Cervical pregnancy is a rare site of ectopic pregnancy compared to tubal. The trophoblast implant into the cervical tissue and become a potentially dangerous site of torrential haemorrhage. The widespread use of Ultrasonography (USG) has led to a dramatic increase in the detection rates of extra uterine pregnancy. We hereby report an interesting case of extra uterine pregnancy with a unique situation where only a high index of suspicion prevented an iatrogenic mishap. The patient was referred as a case of incomplete abortion with a documented report of minimal retained products. Because of a high index of suspicion a serum beta Human chorionic gonadotropin (hCG) was sent prior to deciding for discharge. This indeed turned as a major change in the diagnosis of the case as the serum beta hCG was elevated. On re-evaluation, we diagnosed it as a case of cervical pregnancy which was successfully managed medically.
Ectopic, Foley, Methotrexate, Tamponade
Case Report
A 30-year-old primigravida, normotensive was referred to the Department of Obstetrics and Gynaecology as a case of complete abortion. The chief complaint was spotting and pain lower abdomen following overdue menses for 16 days. This was a spontaneously conceived pregnancy with previous regular cycle. There was no significant past medical and family history. Also there was no history of any prior surgery, vaginal procedure, any genital infections or any contraceptive use prior to conception.
She was not taking any other medication except folic acid 5 mg once daily which was started by her treating doctor once she was overdue by a week. She was non-smoker and her period of gestation on admission was five weeks six days. Urine pregnancy test done at that time showed weak positivity. There was no distinct history of passage of clots or fleshy mass. There was no history of fainting attack, dizziness or syncope. Her transvaginal sonography done at some external centre showed a normal size uterus with a suspicion of incomplete abortion. She was planned for a dilatation and curettage there but because of her constant discomfort she visited us.
On examination in our department, her vitals were stable except tachycardia with a pulse rate of 120 per minute. She was afebrile. Her abdomen was soft and there was no guarding, rigidity, tenderness or organomegaly.
Vaginal speculum examination showed a normal appearing cervix, with minimal bleeding. Vaginal examination revealed a slightly bulky anteverted soft uterus with bilateral normal adenexa without any mass and tenderness. There was neither any appreciable cervical tenderness nor ballooning.
Routine investigations revealed normal complete blood counts, A+ blood group, and negative viral markers. Transvaginal USG of pelvis done at external centre when the patient was 15 days overdue was reported as small amount of retained products with volume 9.8 ml with bilateral normal adenexa and no free fluid.
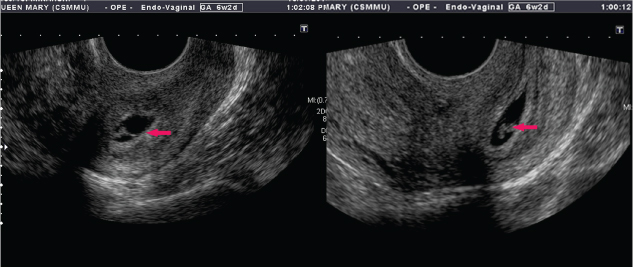
Serum beta hCG sent on admission came as 9946 μIU/ml. Repeat USG done at our centre showed an empty uterine cavity with presence of a gestational sac below the level of the internal os in the cervical canal with a negative sliding organ sign [Table/Fig-1]. A foetal node with a cardiac activity and a sustained peritrophoblastic circulation was seen on colour Doppler examination with high blood flow velocity and low impedence.
USG showing cervix with closed internal os and a gestational sac with good decidual reaction shown by left sided red arrow. Right sided arrow shows foetal node in the gestational sac.
The decision of medical management of cervical ectopic was taken essentially considering the nulli parous status of the patient. After ensuring the normal blood counts, renal and liver function test, multidose methotrexate was started in the dose of 1 mg/kg alternating it with folinic acid 0.1 mg/kg. After 48 hours (day 3) of first dose of methotrexate, the serum beta hCG increased from 9946 to 11,317 μIU/ml. Patient started to have a significant bleeding per vaginum without any cramping pain. Decision of intarcervical foley tamponade was taken as an emergency management option. An endocervical foley tamponade was done with 20 ml saline and the catheter was left in situ for 24 hours following which the active bleeding stopped. The patient’s vitals remain stable throughout. After second dose serum beta hCG declined to 614 μIU/ml (day 5). USG after seven days showed no evidence of gestational sac and a compressed echogenic thickening in cervix possibly the absorbing compressed trophoblast. There was no pelvic collection and the patient was discharged in stable condition. On follow up, patient was absolutely fine with a beta hCG of 18 μIU/ml on day 15 and 6 μIU/ml after four weeks post chemotherapy. Products of conception were sent for histopathology which showed degenerated and viable chorionic villi with decidualized tissue in endocervical tissue.
Discussion
Cervix is an extremely rare site of ectopic pregnancy accounting for less than 1% of all pregnancies [1]. The trophoblast implant into the cervical tissue and become a potentially dangerous site of torrential haemorrhage. The widespread use of USG has led to a dramatic increase in the detection rates of extrauterine pregnancy.
Differentials for cervical pregnancy include a cervical phase of uterine abortion where the placenta lies within the expanded cervix with dilated external and internal os, and a cervical abortion where the entire sac comes in the cervical canal and the external os is closed and stenosed. A ragged and friable cervix in few cases of cervical pregnancy can also mimic a carcinoma cervix [2].
The patient was referred to us as a case of incomplete abortion with a documented USG report of minimal retained products. As such repeating beta hCG in all patients prior to suction is not a routine practice in our center but since the patient was neither giving any history of instrumentation nor was having any significant clinical bleeding and cervical os was closed, a high index of suspicion was raised and serum beta hCG was sent prior to deciding for discharge. This indeed turned as a major change in the diagnosis of the case as the serum beta hCG was elevated. On re-evaluation, we diagnosed a cervical pregnancy which was managed medically successfully.
Long back in 1911, Rubin IC reported criteria to diagnose a cervical pregnancy which involves histopathology [3], however later Paalman R and McElin T have given five clinical criteria to diagnose cervical pregnancy which includes uterine bleeding without cramping pain, an enlarged cervix giving an hourglass uterus, products of conception confined within endocervix, closed internal cervical os and a partially opened external cervical os [4]. Various factors that lead to a higher risk of cervical ectopic include previous uterine curettage, anatomic anomalies (myomas, synechiae), Intrauterine Device (IUD) use, assisted reproduction, diethylstilbestrol exposure and previous caesarean section [5].
A high index of suspicion is indeed required to diagnose cervical ectopic pregnancy in patients without any high risk factors as seen in our case since the patient was a nullipara without any history of uterine instrumentation or any other risk factor.
The treatment for cervical pregnancy has traditionally been surgical which includes an abdominal hysterectomy other interventions in selected patients include a skilful dilatation and curettage which carries a very high chance of profuse haemorrhage, transvaginal ligation of cervical branches of uterine arteries, a shirodkar type cerclage, angiographic uterine artery embolization and intracervical vasopressin injection [5].
Mohebbi MR et al., reported a case of abnormal implantation below prior section scar in a fifth gravida with prior two caesarean sections [6]. USG showed a thickened enlarged cervix with gestational sac of six weeks with cardiac activity. Serum beta hCG was 15,437 mIU/ml. Patient started to have heavy bleeding per vaginum and suction curettage of gestational sac was performed. Among various methods available, the authors did not consider antimetabolite medications such as methotrexate since previous data had shown unsatisfactory results if serum beta hCG is more than 10000 IU/L [7]. However, in recent report by Samal S et al., a cervical pregnancy showing a live foetus of seven weeks four days with beta hCG of 1,03,113 mIU/ml was successfully managed by multidose methotrexate and intraamniotic KCI followed by suction curettage of cervical canal [8].
Although in this case the bleeding was taken care of by suction curettage, there have been case reported by Gupta V et al., in a patient who was referred to them as a case of two months pregnancy with history of attempted dilatation and evacuation followed by profuse bleeding per vaginum which finally required an abdominal hysterectomy [9]. The histopatholgy of cervix showed a chorionic villi and decidual implantation while endometrium showed a hypersecretory change with partial decidualization of stroma. Another patient mentioned in their report was also referred as missed abortion. The patient had amenorrhoea of 15 weeks with spontaneous bleeding. The scan showed an ill-defined gestational sac in endometrial cavity which was diagnosed as blighted ovum and cervix was not commented upon. As soon as dilator was introduced in cervix, patient started bleeding profusely and went into haemorrhagic shock. All resuscitative efforts were taken and intracervical foley tamponade was done with 30 ml saline and patient could be saved.
The available literature does show reports when cervical pregnancy was diagnosed when bleeding occurred while intending to treat a intrauterine pregnancy [10,11].
Profuse bleeding per vaginum and hysterectomy can be avoided by keeping a high index of suspicion for possibility of a primary cervical pregnancy.
Systemic chemotherapy followed by manual vacuum evacuation and foley tamponade in a viable nine weeks cervical pregnancy has been previously reported [12]. The clinching point for easy diagnosis in their case was a ballooned out cervix which was absent in our case and we indeed encountered a relatively less distended cervix on examination as well as on USG but with a viable foetal node and closed internal os and this is not reported till yet.
As our patient was a nullipara, we went ahead for medical management even with a viable foetus. We found that even after start of methotrexate, patient can have bleeding and intracervical foley is a brilliant way to have tamponade and gradually the trophoblast are spontaneously resorbed without any surgical interference.
Conclusion
We hereby report a rare site of extra uterine pregnancy with a unique situation where only a high index of suspicion prevented an iatrogenic mishap. Examination of cervical canal and its collection is a must in imaging for any pregnancy of unknown origin. Raised serum beta hCG along with non-visualization of gestational sac in uterine cavity should be an alarm for pregnancy of unknown origin and cervical site should always be kept in mind. Before embarking on invasive procedure like dilatation and curettage or hysterectomy; consideration can be given to medical management with multidose methotrexate if patient is haemodynamically stable. Tamponade by intracervical foley is an extremely useful method to control start of bleeding in cervical pregnancy along with ongoing medical management.
[1]. Leeman LM, Wendland CL, Cervical ectopic pregnancy. Diagnosis with endovaginal ultrasound examinationand successful treatment with methotrexateArch Fam Med 2000 9:72-77. [Google Scholar]
[2]. Gun M, Mavrogiorgis M, Cervical ectopic pregnancy: a case report and literature reviewUltrasound Obstet Gynecol 2002 19:297-301. [Google Scholar]
[3]. Rubin IC, Cervical pregnancySurg Gynecol Obstet 1911 13:625 [Google Scholar]
[4]. Paalman R, McElin T, Cervical pregnancyAm J Obstet Gynecol 1959 77:1261 [Google Scholar]
[5]. Ushakov FB, Elchalal U, Aceman PJ, Schenker JG, Cervical pregnancy: past and futureObstet Gynecol Surv 1996 52:45 [Google Scholar]
[6]. Mohebbi MR, Rosenkrans KA, Luebbert EE, Hunt TT, Jung MJ, Ectopic pregnancy in cervix: A case reportCase Rep Med 2011 2011:858241 [Google Scholar]
[7]. Hung TH, Shau WY, Hsieh TT, Hsu JJ, Soong YK, Jeng CJ, Prognostic factors for an unsatisfactory primary methotrexate treatment of cervical pregnancy: a quantitative ReviewHuman Reproduction 1998 13(9):2636-42. [Google Scholar]
[8]. Samal S, Ghose S, Pallavee P, Porkkodi P, Successful management of live cervical ectopic pregnancy: a case reportJ Clin Diagn Res 2015 9(12):03-04. [Google Scholar]
[9]. Gupta V, Acharya R, Bansal N, Nanda A, Tandon A, Rani A, Cervical ectopic pregnancy: case report and management modalitiesJournal of South Asian Federation of Obstetrics and Gynecology 2010 2(1):77-79. [Google Scholar]
[10]. Saha E, Paul AK, Cervical ectopic pregnancy mimicking missed abortionBang Med J 2011 44:28-30. [Google Scholar]
[11]. Khatib Y, Khashikar A, Wani R, Patel RD, Cervical ectopic pregnancy: A case report of missed diagnosisMed J DY Patil Univ 2016 9:741-43. [Google Scholar]
[12]. Singh S, Diagnosis and management of cervical ectopic pregnancyJ Hum Reprod Sci 2013 6(4):273-76. [Google Scholar]