Story of a Giant Endometrial Polyp in Asymptomatic Postmenopausal Female
Jahnavi Meena1, Rahul Manchanda2, Sudhir Kulkarni3, Nirmal Bhargava4, Priyanka Mahawar5
1 Fellow, Department of Gynae Endoscopy, Manchanda’s Endoscopic Centre, Pushawati Singhania Research Institute, Delhi, India.
2 Head, Department of Gynae Endoscopy, Manchanda’s Endoscopic Centre, Pushawati Singhania Research Institute, Delhi, India.
3 Head, Department of Pathology, Pushawati Singhania Research Institute, Delhi, India.
4 Fellow, Department of Gynae Endoscopy, Manchanda’s Endoscopic Centre, Pushawati Singhania Research Institute, Delhi, India.
5 Fellow, Department of Gynae Endoscopy, Manchanda’s Endoscopic Centre, Pushawati Singhania Research Institute, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jahnavi Meena, H-25 C, DDA Flats, Dilshad Garden, Delhi-110095, India.
E-mail: docjahnavi@gmail.com
Endometrial polyps are localized overgrowth of endometrial glands and stoma through the uterine cavity. They are associated with postmenopausal bleeding, infertility and menorrhagia and are affected by unbalanced oestrogen therapy or increased frequency of tamoxifen exposure. We report a case of giant endometrial polyp in postmenopausal female without vaginal bleeding and hormone or drug use. A 65-year-old, postmenopausal female P3L2 with hypertension and Diabetes Mellitus (DM) came for routine health check-up. Her physical examination was normal. Pelvic examination uterus was multiparous sized, mid positioned and bilateral fornices were free. Patient was planned for hysteroscopic guided biopsy as her Ultrasonography (USG) showed endometrial thickness to be 12.3 mm. On hysteroscopy, there was hyperplastic endometrium with large endometrial polyp of size 8.5 cm. Polypectomy was done and the same was sent for histopathological evaluation. Report showed cystic hyperplasia without atypia.
To summarize, postmenopausal female will not always present with symptoms and USG can also quite frequently miss the diagnosis, so proper evaluation is needed using hysteroscopy which is gold standard for diagnosis and treatment of endometrial polyp.
Endometrial overgrowth, Hysteroscopic polyp excision, Uterine polyp
Case Report
A 65-year-old, postmenopausal female P3L2 with hypertension and DM came for routine health check up. There was no history of any drug use, especially hormone derivatives. Her physical and per abdominal examination was normal. On pelvic examination uterus was multiparous sized, mid positioned and bilateral fornices were free. On USG her endometrial thickness showed up as 12.3 mm. Patient was planned for hysteroscopic guided biopsy.
Hysteroscopy was performed with 2.9 mm office hysteroscope. The uterine cavity was distended with normal saline with a pressure of 80 mmHg. On hysteroscopy, in cervical canal dense adhesions were present; adhesiolysis was done for the same [Table/Fig-1]. In the uterine cavity, there was hyperplastic endometrium with large polyp of size 8.5 cm arising from the junction of left lateral and posterior wall of uterus [Table/Fig-2]. Polypectomy was done with the help of scissors and forceps and obtained tissue was sent for histopathological evaluation. After removal of the polyp, the uterine cavity was normal. The patient was discharged after 6 hours of surgery. The postoperative interval was unremarkable and the patient did not have any complaints on follow up.
Hysteroscopic finding showing dense adhesions being cut at cervical canal with help of scissors.
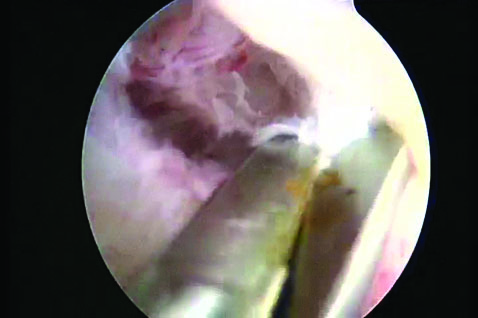
Giant polyp protruding from cervical canal.

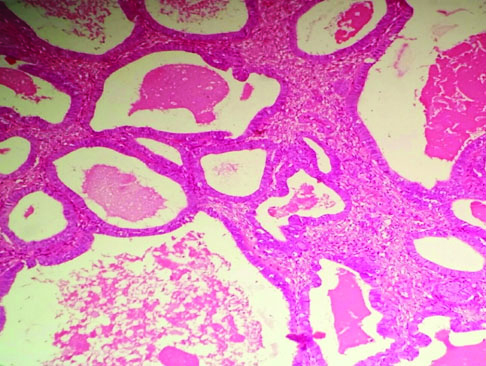
The pathological diagnosis confirmed it to be a giant endometrial polyp with a size of 8.5x1.5 cm [Table/Fig-3]. Microscopic, report showed cystic changes without atypia [Table/Fig-4]. It was composed of multiple endometrial glands embedded in the stroma. No nuclear or cytological atypia were noted. No sign of dysplasia or neoplasia was observed in the glandular or metaplastic epithelium. However, keeping her age, presence of hypertension, DM, obesity & histopathological finding in mind she was advised for total laparoscopic hysterectomy with bilateral salpingo-oophorectomy, though it was not performed as the patient did not consent.
Giant smooth walled polyp 8.5*1.5 cm.

Microscopically, glands of various sizes and irregular shapes are seen with cystic dilatation & epithelium is similar to proliferative type. (Images left to right)
Discussion
Endometrial polyps are localized overgrowths of endometrial tissue composed of variable amount of glands, stroma and blood vessels covered by epithelium. The stroma of the polyp is composed of fibroblast like spindle cells and large blood vessels with thick walls. The polyp epithelium may be active, pseudostratified and after menopause it can be inactive and flat. Depending on response to ovarian hormones, endometrial polyps are divided into three groups viz., mature functioning polyps, immature non functioning polyps and non functioning adenomyomatous polyps [1].
The development of endometrial polyps has been explained by number of molecular mechanisms such as monoclonal endometrial hyperplasia, over-expression of endometrial aromatase and gene mutations. Polyps have characteristic cytogenetic rearrangements similar to uterine leiomyoma. Rearrangements in the High-Mobility Group (HMG) family of transcription factors seem to play a role in pathogenesis [2]. Indraccolo U et al., studied the pathogenesis of endometrial polyps and they demonstrated a causative link: ageing, bcl-2 expression, obesity, tamoxifen regardless of timing and unbalanced oestrogen therapy [3].
Endometrial polyps are most frequently seen in multiparous women in the fifth decade. They are common cause of vaginal bleeding in pre and postmenopausal women, affecting 25% of them [4,5]. They are also associated with infertility. Some may be asymptomatic. In postmenopausal women, polyps usually present with bleeding or discharge accounting for 24.3%.
The most common size of polyp is less than 2 cm, and those greater than 4 cm are called giant polyps. Giant endometrial polyps occur with increased frequency secondary to unbalanced oestrogen levels or tamoxifen exposure after breast cancer [1].
The prevalence of malignancy with endometrial polyps is 1–3% [6]. The risk factors of malignancy within polyps are ageing, obesity, arterial hypertension, postmenopausal period, and tamoxifen.
Hormonal factors may be involved as indicated by endometrial abnormalities in patients treated with tamoxifen. Despite being an oestrogen antagonist, tamoxifen has oestrogen agonistic effects on the endometrium. The partial agonistic activity of tamoxifen in postmenopausal women may produce a hormonal environment of low levels of unopposed oestrogen similar to that in perimenopausal woman. In our patient, the polyp was asymptomatic and developed spontaneously as the patient was not on tamoxifen or other drugs including hormone replacement treatment.
Non-invasive techniques such as transvaginal USD, with or without the use of 3D USD and contrast techniques, remains first line for diagnosis. Transvaginal ultrasonography is a routine, non invasive component of investigation. On the sonographic examination, 12.3 mm thick endometrium was seen in our case which was suspicious and needed evaluation, especially in an asymptomatic postmenopausal female.
Histopathological examination must be performed on all resected polyps to rule out endometrial polyps (0.5%–3%) with malignant foci [1]. Lasmar BP et al., reported that endometrial polyps larger than 15 mm are associated with hyperplasia [5] and Wang J et al., identified that polyps measuring more than 10 mm are associated with malignancy [7]. For the treatment and histologic diagnosis of endometrial polyps, hysteroscopic resection is the most effective method, while blind biopsy and curettage have low diagnostic accuracy and should not be performed. [Table/Fig-5] shows various giant polyps reported in literature [8–14].
Table showing various giant polyps [8–14].
| Author | Size (cm) | Origin | Tamoxifen treatment | Cervical protrusion |
|---|
| Nomikos et al., [8]. | 8 | Uterus | + | - |
| Moon et al., [9] | 7 | Uterus | + | - |
| Cil et al., [10] | 8 | Uterus | - | + |
| Unal et al., [11] | 10 | Uterus | - | + |
| Arıdogan et al., [12] | 14 | Cervix | - | + |
| Branger et al., [13] | 15 | Cervix | - | + |
| Amesse et al., [14] | 5 | Cervix | - | + |
| Present case | 8.5 | Uterus | - | - |
Conclusion
In summary, the origin and pathogenesis of endometrial polyps have not been fully evaluated and understood. Giant endometrial polyps are rare entities and they are associated with tamoxifen and unbalanced oestrogen levels. For diagnostic and therapeutic management, hysteroscopy is the gold standard whereas blind dilation and curettage is not preferred. Removal for histologic assessment is appropriate in postmenopausal women.
[1]. Peterson WF, Novak ER, Endometrial polypsObstet Gynecol 1956 8(1):40-49. [Google Scholar]
[2]. Dal Cin P, Timmerman D, Van den Berghe I, Wanschura S, Kazmierczak B, Vergote I, Genomic changes in endometrial polyps associated with tamoxifen show no evidence for its action as an external carcinogenCancer Res 1998 58:2278 [Google Scholar]
[3]. Indraccolo U, Iorio R, Matteo M, Corona G, Greco P, Indraccolo SR, The pathogenesis of endometrial polyps: A systematic semi-quantitative reviewEur J Gynaecol Oncol 2013 34(1):5-22. [Google Scholar]
[4]. Jutras ML, Cowan BD, Abnormal bleeding in the climactericObstet Gynecol Clin North Am 1990 17(2):409-25. [Google Scholar]
[5]. Lasmar BP, Lasmar RB, Endometrial polyp size and polyp hyperplasiaInt J Gynaecol Obstet 2013 123(3):236-39. [Google Scholar]
[6]. Lieng M, Istre O, Sandvik L, Qvigstad E, Prevalence, 1-year regression rate, and clinical significance of asymptomatic endometrial polyps: cross-sectional studyJ Minim Invasive Gynecol 2009 16(4):465-61. [Google Scholar]
[7]. Wang J, Zhao J, Lin J, Opportunities and risk factors for premalignant and malignant transformation of endometrial polyps: Management strategiesJ Minim Invasive Gynecol 2010 17(1):53-58. [Google Scholar]
[8]. Nomikos IN, Elemenoglou J, Papatheophanis J, Tamoxifen-induced endometrial polyp. A case report and review of the literatureEur J Gynaecol Oncol 1998 19(5):476-78. [Google Scholar]
[9]. Moon SH, Lee SE, Jung IK, Jeong JE, Park WY, Yi WH, A gıant endometrıal polyp wıth tamoxıfen therapy ın postmenopausal womanKorean J Obstet Gynecol 2011 54(12):836-40. [Google Scholar]
[10]. Çil AS, Bozkurt M, Kara D, Guler B, Giant endometrial polyp protruding from the external cervical os in a postmenopausal woman: Magnetic resonance imaging and hysteroscopic findings proceedings in obstetrics and gynecology 2013 3(3):2 [Google Scholar]
[11]. Ünal B, Doğan S, Karaveli FS, Şimşek T, Erdoğan G, Candaner I, Giant endometrial polyp in a postmenopausal woman without hormone/drug use and vaginal bleedingCase Reports in Obstetrics and Gynaecology 2014 2014:5183984pages [Google Scholar]
[12]. Aridogan N, Cetin MT, Kadayifci O, Atay Y, Bisak U, Giant cervical polyp due to a foreign body in a ‘virgin’Aust N Z J Obstet Gynaecol 1988 28(2):146-47. [Google Scholar]
[13]. Branger C, Dreher E, Burkhardt A, Schmuckle U, Giant polyp of the cervixGeburtshilfe Frauenheilkd 1991 51(2):148-49. [Google Scholar]
[14]. Amesse LS, Taneja A, Broxson E, Pfaff-Amesse T, Protruding giant cervical polyp in a young adolescent with a previous rhabdomyosarcomaJ Pediatr Adolesc Gynecol 2002 15(5):271-77. [Google Scholar]