Anaesthetic Management in Brugada Syndrome - A Case Report
Sulochana Dash1, Shanmugam Pragathee2
1 Associate Professor, Department of Anaesthesiology, Saveetha Medical College, Chennai, India.
2 Post graduate, Department of Anaesthesiology, Saveetha Medical College, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sulochana Dash, Vijay Shanti Infinite, Tower – 1, 6A, Chettipedu, Thandallam-602105, Tamilnadu, India.
E-mail: dr.silu76@gmail.com
Brugada Syndrome (BS) is a rare congenital cardiac disorder involving cardiac sodium channels, sometimes presenting with ventricular arrhythmia and sudden cardiac death. Here, we are reporting a case of BS who presented for laparotomy due to obstructed inguinal hernia which was managed satisfactorily with combined epidural and general anaesthesia without any complications.
Epidural anaesthesia, Laparotomy, Ventricular arrhythmia
Case Report
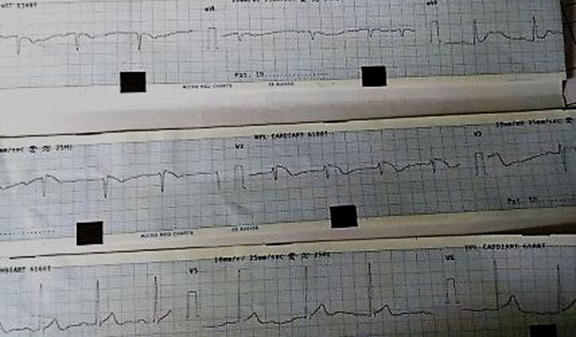
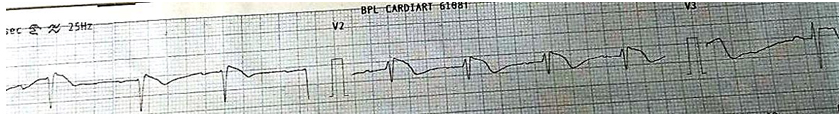
A 72-year-old male patient was incidentally diagnosed as a case of BS on routine preoperative investigation. He was posted for emergency laparotomy for obstructed inguinal hernia. There was no history of angina, syncope and the effort tolerance was about four Metabolic Equivalents (METS). Family history was negative for BS. On examination: weight-60 kg, heart rate-85/min, BP-130/80 mmHg and airway examination was normal. His investigations were within normal limit except Echocardiogram (ECG) which showed Right Bundle Branch Block (RBB) pattern with coved ST segment in V1 to V3 as per the [Table/Fig-1,2] below. His echocardiography was normal with ejection fraction of (EF) – 60%.
Showing 12 lead ECG of the patient showing RBB pattern with ST elevations in right precordial leads.
Showing ECG pattern in V1, V2 and V3 (coved ST segment elevation).
After explaining the procedure, the risk involved with the procedure, a written informed consent was obtained from the patient and he was then shifted to Operating Room (OR). Combined epidural and General Anaesthesia (GA) was planned. Monitors (ECG, NIBP, SpO2, EtCO2) were connected. Defibrillator was kept ready in OR and pads were connected to patient. Two wide bore IV cannulae were started. Right radial artery was cannulated for invasive BP monitoring. Patient was premedicated with Inj. midazolam 1 mg, Inj. glycopyrrolate 0.2 mg and Inj. fentanyl 40 μg IV. Epidural catheter was placed at the T12-L1 level and 5 cm of catheter length was kept in the space. Patient was preloaded with 500 ml of Ringer’s Lactate (RL). GA was induced with Inj. fentanyl 80 μg, inj. propofol 80 mg and inj. vecuronium 6 mg IV was used for intubation. We did not follow Rapid Sequence Intubation (RSI) as the patient presented with irreducible inguinal hernia which was going towards obstruction and features of obstruction were not significant. So we avoided succinyl choline for intubation. Anaesthesia was maintained with oxygen and nitrous oxide at a flow rate of 500 ml/min each and isoflurane 1% with intermittent top up doses of vecuronium. Epidural anaesthesia was activated with 0.125% bupivacaine 10 ml slowly over a period of 20 minutes. The procedure lasted for one hour. At the end of surgery inj. ondansetron 4 mg was administered IV for PONV prophylaxis. Inj. glycopyrrolate 0.5 mg was administered IV followed by Inj. neostigmine 2.5 mg. Patient was extubated at OR and shifted to High Dependency Unit (HDU) for 48 hours of observation. Postoperative analgesia was maintained with epidural top up of 0.125% bupivacaine with tramadol 50 mg SOS. Patient was haemodynamically stable throughout intra and postoperative period and the procedure was uneventful. On third postoperative day he was shifted to ward.
Discussion
BS is rare autosomal dominant congenital cardiac disorders resulting from mutation in SCN5A gene which encodes for tetrodotoxin insensitive human cardiac voltage gated sodium channels (hH1) [1]. This loss of function mutation reduce sodium current available during phase 0 (upstroke) and 1(early repolarisation) of cardiac action potential which leads to voltage gradient during repolarisation and characteristic ST changes in ECG (coved- shaped ST elevation in right precordial leads). Mutations in genes coding for alpha1 and beta 2 subunits of L type calcium channels (CACNA1C and CACNB2) is also thought to cause a variant of BS which causes precordial ST elevation, sudden death and short QT interval [2]. It was first described in 1992 by Brugada and Brugada. The clinical presentation of BS varies from being asymptomatic to having syncope, seizures, palpitation and even sudden death [3]. Prevalence of BS is 1 in 2000 [4–6]. It is more common in men than women and is responsible for 4% of all sudden deaths and 20% of sudden deaths in patients without any structural heart disease [7]. BS is diagnosed by the characteristic ST segment changes as per the 2013 consensus guideline [8]. It is of three types: Type 1- coved type ST elevation ≥ 2 mm with T inversion. Type 2- ST elevation of < 2 mm with either positive of biphasic T wave (Saddle back configuration). Type 3- ST elevation of < 1 mm, saddle back type. BS is diagnosed by typical BS pattern ECG in at least two right precordial leads (V1–V3) and any of the followings: Ventricular Fibrillation (VF), polymorphic ventricular tachycardia, inducible ventricular tachycardia during Electrophysiology (EP) study and unexplained syncope suggesting tachyarrhythmia, nocturnal agonal respiration, family history of SCD and BS pattern ECG. Patients with BS are at risk of ventricular fibrillation and sudden cardiac death during perioperative period due to triggers like medications, surgery, fever, electrolyte disturbances and changes in autonomic nervous system tone. Such patients might present for surgery without any warnings symptoms as in our case. So to avoid perioperative arrhythmias and SCD it is mandatory to optimise of dyselectrolytemia, maintain adequate depth of anaesthesia and normothermia [9,10]. Invasive arterial line should be cannulated for monitoring BP and central venous cannulation should be done for major cases associated with significant fluid shift [9–11]. As we did not anticipate more fluid shift, so central venous cannulation was not done and the case was managed with two peripheral 18 G IV cannulae. External defibrillator pads should be attached to all patients routinely as we did. Patient on Implantable Cardioverter Defibrillator (ICD) should be turned off preoperatively and turn on postoperatively [9,10,12]. Continuous Propofol infusion should be avoided. Epidural blockade with bupivacaine has been safely used in many cases, but dose should be less. We used diluted conc. of local anaesthetic (0.125% Bupivacaine) to reduce the dose. Neostigmine has been used for reversal without any complications when it is combined with Glycopyrrolate. Patient has to be monitored in HDU for 48 hours. A case was reported in 2002 in Oxford Radcliffe Hospitals Trust, Oxford, UK where patient was managed satisfactorily with GA and epidural anaesthesia as in our case who was posted for emergency laparotomy [13]. Similarly, a case of emergency appendicectomy has been managed satisfactorily under GA in Hamad Medical Corporation, Doha, Qatar using propofol, fentanyl, atracurium and isoflurane [14]. A case of facial artery and b/l Maxillary artery embolization for epistaxis was managed under GA in University of Maryland School of Medicine, Baltimore, USA in 2013 without complication [15].
Conclusion
Anaethesiologist should be familiar with BS to manage it during perioperative period satisfactorily. So thorough pre-anaesthetic evaluation and meticulous perioperative management with timely diagnosis and treatment of arrhythmias can decrease the mortality and morbidity and gives better outcome as in our case.
[1]. Rook MB, Bezzina Alshinawi C, Groenewegen WA, Human SCN5A gene mutations alter cardiac sodium channel kinetics and are associated with the Brugada syndromeCardiovasc Res 1999 44:507-17. [Google Scholar]
[2]. Antzelevitch C, Cordeire JM, Casio O, Sanguinettti MC, Aizaw Y, Loss of function mutations in cardiac calcium channel underlie a new clinical entity characterised by ST segment elevation, short QT intervals, and sudden cardiac deathCirculation 2007 115(4):442-49. [Google Scholar]
[3]. Brugada P, Brugada J, Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter reportJournal of the American College of Cardiology 1992 20(6):1391-96. [Google Scholar]
[4]. Antzelevitch C, Brugada syndromePacing Clin Electrophysiol 2006 29(10):1130-59. [Google Scholar]
[5]. Brugada R, Campuzano O, Sarquella-Brugada G, Brugada J, Brugada P, Brugada syndromeMethodist Debakey Cardiovasc J 2014 10(1):25-28. [Google Scholar]
[6]. Shimizu W, The Brugada sundrome—an updateIntern Med 2005 44(12):1224-31. [Google Scholar]
[7]. Berne P, Brugada J, Brugada syndrome 2012Circ J 2012 76:1563-71. [Google Scholar]
[8]. Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, HRS/EHRA/APHRS Expert consensus Statement on the Diagnosis and management of patients with Primary Arrythmia syndromeHeart rhythm 2013 10:1932-63. [Google Scholar]
[9]. Carey SM, Hocking G, Brugada syndrome—a review of the implications for the anaesthetistAnaesth Intensive Care 2011 39:571-77. [Google Scholar]
[10]. Kim JS, Park SY, Min SK, Kim JH, Lee SY, Moon BK, Anaesthesia in patients with Brugada syndromeActa Anaesthesiol Scand 2004 48:1058-61. [Google Scholar]
[11]. Santambrogio LG, Mencherini S, Fuardo M, Caramella F, Braschi A, The surgical patient with Brugada syndrome: a four-case clinical experienceAnesth Analg 2005 100:1263-66. [Google Scholar]
[12]. Inamura M, Okamoto H, Kuroiwa M, Hoka S, General anesthesia for patients with Brugada syndrome. A report of six casesCan J Anaesth 2005 52:409-12. [Google Scholar]
[13]. Edge J, Blackman DJ, Gupta K, Sainsbury M, General anaesthesia in a patient with Brugada syndromeBritish Journal of Anaesthesia 2002 89(5):788-91. [Google Scholar]
[14]. Raval C, Saeed K, Anaesthetic management of a patient of Brugada syndrome for an emergency appendicectomyAnesthesia: Essays and Researches 2012 6(1):101-04. [Google Scholar]
[15]. Smith D, Martz DG, Brugada Syndrome: A Review of Peri-operative Management for the AnesthesiologistInt J Clin Anesthesiol 2014 2(1):1019-21. [Google Scholar]