The two most common dental diseases viz., dental caries and periodontal diseases are caused by dental plaque which is a complex microbial community [1]. Thus, plaque control should be an indispensable part of the daily chores of every individual as the onset of dental diseases can be primarily prevented by regular and meticulous plaque removal. Tooth-brushing, when accomplished properly, results in effective plaque control. However, mechanical plaque control methods have certain inherent limitations [2]. Therefore, adjunctive chemical plaque control methods such as use of mouthwash have been suggested as additional therapeutic strategy to augment but definitely not to replace mechanical plaque control [3]. Mouthwash supplements routine mechanical oral hygiene procedures in controlling supragingival plaque formation.
Due to availability of a variety of mouthwashes with different active ingredients, there is always a dilemma among patients and practitioners regarding its choice. CHX, till date, is considered to be the most effective anti-plaque agent, but with certain limitations [4–6]. Hence, search for an effective and safe alternative to CHX mouthwash has led to introduction of various herbal products in dentistry which are without any major side effects, besides being cheap and locally available [6]. Natural herbs when used in mouthwashes, have shown significant advantages over the chemical ones [7,8].
Probiotics, another potential tool of anti-plaque activity, have been reported to have beneficial effects on oral health [9]. Still, probiotics are not widely used in clinical dental practice due to lack of awareness about probiotics. This calls for actions to be taken in this direction because once the probiotics set a foothold in dentistry, they can be concomitantly beneficial for oral as well as systemic health of the human body and can apparently prove to be a panacea of health promotion. Hence, the present study was designed with an aim to compare the effectiveness of herbal and probiotic mouthwashes with that of CHX on plaque accumulation, gingival health and oral hygiene status.
Materials and Methods
The present study was randomized controlled trial with three parallel groups. Ethical clearance for the present study was obtained from Institutional Ethical Committee of ACPM Dental College and Hospital, Dhule, Maharashtra, India, and permission to conduct study was obtained from the principal of the same institute. The study was conducted at Department of Public Health Dentistry, ACPM Dental College and Hospital, Dhule, Maharashtra for one month. Three different mouthwashes used were Hexidine mouthwash containing 0.2% chlorehexidine gluconate (ICPA Health Products Ltd.), HiOra regular mouthwash (The Himalaya Drug Company) and Darolac sachets (Aristo Pharmaceuticals Pvt. Ltd.). A total of 45 healthy subjects were recruited for the study. Sample size of 45 was calculated using Software G Power (Version 3.1.9.2, 2014) considering effect size f=0.51, α=0.05 and 80% power of the study [10].
Inclusion criteria: Systemically healthy subjects in the age group of 18-21 years, residing in hostel of dental college and who agreed to comply with the study visits were included.
Exclusion criteria: Subjects with malaligned teeth, wearing orthodontic appliances and removable partial dentures; subjects with chronic or aggressive periodontitis; subjects with history of oral prophylaxis within past six months; tobacco consumers and smokers, subjects on any antibiotic therapy in past three months and subjects with medical or pharmacological history that could compromise the conduct of the study were excluded.
A total of 45 subjects were divided into three groups of 15 each (Groups A, B and C) employing simple random sampling by random number table method and each group was randomly assigned one mouthwash by lottery method. The random allocation sequence was generated by one of the authors employing random number table method. The random allocation sequence was concealed from the main investigator until mouthwashes were assigned to the participants. The main investigator enrolled the study subjects and assessed the study variables.
Group allocation: Group A rinsed with 15 ml of HiOra (herbal) mouthwash for 60 seconds twice daily 30 minutes after toothbrushing for 14 days and then spit it; Group B rinsed with 10 ml of hexidine mouthwash for 60 seconds twice daily 30 min after toothbrushing for 14 days and then spit it; Group C rinsed with Darolac (probiotic) sachets dissolved in 20 ml of water for 60 seconds twice daily 30 minutes after toothbrushing for 14 days and then swallowed it. The subjects were asked not to eat or drink anything for next half an hour to achieve the effect of the mouthwash.
Blinding: The blinding and concealment were controlled by a third person (pharmacist of dental college) who distributed mouthwashes in plain plastic bottles of same size identified as Group A and Group B. The content of the Darolac sachets was transferred into small zip lock plastic pouches of similar size so as to maintain uniformity. All the study subjects were unaware of the contents of the bottles and pouches; however blinding of the investigators regarding probiotic mouthwash could not be achieved since it was in powder form. Pharmacist revealed the contents only after completion of the study. The statistician was also blinded with respect to the allotment of intervention in the three groups. Thus, this was a triple-blind study.
All the subjects received complete supragingival scaling to remove all plaque, stains and calculus at baseline. All the study subjects received the toothbrushes and toothpastes of same made to overcome the confounding bias. The cups of herbal and CHX mouthwashes had markings for measurement, while probiotic group subjects were provided daily with freshly prepared 15 ml of mouthwash. The subjects were instructed to withdraw the use of mouthwashes and report immediately if they experienced any side effects due to the use of mouthwashes. Subjects were instructed to brush twice daily with the given toothbrush and toothpaste. The use of mouthwash by female study subjects was monitored by the principal investigator herself in the girls’ hostel of dental college; whereas, the use of mouthwash by male study subjects was monitored by a male assistant investigator at the boys’ hostel of dental college. All the subjects were asked to report to the Department of Public Health Dentistry on the seventh day and 14th day for the recording of the variables i.e., OHI-S [11] to assess oral hygiene status, Plaque Index (PI) described by Silness and Loe in 1964 [12] to measure plaque and Gingival Index (GI) described by Loe and Silness in 1963 to assess gingival status [12].
The clinical examination (type III) of every patient was carried out by principle investigator herself who was calibrated. The calibration was done on a group of 10 subjects, who possessed collectively the full range of conditions expected to be assessed in the study. Oral examination of 10 randomly selected subjects was repeated on different dates. The results so obtained were subjected to κ statistics. The kappa coefficient value for intra-examiner reliability was 0.86 for OHI-S, 0.78 for PI and 0.84 for GI. This value reflected almost perfect agreement in observations [13]. All the three variables i.e., OHI-S, PI and GI were recorded at baseline, on the seventh day and on the 14th day following the use of allocated mouthwashes.
Statistical Anaylsis
The data obtained was subjected to statistical analysis using SPSS 17.0. Depending upon the nature of data, chi square test was applied for categorical data and ANOVA was applied to test continuous data. Significance was assessed at 5% level of significance (p<0.05).
Results
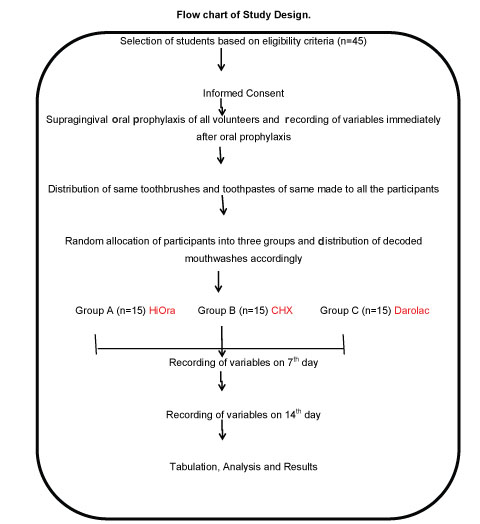
The flowchart of study design is shown in [Table/Fig-1]. [Table/Fig-2] shows gender wise distribution of study subjects in three groups, seven males (46.7%) and eight females (53.3%) in each. [Table/Fig-3] shows comparison of mean values of variables at day 0 (baseline), seven and 14. ANOVA test showed significant difference in the mean values of OHI-S, PI and GI between day 0, day 7 and day 14 in the three groups (p<0.001).
Flowchart depicting study design.
Gender wise distribution of study subjects in three groups.
| Groups | Male | Female | Total |
|---|
| HiOra (Herbal) | 7 (46.7%) | 8 (53.3%) | 15 (100%) |
| CHX | 7 (46.7%) | 8 (53.3%) | 15 (100%) |
| Probiotic | 7 (46.7%) | 8 (53.3%) | 15 (100%) |
| Total | 21 (46.7%) | 24 (53.3%) | 45 (100%) |
Intragroup comparison of mean values of variables at baseline, day 7 and day 14.
| Variable | Mean Value | p-value |
|---|
| Day 0 | Day 7 | Day 14 | |
| HiOra (Herbal) |
| OHI-S | 0 | 0.31±0.21 | 0.17±0.12 | 0.001* |
| PI | 0 | 0.05±0.02 | 0.04±0.01 | 0.001* |
| GI | 0.15±0.05 | 0.05±0.02 | 0.03±0.01 | 0.001* |
| Chlorhexidine |
| OHI-S | 0 | 0.33±0.21 | 0.19±0.09 | 0.001* |
| PI | 0 | 0.06±0.03 | 0.04±0.07 | 0.001* |
| GI | 0.19±0.09 | 0.06±0.03 | 0.04±0.02 | 0.001* |
| Probiotic |
| OHI-S | 0 | 0.30±0.13 | 0.20±0.12 | 0.001* |
| PI | 0 | 0.07±0.02 | 0.04±0.06 | 0.001* |
| GI | 0.18±0.11 | 0.07±0.02 | 0.04±0.09 | 0.001* |
Repeated measure ANOVA; * Significance at p<0.05
[Table/Fig-4] shows comparison of mean values of variables between three groups. ANOVA test showed that there was no significant difference in the effect of the three mouthwashes on plaque accumulation, gingival health and oral hygiene status except in the mean values of GI between groups A, B and C at day seven (p<0.05).
Intergroup comparison of mean values of variables between three groups.
| Variables | Interval | Mean score | p-value |
|---|
| HiOra | CHX | Probiotic | |
|---|
| OHI-S | Baseline | 0 | 0 | 0 | - |
| Day 7 | 0.31±0.17 | 0.33±0.21 | 0.30±0.13 | 0.795 (NS) |
| Day 14 | 0.17±0.12 | 0.19±0.09 | 0.20±0.12 | 0.694 (NS) |
| PI | Baseline | 0 | 0 | 0 | - |
| Day 7 | 0.05±0.02 | 0.06±0.03 | 0.07±0.02 | 1.277 (NS) |
| Day 14 | 0.04±0.01 | 0.04±0.07 | 0.04±0.06 | 0.177 (NS) |
| GI | Baseline | 0.15±0.05 | 0.19±0.09 | 0.18±0.11 | 0.404 (NS) |
| Day 7 | 0.05±0.02 | 0.06±0.03 | 0.07±0.02 | 0.270 (NS) |
| Day 14 | 0.03±0.01 | 0.04±0.02 | 0.04±0.09 | 0.092 (NS) |
ANOVA test; NS – Not significant; * significance at p<0.05
Discussion
The present study compared the efficacy of probiotic, herbal and CHX mouthwashes on oral health using three variables, viz. OHI-S, PI and GI. The results obtained showed that there was a significant improvement in gingival bleeding, plaque accumulation and oral hygiene after 14 days in all the three groups [Table/Fig-2]. Also, it was seen that except for GI on day 7, there was no significant difference in the effectiveness of the three mouthwashes. At day 7, HiOra regular mouthwash was more effective than probiotic mouthwash whereas, there was no significant difference between HiOra regular and probiotic mouthwashes as well as probiotic and CHX mouthwashes [Table/Fig-3].
Oral prophylaxis was carried out for all the study subjects to maintain homogeneity in baseline data between the three groups [14]. Subjects were instructed to rinse with the specified amount of each mouthwash for 60 seconds twice daily i.e., 10 ml and 15 ml of CHX and HiOra regular mouthwashes respectively as per manufacturers’ instructions. The use of each Darolac sachet dissolved in 20 ml of water was in accordance of a study conducted by Jindal G et al., [15]. The subjects of the three groups were instructed to use the mouthwash 30 minutes after toothbrushing as per previous literature [16,17].
All the three mouthwashes showed improvement in the mean scores of OHI-S, PI and GI after 14 days of use. This can be attributed to anti-bacterial property of CHX. CHX attacks the bacterial cell membrane, causing leakage and/or precipitation of the cellular contents. Specifically, it binds to salivary mucins, which reduces pellicle formation and inhibits plaque colonization. It also binds to bacteria and hinders their adsorption onto the teeth [18]. In case of HiOra mouthwash, contents of the mouthwash such as pilu, bibhitaka, nagavalli, gandhapurataila, ela, peppermint satva, Yavanisatva helped in improving oral health. Bibhitaka and nagavalli have been documented to reduce significantly the cell-surface hydrophobicity of three early plaque settlers and inhibits adherence of bacteria to the host tissues [19,20]. Pilu, locally called miswak, is a well-known anti-plaque and anti-microbial agent due to presence of an alkaloid, salavdorin [19,21]. Ela is an effective gargle in bad odour of the oral cavity and dental ailments. E. cardamomum has been reported to significantly inhibit the growth of oral microflora [19].
The present study employed Darolac sachets dissolved in water. Each 1 gm sachet of Darolac contains probiotics not less than 1.25 billion cells of L. acidophilus, L. rhamnosus, B. longum and S. boulardii. Lactobacilli produce low molecular weight bacteriocins with an inhibitory effect against a wide range of bacterial species related to oral diseases [22]. L. rhamnosus demonstrates both high antimicrobial activity and high tolerance of environmental stress [23]. Assistance of Bifidobacterium species includes metabolism of lactose, generation of lactic ions from lactic acid and vitamin synthesis. They also produce beneficial short-chain fatty acids [24]. Saccharomyces boulardii has anti-microbial action [25]. It is probably the synthesis of compounds like bacteriocin or biosurfactant and inhibition of cell association, colonization and invasion by pathogenic bacteria that are responsible for the anti-plaque action of probiotics like Darolac [26]. Hence, in the present study, Darolac improved gingival health due to above mentioned facts. Darolac sachets dissolved in water were used as mouthwashes by “Swish and Swallow” technique in accordance with study conducted by Jindal G et al., [15]. The ‘swishing’ part ensured oral benefits and ‘swallowing’ is supposed to provide systemic benefits.
Following is a summary of the available literature regarding chlorhexidine, herbal and probiotic studies, highlighting studies which have obtained results similar to the present study and those that have obtained contradictory results [Table/Fig-5] [19,26–34]:
Few related studies at a glance.
| Sr no | Similar Studies | Contradictory Studies |
|---|
| 1 | Parwani SR et al., who showed no significant difference of post-rinsing PI scores between CHX and herbal mouthwash groups [27]. | Singh A et al., where statistically significant difference in plaque parameters was observed with CHX compared to HiOra Regular Mouthwash [19]. |
| 2 | Narayan A and Mendon C where HiOra and CHX mouthwashes were shown to have equal anti-plaque efficacy [28]. | Harini PM and Anegundi RT where there was no significant difference in the mean plaque scores of probiotic and CHX groups but probiotic group proved to be statistically better than CHX when GI was considered [32]. |
| 3 | Shetty S et al., where there were no statistically significant differences between CHX and HiOra groups with regards to OHI, PI and GI [29]. | Biswas G et al., where improvement in plaque and gingival index scores were better in CHX group than herbal mouthwash [33]. |
| 4 | Shah RK, who demonstrated no significant difference in the gingival inflammation between probiotic and CHX mouthrinses at the end of study duration [30]. | Purunaik S et al., which showed that probiotic mouthrinse was significantly more effective than chlorhexidine at the end of 14th day [26]. |
| 5 | Nadkerny PV et al., who showed equal efficacy of probiotic and chlorhexidine mouthwashes in reduction of OHI-S, PI and GI at the end of 28th day [31]. | Mishra R et al., where maximum reduction in PI was seen with chlorhexidine rinse, followed by herbal mouthwash and minimum in probiotic mouthwash at the end of one week [34]. |
Clinical Implications and Future Prospects
It is perhaps surprising that chemical anti-plaque agents of superior or atleast equivalent efficacy, as an alternative to CHX, to overcome its undesirable side effects, safety and better acceptability have largely not been found and CHX remains the so-called gold standard of plaque control agents. With the public being increasingly cautious about the use of synthetic drugs owing to their adverse effects, “run of the masses” towards natural remedies is on an uptrend and oral health is no exception to this. Hence, oral hygiene products of herbal origin such as herbal mouthwashes need to be studied for their efficacy. Probiotics are proved to have dual health benefits, both locally on oral health as well as systemically on general health. Thus, both herbal and probiotic mouthwashes can be advocated as suitable alternatives to CHX if their use and prescription is supported by strong scientific evidence.
Limitation
A cross-over design with wash-out period could have been a more valid study design as it eliminates the bias of variable host response.
Conclusion
It can be concluded that the three mouthwashes i.e., CHX, herbal and probiotic were equally effective in improving oral health. The authors suggest the promotion of herbal as well as probiotic mouthwash after conducting clinical trials on a larger scale, so that risk of adverse effects is reduced and general health is promoted along with oral health.
Repeated measure ANOVA; * Significance at p<0.05
ANOVA test; NS – Not significant; * significance at p<0.05