Primary Tuberculosis of Nose Causing Bilateral Nasal Obstruction and Halitosis in a 25-Year-Old Woman
Leena Rajam1, M Hari Kumar2, Sabitha Hari Kumar3
1 Assistant Professor, Department of ENT, Institute of Social Obstetrics and Kasturba Gandhi Hospital for Women and Children, Chennai, India.
2 Senior Lecturer, Department of Oral Medicine and Radiology, Saveetha Dental College and Hospital, Chennai, India.
3 Consultant Dental Surgeon, Dr. Hari’s Dental and ORO Care, Nagercoil, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. M Hari Kumar, Dr. Hari’s Dental and ORO Care, No. 711B; Opposite to Vadasery Mosque, TVM Road, Nagercoil-629001, Tamil Nadu, India.
E-mail: drhari.omrd@gmail.com
Primary or secondary nasal tuberculosis is rare and usually, it is considered as an extra pulmonary form of tuberculosis. Nasal tuberculosis infection may spread to maxillary palatal region by contagious or haematogenous route causing palatal perforation. In some instance, it may cause septal perforation with nasal obstruction which may give rise to halitosis. We report a case where, there was bilateral nasal mucosal involvement leading to severe nasal obstruction. This rare manifestation should be considered in areas where the disease is prevalent as delay in diagnosis and treatment could lead to serious and life threatening complications due to local spread from the nose to the para nasal sinuses and brain.
Biopsy, Caseating granuloma, Culture, Diagnostic nasal endoscope
Case Report
A 25-year-old woman presented to dental clinic with history of bilateral nasal obstruction and halitosis, along with nasal mucoid discharge for one year. There was neither history of headache, dyspnoea, haemoptysis, ear discharge or throat complaints, nor history of loss of appetite or loss of weight. She had received several courses of different antibiotics with no response for the presenting complaint, before she presented to our clinic. Details about the antibiotics were not available. The patient had received Bacille Calmette Guerin (BCG) vaccination in her childhood.
Vital signs remained within normal limits with pulse of 80 bpm and respiratory rate was 20/minute. The blood pressure was 124/80 mmHg. Her investigation revealed haemoglobin 9.8gm% and total white blood cell count was 11200 cells/mm3. ESR was 56 mm/hr. Serology test for IgA, IgM and IgG for TB were negative. Testing for Syphilis, HIV and sputum culture for Acid fast bacilli (AFB) were negative. X-ray chest was normal.
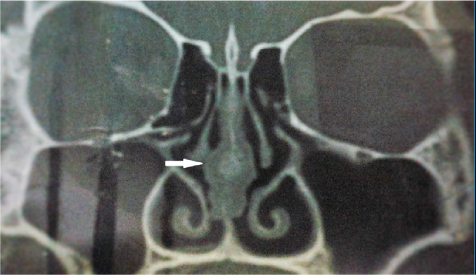
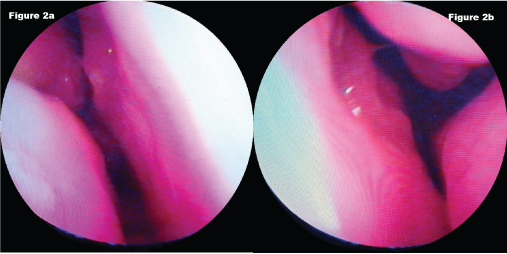
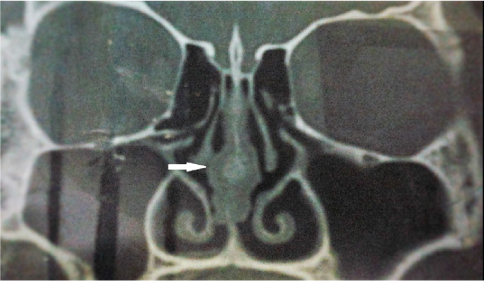
Computed Tomography Para nasal sinus (CTPNS) (coronal view) revealed a bulge in the posterior bony septum suggesting a septal mass [Table/Fig-1]. Diagnostic nasal endoscopic examination revealed an irregular bulge with a granular surface measuring 1 cm × 1.4 cm in the right posterior bony septum and septal mass measuring 1 cm ×1.5 cm in the left posterior bony septum [Table/Fig-2a,b].
Pre-operative computerized tomography para nasal sinus (CT PNS) coronal section showing septal mass. In this picture white arrow indicate the septal mass.
a) Pre-operative diagnostic nasal endoscopic examination shows the septal mass measuring 1 cm × 1.4 cm in the right posterior bony septum; b) Pre-operative diagnostic nasal endoscopic examination shows septal mass measuring 1 cm ×1.5 cm in the left posterior bony septum.
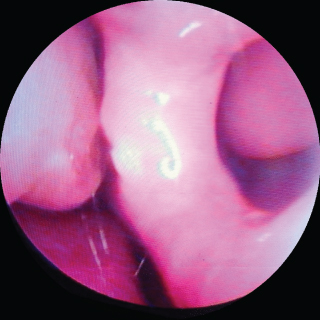
Transnasal endoscopic excision of septal mass was done under general anesthesia and postoperative endoscopic examination revealed posterior septal defect measuring 1.2 cm ×1.7 cm [Table/Fig-3].
Post-operative diagnostic nasal endoscopic examination showing posterior septal defect measuring 1.2 cm × 1.7 cm after septal mass excision.
The biopsy report revealed fragmented bony tissue and caseating granuloma composed of epitheloid cells, langhans type of giant cells suggestive of tuberculous granuloma of bony septum [Table/Fig-4]. The excised septal mass was positive for AFB on Ziehl-Neelsen staining [Table/Fig-5]. In this case, post-operative tissue culture for acid fast was not done due to the unavailability of lowenstein- jensen media and dickinson mycobacteria growth indicator tube in our hospital. The patient was started on category 1 Anti-tuberculosis therapy (Cat 1 ATT) in view of the above findings. ATT consists of multidrug combination tablet 4-D Plus (Isoniazid 300 mg, Rifampicin 600 mg, Pyrizinamide 1600 mg and Ethambutol 1100 mg) for first two months. This was followed by tablet Bicox-600 (Isonazid 300 mg and Rifampicin 600 mg) for next five months. The patient was well after five months, she had no episodes of nasal blockage. Due to patient’s poor economic status, the authors were unable to procure specific laboratory test for tuberculosis in this patient.
Histopathological examination (haematoxylin and eosin stain) picture showing tuberculous granuloma of bony septum. In this picture red arrows show lymphocytes and langhans multinucleated giant cells arranged in horseshoe pattern at the cell periphery. The black arrow indicates central caseous necrosis surrounded by few lymphocytes.
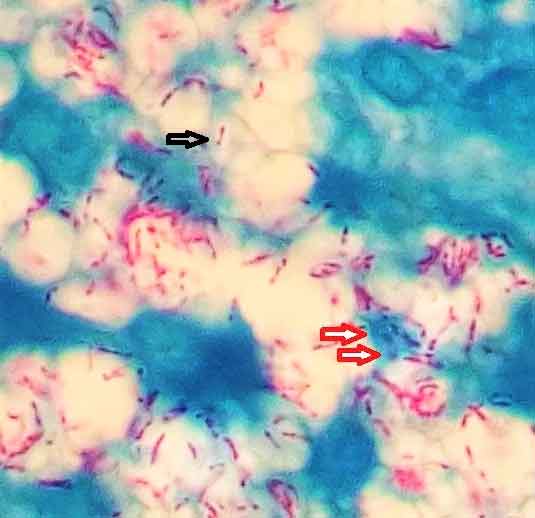
Ziehl-Neelsen stain of the septal mass specimen shows presence of multiple acid fast bacilli surrounding the langhans giant cell and the red arrows indicate langhans giant cell. In this picture black arrows indicate few acid fast bacilli in the area of caseous necrosis.

During the 14–month follow up, the patient was investigated with diagnostic nasal endoscopic examination and the result showed persistence of posterior septal defect measuring 1.2 cm × 1.7 cm [Table/Fig-6]. Surgical correction of septal defect was offered, but declined by the patient. The follow–up chest X-ray was normal [Table/Fig-7]. The patient was advised to have regular recall visits, for every six months. In this case, a good response to Cat1 ATT with the presence of typical caseating granuloma in the endoscopically excised mass from the septum confirmed the final diagnosis as nasal tuberculosis.
At 14-month follow–up, diagnostic nasal endoscopic examination shows persistence of posterior septal defect measuring 1.2 cm ×1.7 cm.
Follow–up chest X-ray was normal.
Discussion
TB is an infection caused by mycobacteriumtuberculosis and is prevalent in tropical countries. TB typically affects the lungs (Pulmonary TB) but frequently involves other organs (extra-pulmonary TB) [1]. Tuberculosis affecting the nasal mucosa is not common as the nasal mucosa is inherently resistant to TB. Till date, only 35 cases of nasal tuberculosis have been reported in medical literature [2–4].
Tuberculosis of the nasal mucosa is more common in adult young females than males. But there is no particular preponderance for any age group, ranging from 19 to 85 years. About one-third of the 35 reported cases of nasal tuberculosis were seen in the age group below 20 years. Due to non-specific symptoms of nasal tuberculosis, diagnosis in most cases remains challenging. Usually the commonest clinical presentation for nasal tuberculosis is nasal obstruction and catarrh. Confirmation of nasal tuberculosis is made by culture test with isolation of tubercle bacilli from the surgically excised specimen. AFB on gram-staining may also be detected in mycobacterium leprae infection and hence, is not specific for tuberculosis [4,5].
The differential diagnosis for tuberculosis of nose includes lethal midline granuloma, wegener’s granuloma, sarcoid, syphilis and fungal infection. Ziehl-Neelsen stain for acid-fast mycobacterial bacilli provides specificity of 98% but relatively low sensitivity of 65%. New diagnostic techniques include nucleic acid amplification tests provides good specificity of 96% but relatively moderate sensitivity of 78% whereas, Interferon γ assays provides specificity of 95% but relatively good sensitivity of 85% [6].
Polymerase Chain Reaction (PCR) method helps the identification of mycobacteria in a short time of 48 hours and it has sensitivity and specificity as 84% and 100% [7]. Culture remains the gold standard diagnostic test for tuberculosis and it has sensitivity and specificity as 63% and 98% [6,7].
Global tuberculosis report 2015 recommends treatment consisting six-month regimen of four first-line drugs: isoniazid, rifampicin, ethambutol and pyrazinamide for new cases of drug-susceptible TB [1]. The management of nasal tuberculosis mainly consists of ample anti-tuberculosis therapy with excisional surgery. In case of significant nasal obstruction, reconstructive plastic surgery for perforation of nasal septum may be required for cosmetic purpose [3].
Conclusion
Diagnosing nasal tuberculosis has been always been the biggest challenge for the otolaryngologist and oral diagnostician. Molecular techniques can be helpful in diagnosing, however the limitations due to sensitivity and specificity of these tests need to be borne in mind. Where available, and histopathology of the suspicious material, confirmed by culture remains the key for the diagnosis. Where facilities for culture are not available, for example in low resource settings, confirming the diagnosis of nasal tuberculosis is always based on successful response to therapeutic trial with anti-tuberculosis treatment.
[1]. World Health Organization. Global tuberculosis report 2015. World Health Organization: 2015 [Google Scholar]
[2]. Lai TY, Liu PJ, Chan LP, Primary nasal tuberculosis presenting with septal perforationJournal of the Formosan Medical Association 2007 106(11):953-55. [Google Scholar]
[3]. Dixit R, Dave L, Primary nasal tuberculosisLung India 2008 25(2):102 [Google Scholar]
[4]. Ozer M, Ozsurekci Y, Cengiz AB, Özçelik U, Yalçın E, Gököz Ö, Primary nasal tuberculosis in a 10-year-old girlCanadian Journal of Infectious Diseases and Medical Microbiology 2016 :2016 [Google Scholar]
[5]. Munck K, Mandpe AH, Mycobacterial infections of the head and neckOtolaryngologic Clinics of North America 2003 36(4):569-76. [Google Scholar]
[6]. Masterson L, Srouji I, Kent R, Bath AP, Nasal tuberculosis–an update of current clinical and laboratory investigationThe Journal of Laryngology & Otology 2011 125(02):210-13. [Google Scholar]
[7]. Canbolat NA, Tezcan E, Yanık S, Akkoca AN, Ozdemir ZT, Kaynar A, Primary nasal tuberculosis: Case ReportAmerican Journal of Health Research 2014 2(5):316-18. [Google Scholar]