The term metabolic syndrome (syndrome X, insulin resistance syndrome) emerged from observations that there is gathering of cardiovascular risk factors in obese persons. Since the original definition by the World Health Organization in 1998, the criteria for the MS have evolved, reflecting growing clinical evidence. The major components of the metabolic syndrome include central obesity, hypertriglyceridemia, low HDL cholesterol, hyperglycaemia and hypertension. Insulin resistance is a central pathophysiological process associated with MS [1].
As defined by the World Health Organization (WHO) the prevalence of obesity is relatively low in Asia compared to Western countries [2]. Despite this, incidence of MS is rising in Asia and is growing into a significant public health problem. Previous studies indicate that metabolic responses to central obesity may be greater in South and East Asians than their Western counterparts at given Body Mass Indexes (BMIs) [3].
Materials and Methods
We included 100 consecutive patients with STEMI admitted to Government Medical College Thrissur, Kerala, India, a tertiary care hospital, in this prospective observational study. The study was carried out from April 2009 to February 2010. Persons with age below 25 years and above 70 years, abdominal distension due to pathological causes, pregnancy and those who didn’t give consent were excluded from the study.
Subjects fulfilling the inclusion criteria (patients admitted with STEMI) were enrolled in the study. Informed consent was obtained from the subjects. Demographic data (age and gender), and previous known risk factors were obtained. Height and weight were measured with the participant wearing light clothing and no shoes; body mass index was calculated as weight (kg)/height (m2). Subjects were assessed for the five-component conditions of the MS. Smoking habits and a physician diagnosis of high blood pressure were queried. Blood pressure was measured by using a standard mercury sphygmomanometer in the right upper limb in the supine position. The mean value of two measurements taken at least one minute apart was used in the analysis. Fifth-phase Korotkoff sound was used for diastolic blood pressure.
Fasting blood samples were drawn for glucose and lipid profile in first 24 hours after acute coronary insult. Fasting plasma glucose was measured with glucose oxidase method. In patients who have had an acute MI, lipoprotein levels measured within the first 24 hours provide an approximation of their usual levels, otherwise, levels may not be stable for up to six weeks. Total cholesterol and triglycerides were measured by enzymatic methods (EM 360 autoanalyser). The HDL cholesterol was measured by precipitation with Magnesium (Mg) and phosphotungstic acid. LDL cholesterol was calculated from the Friedewald equation (provided the triglycerides were <400 mg/dL) [11].
Waist circumference was measured using non stretchable flexible tape in horizontal position just above the iliac crest at the end of normal respiration, in the fasting state with the subject standing erect and looking straight forward and observer sitting in front of the subject.
Though the primary aim of this study was to describe the prevalence of MS among patients who presented with STEMI, secondary analyses were also performed for other parameters such as age, sex, BMI and the findings were compared between patients with and without MS.
There is a paucity of data regarding the applicability of NCEP-ATP 3 and International Diabetes Federation (IDF) definitions of the MS and its relationship with cardiovascular disease in Asians. The originally accepted criteria for the metabolic syndrome were based on risk prediction in the non-Asian Indian populations. However, the recent data from Asian Indians indicate that these definitions may not be satisfactory for risk prediction in Asians.
In this study MS was identified using criteria based on a “Consensus statement for diagnosis of metabolic syndrome for Asian Indians” [12]. This includes components of ATP 3 criteria with a modification for waist circumference [6]. Presence of three or more of the following suggest metabolic syndrome.
Waist circumference >90 cm in men and 80 cm in women.
Blood pressure >130/85 mmHg or on treatment for hypertension.
Fasting plasma glucose >100 mg% or on treatment for diabetes.
Serum triglycerides > 150 mg/dl, 5 HDL <40 mg/dl in male and <50 mg/dl in female.
ST Elevation Myocardial Infarction (STEMI): Typical rise and fall of biochemical markers of myocardial necrosis with at least one of the following: (a) ischemic symptoms; (b) development of pathologic Q waves on the ECG; (c) ECG changes indicative of ischemia- ST segment elevation at the J point in two or more contiguous leads with the cut off points 0.2 mV in leads V1, V2, or V3 and 0.1 mV in other leads [13].
Ethical Clearance of the Institute was obtained before conducting the study. There was no major ethical issues regarding the study and no invasive procedures were involved in the study.
Statistical Analysis
Data was analyzed using Epi Info software version 7.0. For descriptive statistics results of categorical variables expressed as frequency and percentages. Continuous variables expressed as means along with standard deviation. To test significance of association between different factors and MS Chi - square test was used. A p-value of less than 0.05 was considered statistically significant.
Results
The baseline characteristics of the study group are listed in [Table/Fig-1]. There were 100 patients (males 80, females 20) with a mean age of 58±9.8.
Baseline characteristics of patients.
| Baseline Characteristics | |
|---|
| Number of patients N (%) | 100(100) |
| Age (years) (mean±SD) | 58±9.8 |
| Males | 80 |
| Hypertension | 47(47) |
| Diabetes mellitus | 34(34) |
| Smoking | 76(76) |
| Coronary artery disease | 35(35) |
| BMI, kg/m2 (mean±SD) | 20.8±3.2 |
| Patients according to BMI | |
| Normal (<25 kg/m2) | 60(60) |
| Overweight (25-30 kg/m2) | 28(28) |
| Obese | 12(12) |
| Blood pressure (mm Hg) | |
| Systolic (mean±SD) | 136±22.5 |
| Diastolic (mean±SD) | 84±10.3 |
| Waist circumference cm (mean±SD) | |
| Male | 84±9.7 |
| Female | 85.3±8.7 |
| Lipid profile | |
| Total cholesterol(mean±SD) | 187±49 |
| High density lipoprotein (HDL) (mean±SD) | 56.1±15.4 |
| Low density lipoprotein(mean±SD) | 105.7±53.7 |
| Triglycerides(mean±SD) | 102.1±55.5 |
| Fasting blood sugar (mean±SD) | 129.3±48.8 |
| Metabolic syndrome components | |
| Elevated waist circumference | 45(45) |
| Elevated triglycerides | 16(16) |
| Reduced HDL cholesterol | 25(25) |
| Elevated blood pressure | 36(36) |
| Elevated fasting plasma glucose | 73(73) |
Data are presented as mean±SD or n (%); BMI: body mass index.
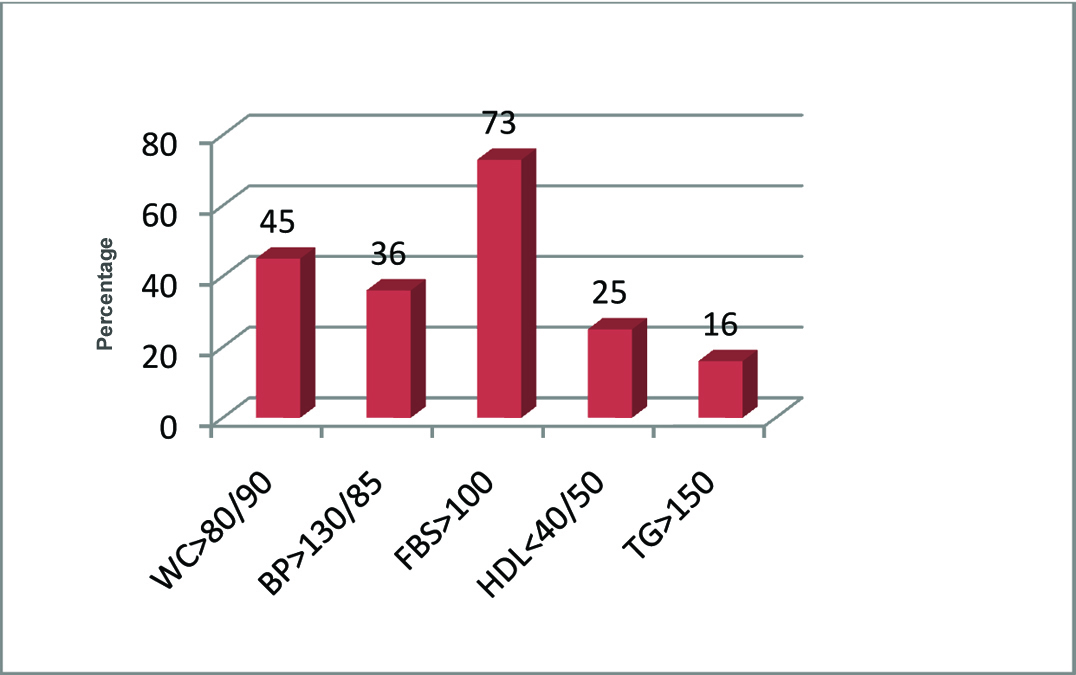
[Table/Fig-2] shows prevalence of individual components of MS in the study group. Waist circumference >80/90 was seen in 45 (45%), BP >130/85 was present in 36(36%), Fasting Blood Sugar (FBS) >100 was present in 73(73%), HDL <40(male) /50(female) was 25(25%), Triglycerides >150 was 16(16%). Elevated FPG and increased waist circumference were the most common metabolic components observed.
Frequency of components of MS.
WC = waist circumfernce, BP= Blood pressure, FPS= Fasting blood sugar, HDL= High density lipoprotein, TG= Tryglycerides
Overall frequency of MS in patients admitted with STEMI was found to be 40 (40%). A total of 29 (36%) of total males and 11 (55%) of total females were deemed to have MS [Table/Fig-3]. Frequency of pre-existing diabetes was 34%, pre-existing hypertension was 47%, pre-existing ischemic heart disease was 35%.
Among the 100 patients with STEMI, 49(49%) were diagnosed with anterior wall MI and 37 (37%) were diagnosed with inferior wall MI. Mean BMI was 20 (kg/m2). Nineteen (24%) males and 9 (45%) females were overweight, together contributing 28% of total patients. Almost 12% were obese {5 (6.3%) males and 7(35%) females}. Prevalence of overweight was higher in patients with MS as compared to the group without MS 40% vs 28% (p<0.05). Similar observation was found for obesity 18% vs 12% (p<0.05). Total 77% of patients in MS group (p<0.001) and 70% of females (p-0.0117) were having increased waist circumference i.e., central obesity.
Mean systolic BP was 136±22.5 and diastolic BP was 84±10.3. Mean waist circumferences was 85.3±8.7 in females and 84±9.7 in males. Mean total cholesterol was 187±49 (males 188, females 183). Mean LDL was 105.7±53.7 and HDL was 56.1±15.4. Mean triglycerides was 102.1±55.5.
On univariate analysis with patients divided into those with MS and without MS, significant differences were noted between the MS and non-MS groups in the prevalence of components of MS. Frequency of individual components in MS group vs no MS group is shown in [Table/Fig-3].
Frequency of individual components in MS vs No MS group.
| Variable | MS | MS% | No MS | No MS% | Total | p-value |
|---|
| Male | 29 | 36% | 51 | 63% | 80% | 0.1283 |
| Female | 11 | 55% | 9 | 45% | 20% | 0.1283 |
| BMI>22.9 | 16 | 40 | 12 | 20 | 28% | 0.0292 |
| BMI>24.9 | 7 | 18 | 5 | 8 | 12% | 0.0259 |
| WC>80/90 | 31 | 77 | 14 | 23 | 45% | <0.001 |
| BP>130/85 | 23 | 58 | 13 | 22 | 36% | 0.0002 |
| FPG>100 | 37 | 93 | 36 | 60 | 73% | 0.0002 |
| HDL<40/50 | 18 | 45 | 7 | 12 | 25% | 0.0001 |
| TG>150 | 15 | 37.5 | 1 | 1.7 | 16% | 0.0000 |
| DM | 16 | 40% | 18 | 30% | 34% | 0.3059 |
BMI :body mass index WC :waist circumference BP: blood pressure FPG: fasting plasma glucose HDL: high density lipoproteins TG : Triglycerides DM: Diabetes Mellitus
Data analyzed with chi-square test.
Discussion
Study was conducted on 100 consecutive patients with ST elevation myocardial infarction. Out of these 40 (40%) patients were found to have MS on applying the criteria. Among these 29 patients were males and 11 were females accounting for 36% of the males and 55% of the females respectively.
The prevalence of MS in patients with Acute Coronary Syndrome (ACS) spans around 29 and 62% in various studies as there is diversity in the definition of MS criteria [14]. The prevalence of MS in patients with ACS has not been well documented especially in South east Asian population even though there is large evidence regarding the adverse impact of MS. MS is commonly associated with CAD according to Western studies [15]. Zeller M et al., in their study of 633 STEMI patients found that 46% fulfilled criteria for MS [15]. Al-Aqeedi RF et al., reported a prevalence of 63% [14] and Pandey S et al., reported 26.1 % of MS in ACS [16].
Present study reveals high prevalence of MS in STEMI patients, particularly in female gender. Out of the total number of females 55% satisfied the criteria for MS.
Turhan H et al., in a study reported higher prevalence of MS in women with CAD than men (73% versus 31%). In addition women had a significantly higher mean number of components of MS compared to men [17]. Pandey S et al., also reported higher prevalence of metabolic syndrome in females [16].
The mean BMI in the study was 20. Twenty eight (28%) of the total patients were overweight and 12 (12%) of the total were having obesity. Mean BMI in Yasmin S et al., study was 25 in males and 32 in females [18]. In the study by Prasad SP mean BMI was 29.7 [19]. Kumar N et al., in their study found a prevalence of 16.7% for obesity [20]. The mean BMI and obesity in our study was low compared to these studies, may be because most of the patients were from a lower socio economic class. Obesity and being overweight were significantly more prevalent in the MS patients. In the MS group 40% were overweight and 18 were obese compared to 20% and 8% in non MS group.
On analyzing the individual components of MS elevated FPG (73%) was the most common component followed by waist circumference 45%. FPG was more than 100 in 73% of the total patients. Yasmin S et al., found that 56% patients had high FPG value, but here the cut off for FPG was 110 instead of 100 in our study [19]. Chung EH et al., found a high FPG of 75% [21] and Al-Aqeedi RF et al., reported FPG OF 76% in their study [14]. This high prevalence of elevated FBS may be part of stress hyperglycaemia due to the STEMI.
Out of the 100 patients 45 had WC >80/90. Central obesity was significantly high in MS group. In patients with MS, 31(77.5%) patients were having a big waist compared to 14 (23%) in non MS group. Yasmin S et al., noted a high prevalence of increased waist circumference in 45% of patients in their study [19]. Gupta R et al., in their study reported 54% [22] and Al-Aqeedi RF et al., reported 65% of patients with truncal obesity [14].
Despite the markedly high prevalence of MS in this high risk population, there is a low rate of clinical detection and management of metabolic syndrome. This supports the potential for preventive efforts in the form of lifestyle modifications including a balanced diet and exercise.
Limitation
There were some limitations in the present study. It was a prospective single center study. The frequency of metabolic syndrome may have been underestimated as the sample size was relatively small.
Conclusion
The present study concluded that there is a remarkably high occurrence of MS and central obesity in patients with ST elevation MI in our local population, especially in females, despite low mean BMI and low rates of general obesity. Given the high prevalence of central obesity and MS in this population, the role of specific and targeted interventions for clinical detection and management of MS needs to be addressed.
Author Contribution
Both Dr Uppalakkal Bijilesh and Dr Lekshmi Sankar K were involved in the concept, study design, data collection and analysis of the study. Dr Lekshmi Sankar was working in Government Medical College, Thrissur, Kerala, India at the time of the study, where the study was conducted. She then got shifted to Government Medical College, Manjeri, Kerala, India which is in the nearby district.
Data are presented as mean±SD or n (%); BMI: body mass index.
BMI :body mass index WC :waist circumference BP: blood pressure FPG: fasting plasma glucose HDL: high density lipoproteins TG : Triglycerides DM: Diabetes Mellitus
Data analyzed with chi-square test.