Magnetic Resonance Imaging in Mixed Mullerian Tumour: Report of Two Cases
Pratiksha Yadav1, Vidhi Bakshi2, Rajul Bhargava3
1 Associate Professor, Department of Radio Diagnosis, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pune, Maharashtra, India.
2 Chief Resident, Department of Radio Diagnosis, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pune, Maharashtra, India.
3 Chief Resident, Department of Radio Diagnosis, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratiksha Yadav, Associate Professor, Department of Radio Diagnosis, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Sant Tukaram Nagar, Pimpri, Pune-411018, Maharashtra, India.
E-mail: yadavpratiksha@hotmail.com
Malignant Mixed Mullerian Tumours (MMMTs) or carcinosarcomas of uterus are rare aggressive tumours of mesenchymal origin. It is associated with high incidence of lymphatic, pulmonary and peritoneal metastasis. We hereby present two cases of mixed mullerian tumour. Case-1 was a 60-year-old post menopausal woman who had come with complaint of metrorrhagia and a protruding mass in the vagina. Case-2 was of a 54-year-old post-menopausal woman who came with complaints of heavy vaginal bleeding, pelvic pain since two months. For the assessment of these tumours Magnetic Resonance Imaging (MRI) is preferred imaging modality due to excellent tissue contrast to detect the myometrial invasion, local extent and staging. Preoperative differentiation of mullerian tumour with endometrial carcinoma is important as both have different treatment.
Carcinosarcoma, Polypoidal mass, Uterine neoplasm
Case Report
We present two cases of mixed mullerian tumour.
Case-1
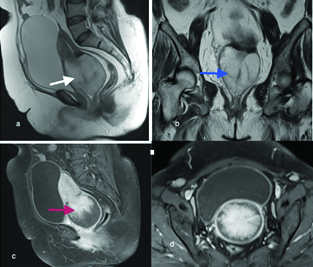
A 60-year-old woman reported with complaints of bleeding per vagina since three months and pelvic pain since four months. She was feeling a protruding mass in the cervix and vagina since two months. On examination, there was a fungating polypoidal mass in the cervical endometrium and superior part of vagina. Ultrasonography (USG) of pelvis was advised which showed a heterogenous, lobulated mass, involving the inferior aspect of uterus and cervix. The mass was protruding into the vagina. MRI was advised for further evaluation which showed a well defined large, lobulated mass occupying the cervix and inferior aspect of uterus with expansion of the cervical canal [Table/Fig-1a]. It measured 7.8 cm (craniocaudal) x 6.5 cm (transverse) 6.8 cm (anteroposterior). The mass was hyperintense on T2WI and STIR, hypointense on T1WI [Table/Fig-1a,b]. On post contrast MRI it showed heterogenous enhancement [Table/Fig-1c,d]. There were multiple septae seen in the mass. Fat plane was lost between the mass and the bladder [Table/Fig-1a], however fat plane between mass and the rectum was maintained. Multiple lymph nodes were seen in the bilateral internal iliac and bilateral inguinal region, largest at the left internal iliac measured 1.7 cm x 1.5 cm. Both ovaries were not visualized, probably atrophic. The patient was operated and a large fungating mass was removed. It revealed high grade sarcomatous and carcinomatous elements consistent with mixed mullerian tumour on histopathology [Table/Fig-2].
Sagittal T2WI showing; a) Large predominantly hyperintense mass seen involving the inferior aspect of uterus and cervix (white arrow). Fat plane between bladder and mass was lost; b) Coronal T2WI showing heterogenous mass with expansion of the cervical endometrium (blue arrow); c) Post gadolinium T1WI sagittal image and; d) Post gadolinium T1WI axial image showing heterogenous enhancement of the mass (red arrow).
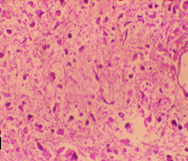
Histopathology of the mixed mullerian tumour. Haematoxylin and eosin stain (original magnification x400) showing high grade carcinomatous and sarcomatous components.
Case-2
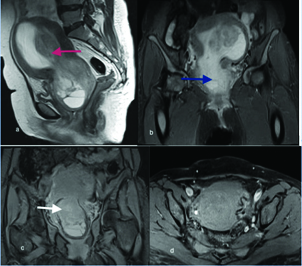
A 54-year-old post-menopausal woman reported with the complaint of vaginal bleeding, pelvic pain and frequent micturition since four months. Patient had no other past medical history. On clinical examination uterus was enlarged and a mass was felt in the cervix. USG pelvis was done which revealed enlarged uterus with a large heterogenous mass which involved posterior wall of the uterus and cervix. There was thickened endometrial cavity with fluid seen in the uterine and cervical endometrial cavity. On MRI, the uterus was enlarged with distorted normal shape and outline [Table/Fig-3a]. A heterogeneous mass seen involving the right posterolateral wall of the uterus and cervix [Table/Fig-3a]. This mass was protruding into the endocervical canal and causing expansion of the uterine and cervical endometrium [Table/Fig-3b]. The mass was effacing the posterior wall of the bladder and anterior wall of the rectum with loss of intervening fat plane. On post contrast MRI it showed heterogenous enhancement [Table/Fig-3c,d]. Hysteroscopic biopsy was done and carcinosarcoma was revealed on histopathology. Patient was operated and the large mixed mullerian tumour was detected on postoperative biopsy.
MRI showing: a) Sagittal T2WI showing a mixed signal intensity mass in the uterine cavity with expansion of the uterine and cervical endometrial cavity (red arrow); b) Coronal STIR image showing large heterogenous mass with herniation into the cervix (blue arrow); c, d) Post contrast coronal and axial T1WI showing heterogenous enhancement of mass (white arrow).
Discussion
Mixed mullerian tumours are very rare aggressive tumours with poor prognosis [1]. It usually arise in the uterine corpus however it can arise from cervix, ovaries and fallopian tubes [2]. Patients with MMMT’s have poor prognosis as compare to endometrial carcinoma. Preoperative differentiation of mullerian tumour with endometrial carcinoma is important as both have different treatment.
Uterine sarcomas have been divided into three types namely the endometrial stromal sarcomas, leiomyosarcomas, and MMMTs. MMMTs are metaplastic carcinomas which have both mesenchymal and epithelial components, hence they are said to be as an aggressive form of endometrial carcinoma. According to the The International Federation of Gynaecology and Obstetrics (FIGO) classification, MMMTs fall under the same staging system as endometrial carcinoma [3]. Incidence of MMMTs increases with age, more common in postmenopausal women. Some of the predisposing factors include excess oestrogen, obesity and nulliparity. In addition, recent studies have shown tamoxifen to be a risk factor in the development of both uterine MMMT and endometrial carcinoma [4]. Patient usually presents with pyometra, vaginal bleeding and abdominal pain. Elderly patients may present with a polypoid mass. [5]. At physical examination, 50%–95% of patients have bulky uterus with nearly half of them having protrusion of a polypoid lesion through the endocervical canal [6]. The triad of symptoms includes severe vaginal bleeding, pain and the passage of necrotic tissue per vaginum [7].
The work up of these patients includes routine blood investigations and chest X-rays, also pyelography, cystoscopy, proctoscopy, and bone scans if required [8]. Increased levels of serum CA-125 have been reported in some cases [9].
MRI is the choice of modality for the visualization and assessment of these tumours because of it’s improved ability to delineate extent and local spread of disease [10].
The MR signal-intensity characteristics of MMT cannot be differentiated from endometrial carcinomas. Usually the tumours are well defined although the tumour margins usually irregular. Bharwani N et al., retrospectively reviewed MRI examination of 51 histologically confirmed MMMT’s [11]. Epicenter of majority of these tumours was endometrium (88%) [11]. On T1WI majority of MMMT’s were isointense to myometrium and endometrium, on T2WI 92% of MMMT’s were hyperintense to myometrium and hypo or isointense to endometrium [11]. Post contrast MRI showed heterogeneous enhancement in 58% and homogeneous enhancement in 42% cases [11]. In this study 88% of MMMT’s were indistiguishable from endometrial adenocarcinoma [11]. Large exophytic MMMT’s not obliterating the normal uterine architexture though large endophytic growths invade the myometrium [12]. In both of our cases the tumour was large and heterogeneous with epicenter was at endometrium. In Case-1, it was protruding mass with expansion of the cervical endometrium and in Case-2 it showed expansion of the uterine as well as cervical endometrium.
MMMTs are frequently large in size and exhibit aggressive nature, by spreading extensively through the myometrium. In addition, the peritoneum will be involved in over half of the cases that extend beyond the uterus [13]. Worthington JL et al., described that the large masses had a heterogeneous T2-weighted signal intensity and mildly in homogeneous low T1- weighted signal intensity [14].
Recent studies using Diffusion Weighted MRI (DW-MRI) in characteristics of MMMTs and uterine sarcomas have suggested that DW-MRI may be a useful technique for differentiation of MMMTs with endometrial carcinoma [15]. Combined anatomic and functional imaging of endometrium which includes the use of routine T1-weighted and T2-weighted sequences together with DCE-MRI and DW-MRI may be useful to differentiate these two groups of endometrial pathologic abnormalities [11].
Conclusion
Uterine carcinosarcoma is a rare, aggressive, rapidly progressing neoplasm with a poor prognosis. The imaging findings of uterine MMMTs are not pathognomonic. However, the presence of enhancement equal to or more than that of the myometrium points towards the possibility of an MMMT. The presence of cervical stromal invasion and nodal enlargement at presentation is a common feature of MMMTs.
[1]. Kanthan R, Senger JL, Uterine carcinosarcomas (malignant mixed müllerian tumours): a review with special emphasis on the controversies in managementObstetrics and Gynecology International 2011 2011:470795 [Google Scholar]
[2]. Shim JJ, Shim JC, Lee HK, Lee KE, Lee GJ, Kim HK, Malignant mixed mullerian tumour arising from the uterine cervix: a case reportJ Korean Soc Radiol 2012 67(4):263-67. [Google Scholar]
[3]. Prat J, FIGO staging for uterine sarcomasInt J Gynaecol Obstet 2009 104(3):177-78. [Google Scholar]
[4]. Wickerham DL, Fisher B, Wolmark N, Bryant J, Costantino J, Bernstein L, Association of tamoxifen and uterine sarcomaJ Clin Oncol 2002 20:2758-60. [Google Scholar]
[5]. El-Nashar SA, Mariani A, Uterine carcinosarcomaClinical Obstetrics and Gynecology 2011 54(2):292-304. [Google Scholar]
[6]. Kuyumcuo lu U, Kale A, Homologous type of malignant mixed Mullerian tumour of the uterus presenting as a cervical massJournal of the Chinese Medical Association 2009 72(10):533-35. [Google Scholar]
[7]. Doss LL, Llorens AS, Henriquez EM, Carcinosarcoma of the uterus: a 40-year experience from the state of MissouriGynecologic Oncology 1984 18(1):43-53. [Google Scholar]
[8]. Ho KC, Lai CH, Wu TI, Ng KK, Yen TC, Lin G, 18 F-fluorodeoxyglucose positron emission tomography in uterine carcinosarcomaEuropean Journal of Nuclear Medicine and Molecular Imaging 2008 35(3):484-92. [Google Scholar]
[9]. Huang GS, Chiu LG, Gebb JS, Gunter MJ, Sukumvanich P, Goldberg GL, Serum CA125 predicts extrauterine disease and survival in uterine carcinosarcomaGynecologic Oncology 2007 107(3):513-17. [Google Scholar]
[10]. Tanaka YO, Tsunoda H, Minami R, Yoshikawa H, Minami M, Carcinosarcoma of the uterus: MR findingsJournal of Magnetic Resonance Imaging 2008 28(2):434-39. [Google Scholar]
[11]. Bharwani N, Newland A, Tunariu N, Babar S, Sahdev A, Rockall AG, MRI appearances of uterine malignant mixed müllerian tumoursAJR 2010 195:1268-75. [Google Scholar]
[12]. Sahdev A, Sohaib SA, Jacobs I, Shepherd JH, Oram DH, Reznek RH, MR imaging of uterine sarcomasAJR 2001 177:1307-11. [Google Scholar]
[13]. Rockall AG, Meroni R, Sohaib SA, Reynolds K, Alexander S, Shephard JH, Evaluation of endometrial carcinoma on magnetic resonance imagingInt J Gynecol Cancer 2007 17:188-96. [Google Scholar]
[14]. Worthington JL, Balfe DM, Lee JK, Gerjell DJ, Heiken JP, Ling D, Uterine neoplasms: MR imagingRadiology 1986 159:725-30. [Google Scholar]
[15]. Namimoto T, Yamashita Y, Awai K, Nakaura T, Yanaga Y, Hirai T, Combined use of T2-weighted and diffusion-weighted 3-T MR imaging for differentiating uterine sarcomas from benign leiomyomasEur Radiol 2009 19:2756-64. [Google Scholar]