Invasive Mucormycosis in a Case of Aluminium Phosphide Poisoning
Nitin Gupta1, Gagandeep Singh2, Karan Aggarwal3, Alok Thakar4, Immaculata Xess5
1 Senior Resident, Department of Medicine and Microbiology, Infectious Disease Division, All India Institute of Medical Sciences, Delhi, India.
2 Assistant Professor, Department of Microbiology, All India Institute of Medical Sciences, Delhi, India.
3 Junior Resident, Department of Otorhinolaryngology, All India Institute of Medical Sciences, Delhi, India.
4 Professor, Department of Otorhinolaryngology, All India Institute of Medical Sciences, Delhi, India.
5 Professor, Department of Microbiology, All India Institute of Medical Sciences, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Immaculata Xess, Professor, Department of Microbiology, All India Institute of Medical Sciences, Delhi-110029, India.
E-mail: immaxess@gmail.com
Mucormycosis is a rapidly progressive disease with high mortality reported mostly in immunocompromised individuals. We report a case of Rhino-orbital mucormycosis (Lichtheimia corymbifera) in an immunocompetent individual with history of consumption of Aluminium Phosphide (ALP) tablets. We postulated the following effects of ALP poisoning that would have increased the chances of mucormycosis in this patient: 1) Metabolic acidosis; 2) Acute Kidney Injury (AKI); and 3) Liberation of free oxygen radicals.
Invasive fungal infections, Lichtheimia corymbifera, Pesticide poisoning
Case Report
A 20-year-old female patient with no prior co-morbidities developed acute onset of vomiting, loose stools and pain abdomen within an hour of ingestion of two tablets of ALP. She was admitted to a local hospital where it was noticed that she had decreased urine output along with raised urea (198.5 mg/dl) and creatinine (6.0 mg/dl) implying acute renal failure. Arterial Blood Gas (ABG) analysis revealed metabolic acidosis (pH-7.2, pCO2-13.7 mmHg, pO2-63 mmHg). She received five sessions of haemodialysis and was started on intravenous meropenem and vancomycin.
She was referred to our hospital after nine days of initial presentation. She was admitted with complaints of fever, decreased vision in both eyes, swelling of both eyelids and bleeding from nose since previous six days. There was no significant past history. Examination revealed bilateral periorbital oedema, proptosis along with bilateral necrotic areas in the nasal cavity. There was no perception of light in the right eye. In the left eye, perception of light was present but the patient was not able to detect hand movement with her left eye. There was complete loss of all the ocular movements. HIV, HBsAg and Anti HCV were negative. Her peripheral smear did not show any blast cells. Her blood sugar and HBA1C levels were within normal limits. Non-contrast computed tomography scan of the paranasal sinuses showed heterogeneous densities in bilateral maxillary, ethmoidal, frontal and sphenoidal sinuses with preseptal, zygomatic and premaxillary extension suggestive of fungal sinusitis. The Calcofluor white - KOH examination of the nasal crusts revealed broad aseptate hyphae branching at right angle [Table/Fig-1]. The patient was diagnosed as a case of rhino-orbital mucormycosis.
Calcofluor white KOH mount of nasal crust shows aseptate hyphae.

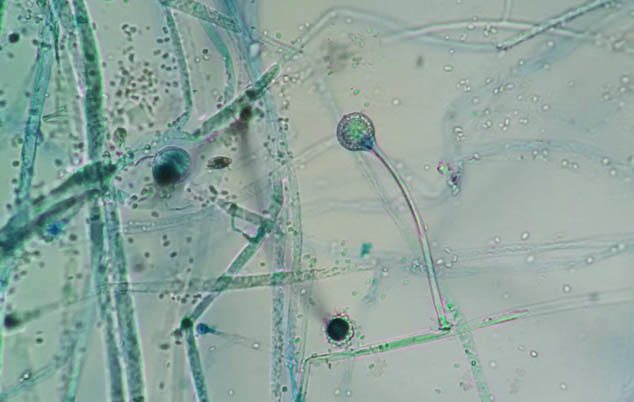
She was started on intravenous amphotericin B and bilateral nasal endoscopic debridement was done. The nasal crust sample was also cultured on sabouraud dextrose agar (Trios, Prague, Czech Republic). Rapidly growing colonies were observed after 48 hour which were identified as Lichtheimia corymbifera based on the micro-morphological features [Table/Fig-2]. The patient however succumbed to refractory shock.
Lactophenol Cotton blue mount shows Lichtheimia corymbifera.
Discussion
Mucormycosis is a rapidly progressive disease with very high mortality [1]. The alarming rise in the number of cases reported from developing countries including India is a cause of great concern. Rhino-Orbito-Cerebral (ROC) mucormycosis is the most common form in India [1]. The most common mucormycetes implicated in ROC are Rhizopus, Mucor and Lichtheimia spp. [1]. Although it is most commonly reported in settings of uncontrolled diabetes, prolonged steroid therapy and haematological malignancies, cases in immunocompetent individuals has been frequently reported [2,3]. We report a case of Rhino-orbital mucormycosis in an unusual backdrop of ALP poisoning. ALP is a commonly used pesticide in India and is amongst the commonest and deadliest suicidal poison [4]. It is freely available in the markets in 3 gm tablets. The fatal dose for ALP is (0.15-0.5) gm.
The occurrence of invasive mucormycosis in an otherwise immunocompetent individual suggests that the ALP poisoning had some role in increasing the odds. We postulate the following mechanisms that possibly led to increased susceptibility to infection with mucormycetes in this patient:
Metabolic acidosis as a result of ALP poisoning [5]: Acidosis increases the susceptibility to mucormycosis since the iron required for hyphal growth is released from transferrin as the blood pH drops [6]. Acidosis also renders the phagocytic cells dysfunctional. Both neutrophils and macrophages exhibit an impaired chemotaxis and defective killing by both oxidative and non-oxidative pathways under such conditions [7].
Acute kidney injury caused by ALP poisoning: AKI is a known effect of ALP poisoning. Systemic mucormycosis has been reported in both acute and chronic renal failure. Patients with chronic renal failure on maintenance haemodialysis have been reported to be more susceptible to mucormycosis. Decreased cell-mediated immunity and impaired functions of neutrophil might be responsible for the increased susceptibility in these cases [6].
Free Oxygen Radicals liberated due to ALP poisoning: ALP poisoning induces oxidative stress and causes increased release of free oxygen radicals. It also affects the cytochrome oxidase enzyme and glutathione, thereby interfering with the anti-oxidative mechanisms. This results in lipid peroxidation and protein denaturation of the cell membrane in various organs making them more susceptible [8].
Conclusion
We present this case to highlight the possibility of mucormycetes in unusual clinical settings. In a country like India, where aluminium phosphide poisoning and mucormycosis are both common and fatal, it needs to be ascertained that whether they have any causal association between them.
[1]. Chakrabarti A, Singh R, The emerging epidemiology of mould infections in developing countriesCurr Opin Infect Dis 2011 24(6):521-26. [Google Scholar]
[2]. Chakrabarti A, Chatterjee SS, Das A, Panda N, Shivaprakash MR, Kaur A, Invasive zygomycosis in India: Experience in a tertiary care hospitalPostgrad Med J 2009 85(1009):573-81. [Google Scholar]
[3]. Suresh S, Arumugam D, Zacharias G, Palaninathan S, Vishwanathan R, Venkatraman V, Prevalence and clinical profile of fungal rhinosinusitisAllergy & rhinology (Providence, RI) 2016 7(2):115-20. [Google Scholar]
[4]. Singh D, Dewan I, Pandey AN, Tyagi S, Spectrum of unnatural fatalities in the Chandigarh zone of north-west India-A 25 year autopsy study from a tertiary care hospitalJ Clin Forensic Med 2003 10(3):145-52. [Google Scholar]
[5]. Proudfoot AT, Aluminium and zinc phosphide poisoningClin Toxicol (Phila) 2009 47(2):89-100. [Google Scholar]
[6]. Binder U, Maurer E, Lass-Florl C, Mucormycosis from the pathogens to the diseaseClin Microbiol Infect 2014 20(Suppl 6):60-66. [Google Scholar]
[7]. Ibrahim AS, Spellberg B, Walsh TJ, Kontoyiannis DP, Pathogenesis of mucormycosisClin Infect Dis 2012 54(Suppl 1):S16-22. [Google Scholar]
[8]. Chugh SN, Arora V, Sharma A, Chugh K, Free radical scavengers and lipid peroxidation in acute aluminium phosphide poisoningIndian J Med Res 1996 104:190-93. [Google Scholar]