteoporosis
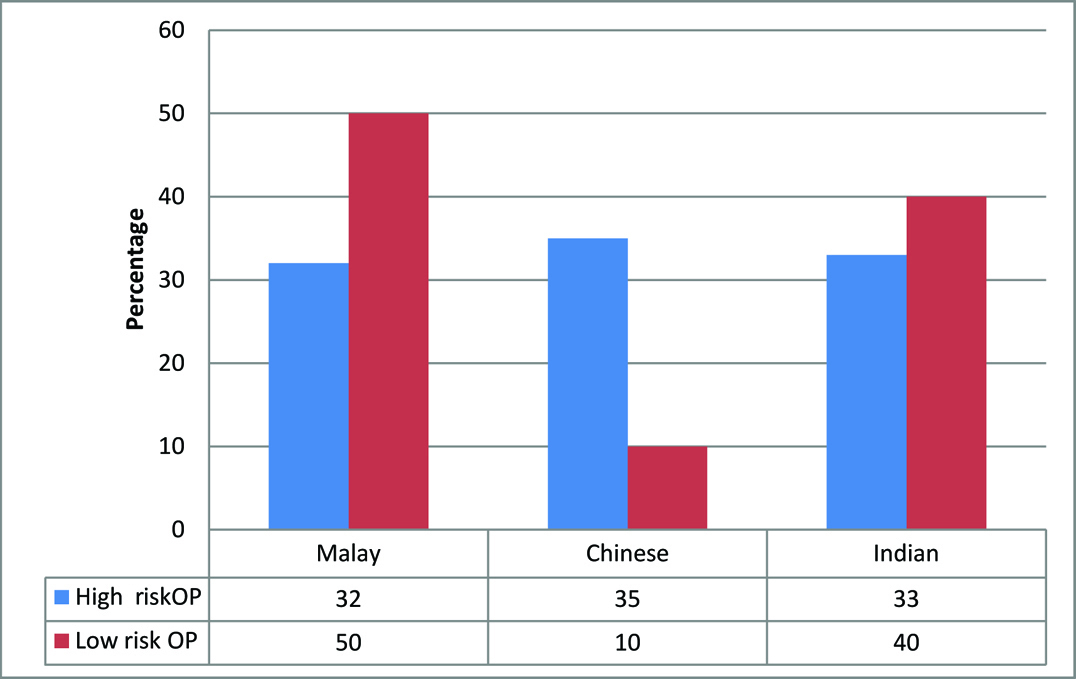
From [Table/Fig-4] the prevalence of osteoporotic condition between ethnic backgrounds of non-users warfarin showed that around 35% of Chinese have high risk of compared to Malay (32%) and Indian (33%). In addition, 50% of Malay participants were at low risk of osteoporosis.
Prevalence of osteoporotic condition between ethnicity group for non users warfarin group. (n=140).
From [Table/Fig-5], there were significant differences of the mean value of T-score between age, race, use of warfarin, family history Osteoporosis and family history of fracture. The older age, warfarin users, Chinese participants, family history of fracture and family history of Osteoporosis were more likely to have risk of osteoporosis (p<0.05). The results also showed that there was no significant correlation between T-score and the INR and duration of therapy. The only meaningful correlation was found between T-score and age, BMI, and warfarin dose (r=-0.314, p=0.001), (r=0.175, p=0.004), (r=-204, p=0.020), respectively.
Risk factors of Osteoporosis among the sample of the study (n=270).
| Risk factor (n) | Mean±SD | p-value |
|---|
| Age |
| ≤ 50 years (89) | -1.358±1.019 | 0.001* |
| > 50 years(181) | -1.838±0.878 |
| Use of warfarin |
| No (140) | -1.553±0.994 | 0.025* |
| Yes (130) | -1.813±0.890 |
| Race |
| Malay(106) | -1.553±0.862 | 0.001** |
| Chinese(84) | -2.027±0.965 |
| Indian(80) | -1.477±0.965 |
| Family history of fractures |
| No (213) | -1.579±0.965 | 0.001* |
| Yes (57) | -2.047±0.847 |
| Family history OP |
| No (225) | -1.590±0.950 | 0.001* |
| Yes (45) | -2.120±0.835 |
*t-test significant (p-value <0.05); **One way AVOVA; OP, osteoporosis
From [Table/Fig-6], Two-way ANOVA tests showed that the interaction of risk factors of Osteoporosis (13% of adjusted R square) could be explained by the warfarin use with race and warfarin use with age (p<0.05). Considering the interaction of three factors showed that 12% of Adjusted R square could be explained by warfarin use with age and race together (p<0.001). The Chinese participants who aged more than 50-year-old and use warfarin were more likely to have the risk of OP.
Predictors of chronic warfarin therapy (n=130).
| Mean Squaret-score | df | F | Sig |
|---|
| Use* race |
| Malay | - 1.78±0.83 | 4 | 2.837 | 0.025* |
| Chinese | -1.96±0.84 |
| Indian | - 1.62±1.03 |
| Use * age |
| ≤50 year | -1.92±0.82 | 2 | 5.949 | 0.003* |
| >50 year | -1.80±0.89 |
| Use * family history OP |
| No | -1.74±0.88 | 2 | 0.372 | 0.690 |
| Yes | -2.04±0.87 |
| Use * family history fracture |
| No | -1.69±0.90 | 2 | 2.172 | 0.116 |
| Yes | -2.11±0.78 |
| Use * age>50 *race |
| Malay | -1.74±0.81 | 10 | 3.958 | 0.001* |
| Chinese | -2.07±0.86 |
| Indian | -1.66±0.91 |
* t-test significant (p-value <0.05); OP-osteoporosis
Discussion
This study showed a high prevalence of osteoporosis risk in the study sample. There was a significant association between the incidence of long-term warfarin use and risk of osteoporosis which later lead to fractures, suggesting that warfarin use itself need to increase prophylactic therapy for osteoporosis in elders on long-term therapy. This study found that the chronic utilization of warfarin leads to the reduction in BMD with risk of osteoporosis than the non-users of warfarin. Previous studies on warfarin use and fracture risk had conflicting results. In one of the earliest study conducted by Simon RR et al., on the rat showed that a month of treatment with sodium warfarin was found to increase osteoclast numbers while decreasing the number and activity of osteoblasts. These findings regarding the effects of warfarin are similar to the effects of glucocorticoids and heparin on the bone [18]. However, a previous study found a greater than twofold higher age- and sex-adjusted standardized incidence of both spinal and rib fractures compared with incidence rates in the general population with incidence of venous thrombosis [19].
As further research and analysis on warfarin treatment was carried out, results showed that using warfarin for more than three months does not decrease vertebral and rib fracture. The risk was two-fold greater for patients, who used warfarin for >12 months. It is worth mentioning that patients included in this research previously had venous thrombosis. They also received anticoagulation therapy. In the National Atrial Fibrillation Registry in the USA, research on warfarin use by over 68-year-old males and females was carried out. Warfarin use prior to atrial fibrillation index hospitalisation was tested using regular INR monitoring plus medical record of warfarin. Results showed that hip, wrist, spine, and rib fractures were estimated at index hospilatisation and follow up visits. Overall, warfarin use ≥one year was associated with 25% increased risk of any fracture, but on examination of specific fracture sites, associations were only found with spinal and rib fractures. In analyses stratified by sex, an association was noted only in men [20].
This study indicated a significant correlation found for osteoporosis risk factor with the higher dosage of warfarin. In another case-control study conducted by Danish National Health Service Registry, results indicated that there exists only a small fracture risk increase related to low dose warfarin use compared to non warfarin use. According to the authors, the reason behind the high fracture risk might be attributed to oral anticoagulant use clinical indication such as atrial fibrillation and venous thrombosis. This indicates that the underlying condition could have made osteoporosis patients more vulnerable to risks of bone fractures rather than the pharmacological effect of the anticoagulant [21]. This study concluded that the risk factors of osteoporosis were affected by age, menstrual period, family history of osteoporosis and family history of fractures. On the other hand, several studies have failed to find an association of warfarin use and fracture risk. In a population-based cohort study of 6,000 ambulatories, mostly white women 65 years of age and older or use <90 days in the five to seven years preceding the index date with risk of non-vertebral osteoporotic fractures [9].
Limitation
This study is limited to the size of the sample, that large sample of patients will demonstrate more risk factors and the impact of each factor on BMD. In addition, this case control study explained the risk factors of osteoporosis between warfarin users and no-users. Therefore, future exploration with longitudinal studies are needed to evaluate the relationship between oral anticoagulants and the risk of osteoporosis.
Conclusion
Considering the advantage of pre-schedule identification of osteoporosis, it is proposed that patients on long term warfarin use ought to be considered for the reduction of bone density test. The risk among the patients group was higher than those in the control group, where the patients showed a negative correlation with a higher dose of warfarin intake and age. Additionally, it is unequivocally proposed for the prophylactic utilization of calcium–vitamin D supplements for these patients. The clinical finding of this study will provide the fundamental basis for health care professionals to understand the logical and the appropriate utilization of health services in the management of osteoporosis in Malaysia. The study outcomes will lead to better patient care, enhance patient quality of life, and avoid possible adverse effects. Findings revealed that the pharmacist supervisor at the hospital should provide a sufficient degree of awareness to patients who are taking warfarin for treatment exchange according to patients INR ratio.
*t-test Significant (p-value <0.05); BMI, body mass index; INR, international normalization ratio; SI, stiffness index
* Chi-square significant (p-value <0.05); OP - osteoporosis; NS - not significant
*t-test significant (p-value <0.05); **One way AVOVA; OP, osteoporosis
* t-test significant (p-value <0.05); OP-osteoporosis