Hemiarthroplasty is a common surgery done for displaced fractures of neck of femur [1]. Usually femoral neck fractures are associated with higher morbidity and mortality [2]. The uncertainty of union after internal fixation is due to physiological quality of the bone, osteoporosis and increased intra-capsular pressure. Even if union occurs, there is a chance of avascular necrosis of the head of the femur. Moreover, there are high chances of secondary osteoarthritis. All this leads to an increased number of surgeries, which increases the morbidity and mortality of the patients. There is up to 25% mortality in these patients, so rather than considering internal fixation in these patients, prosthetic replacement is better option for displaced fracture neck of femur. Replacement of the head of the femur alone is hemi replacement arthroplasty. It may be either unipolar or bipolar replacement arthroplasty.
Various prostheses are in use for arthroplasty, but the concern with the prosthesis is stem loosening and migration. To overcome these, several strategies are used such as achieving a geometrically stable press fit between bone and implant, stimulating bone growth and use of Polymethyl Methacrylate (PMMA) cement. Among these strategies, use of PMMA cement offers definite advantages as it acts as a grouting agent to replace thinning trabecular bone, offering immediate interference stability between implant and bone, thus greatly simplifying rehabilitation. Bipolar arthroplasty was introduced to prevent or retard acetabular wear. These prostheses have a 22 to 32 mm head that articulate with a ultra-high density polyethylene liner of varying sizes. The liner is covered with polished metal outer head that articulates with the acetabular cartilage. Theoretically, hip motion primarily occurs at prosthetic joint and only secondarily at metal cartilage interface, minimizing articular wear.
There is evidence for use of cemented hemiarthroplasty resulting in greater anchoring and lesser periprosthetic fracture. However, cemented prosthesis may result in more mortality from haemodynamic instability and cardiopulmonary complications termed as ‘cement reaction’ or bone cement implantation syndrome [3,4]. In contrast, uncemented hemiarthroplasty procedures may result in loosening of prosthesis and post-operative fractures and thigh pain [5]. In addition, the procedure is less strenuous, and blood loss during procedure is low [6–8].
Bipolar hemireplacement arthroplasty prosthesis decreases the acetabular erosion and can be used in younger patients. It improves stability due to self-centring or self-aligning mechanism. Recently, many surgeons are evaluating effectiveness of cemented and uncemented hemiarthroplasty for fracture neck of femur. There is evidence for better results in terms of mobility, revision rates and thigh pain after cemented hemiarthroplasty in spite of longer duration of surgery and blood loss during the procedure [9,10]. However, a meta-analysis comprising of 7 randomised control trials has shown that, there is no difference between cemented and uncemented hemiarthroplasty in terms of mortality, range of movements, quality of life and reoperation rate [11,12]. The objectives of this study was to compare cemented and uncemented hemiarthroplasty in terms of blood loss during the procedure, postoperative complications, mortality, functional recovery and long term clinical outcome.
Materials and Methods
In a prospective study spanning for 8 years from January 2006 to January 2014 in a tertiary care centre, Bangalore, 52 cases of fracture neck of femur were selected. All patients aged more than 50 years with fresh and old fractures of neck of femur having calcarfemorale not less than 5 mm with normal acetabulum were included in the study. Patients who were less than 50 years of age, with active infection, associated medical illness like coronary artery disease and cerebrovascular disorders, pathological fractures, polytrauma and acetabular erosions were excluded. Institutional Ethics Clearance was obtained before the start of the study and written informed consent was taken from each patient before they were recruited for the study.
The patient’s demographic profile, including age, sex, address, occupation and complete history (with personal, past and co-morbid conditions) were noted. A detailed physical examination followed and any associated abdominal, thoracic, head and neck injuries were ruled out. The affected limb was thoroughly examined to rule out vascular or neurological injury. Ipsilateral knee was examined for associated injury. X-ray of pelvis (AP view) with both hip obtained by internally rotating both limbs by 15 degrees to offset the anteversion of femoral neck. AP view of pelvis allowed for comparison of involved side with contralateral side.
All patients admitted and selected for the operative method of treatment underwent the pre-operative work up with complete haemogram investigation, blood group typing and medical and surgical reference whenever indicated for operative fitness.
Preoperative preparation
All patients admitted and selected for the operative method of treatment underwent the pre-operative work up as the standard protocol as follows: haemoglobin, Complete Blood Count (CBC), blood urea, serum creatinine, serum bilirubin, serum electrolytes, blood group and Rh-typing, chest X-ray, ECG, 2D ECHO if required for cardiologist fitness and medical and surgical reference whenever indicated for operative fitness.
After anaesthetic fitness the patients were posted for surgery as early as possible with the fulfilment of following requirements:
Written and informed consent for surgery.
Adequate blood for transfusion in case of low Hb%.
Detailed pre-operative planning was done. Thickness of cortex of femur, medullary canal, type of fracture (Garden’s classification) and amount of calcar present was noted in each X–ray. Pre-operatively head size was measured radiologically in all patients but all sizes of the heads were kept for surgery.
Procedure that the patient has to undergo was explained and isometric quadriceps and hamstring exercises were taught pre-operatively to the patient.
Inj. Cefotaxime 1 gm IV was administered pre-operatively.
Xylocaine sensitivity test was done.
Grading of osteoporosis
Singh’s index based on trabecular pattern of the proximal femur was employed for grading osteoporosis. Grade 6: Normal with primary compression and tension trabecular pattern and secondary compression and tension trabecular pattern. Grade 5: Decrease in secondary trabecular pattern and the Ward’s triangle becomes prominent. Grade 4: Absence of secondary trabecular pattern with decrease in primary trabecular pattern. Grade 3: A break occurs in tension trabeculae. Grade 2: Loss of complete primary tension trabeculae. Marked reduction in compression trabecular pattern. Grade 1: Only a few compression trabeculae seen. Grade 3 and below was considerd as significant osteoporosis.
Anaesthesia
Epidural anaesthesia was used in 22 patients and spinal anaesthesia in 30 patients.
Prophylactic anti-deep venous thrombosis treatment
Patients were started on Injection clexane (enoxaparin sodium) 40 mg subcutaneous once daily, preoperatively and followed postoperatively till ambulation. The previous night before surgery the dose was skipped.
Operative method
Hip was opened by Moore’s Posterior approach. After the femoral head was extracted, the femoral neck was nibbled in such a way that enough of calcar (minimum of 0.5 inches) remained to support the medial aspect of prosthesis. Then an awl or straight curette was inserted in line with femoral shaft to aid in entering diaphyseal medullary canal. A notch was made in the postero-superior portion of the neck to help maintain anteversion of 10°-15°. Then with an appropriate rasp medullary canal was rasped in valgus and 10-15 degrees of anteversion relative to the plane in which the knee joint axis lies.
Decision for cementing the canal
The decision for cementing was taken based upon the pre op X-ray and the condition of femoral bone. In case the prosthesis was also loose, the canal was cemented. Usually 40 mg of cement was used.
Preparation of bone cement
Regular PMMA bone cement is supplied as two sterile components. Powder packet – contains particles (10 to 150 microns in diameter) of PMMA, about 10% barium sulphate and a polymerization initiator (approx. 1% benzoyl peroxide) and Liquid vial–contains methyl methacrylate monomer and an activator (about 3% of DMP toluidine) that promotes cold curing process. Manual mixing technique is used, in which the liquid is added to the powder and mixed by stirring. Initial period is the dough time, the time from the beginning of mixing until the cement does not stick to non-powdered surgical gloves, usually 2-3 minutes. Working time is the time from the end of the dough time until the cement is too stiff to manipulate usually 5-8 minutes. Setting time is the sum of two and is typically 8-10 minutes. Once the dough of the cement is made the packed ribbon gauze is removed and the cement inserted into the medullary canal by cement gun after the cement restrictor is inserted.
Insertion of prosthesis
The appropriate size of prosthesis was seated in the prepared medullary canal with the 10-15 degrees of anteversion and valgus position. The prosthesis was impacted with gentle blows in to the medullary canal. After the cement is set properly the prosthesis was reduced into the acetabulum by gentle traction in the extended position of the knee, with minimal external rotation terminally. Difficult reductions were achieved using Murphy’s skid. While reduction, care was taken to prevent dislodgement of the outer head, and there was no dislodgement of the prosthesis in present study. The hip was tested for full range of movements and stability intra-operatively while closure of the wound, capsule and external rotators were sutured back. The wound was closed meticulously in layers over a suction drain maintaining haemostasis throughout the procedure and sterile dressing was applied. Same procedure was followed in the uncemented cases without the cementing step [Table/Fig-1].
Final Prosthesis seating on the calcar.

Duration of surgery from incision to closure was noted, blood loss during the procedure was calculated, and whether prosthesis can be easily reduced and difficulty in reduction was noted. Blood loss was assessed and blood transfusion carried out if required.
Follow up
After getting check X–ray and confirming the prosthesis position, patients were made to ambulate with the help of walker. In cemented hips full weight bearing was done immediately and in case on uncemented type it was progressed from partial weight bearing to full weight bearing over a period of 4-6 weeks. By the time of discharge, patients were made to ambulate with the help of walker.
The follow up was carried out at 6 weeks, 3 months, 6 months, 1 year and every year afterwards. At each follow up clinical evaluation was done for limb length discrepancy, thigh pain, rotation of the limb, gait pattern and range of movements. Harris Hip Score evaluation was done at each follow up. Radiological evaluation was done at each follow up for calcar length, periprosthetic fractures. Other complications like superficial infection, deep infection, urinary tract infection, bed sores, and any medical complications if present were noted.
Statistical Analysis
Results on continuous measurements are presented on mean±SD and results on categorical measurements are presented in percentages. Significance is assessed at 5%. Student’s t-test (two-tailed, independent) has been used to find the significance of study parameters on continuous scale between two groups.
Results
Demographic characteristics of the patients are presented in [Table/Fig-2].
Baseline and demographic characteristics of patients.
| Characteristics | n = 52 |
|---|
| Age in years (mean±SD) | 70 (±2.2) |
| Range | 50 – 100 |
| Sex : male : female | 22:30 |
| Side: right : left | 24:28 |
| Garden’s type |
| III | 14 |
| IV | 38 |
| Mode of injury |
| Trivial fall | 31 |
| Fall | 13 |
| RTA | 8 |
| Medical illness | 36 |
Bipolar hemiarthroplasty outcomes
Out of 52 cases, 24 were treated with cemented and 28 were treated with uncemented bipolar hemiarthroplasty. Mean duration of follow up was 59.3 (±7.3) months. Mean blood in 67% of the patients during hemiarthroplasty was between 150-200 ml. It was calculated by number of fully soaked mops used during the procedure and amount of blood collected in the suction machine (total amount – normal saline already there in the machine). Each mop, which was used in our institution were absorbing about 40 ml of blood. In cases of cemented bipolar group, it ranged from 100-200 ml.
Anaemia was the most common associated medical illness in both groups. Diabetes mellitus was noted in six patients. Number of days of hospital stay is tabulated in [Table/Fig-3] and most patients in both groups stayed for 8 to 14 days. It varied from 3 days to 14 days, with mean stay of 8.96±1.55 days in the cemented group and 8.75±1.96 in the uncemented group. There was no change in limb lengths in both groups. Shortening was noted in two patients in cemented group and four patients in the uncemented group, which was 1.5 cm. However, a significant gait alteration was not noticed and pain was occasional and subsided with analgesics. These patients were walking with support using walking aid (walker). There was no rotation of limb in most patients. In cemented bipolar group, three patients had external rotation deformity, which ranged from 20 to 30 degree. This was persistent until last follow up. It was also noted that, one of them had shortening during the last follow up. In uncemented bipolar group, 4 patients had external rotation deformity, which ranged from 20 to 35 degree. This was persistent until last follow up.
Characteristics during and after surgery for patients according to hemiarthroplasty performed along with functional outcomes; †p<0.05.
| Parameter | BipolarCemented(n=24) | BipolarUncemented(n=28) |
|---|
| Blood loss |
| 100-150 ml | 5 | 12 |
| 150-200 ml | 19 | 16 |
| Head size |
| 40-50 | 19 | 23 |
| >50 | 5 | 4 |
| Hospital stay | | |
| 3-7 days | 1 | 6 |
| 8-14 days | 23 | 22 |
| Limb length |
| Nil | 22 | 22 |
| Lengthening | 0 | 2 |
| Shortening | 2 | 4 |
| Rotation of limb |
| Nil | 21 | 24 |
| Externally rotated | 3 | 4 |
| Complications |
| Nil | 20 | 28† |
| Deep infections | 1 | 0 |
| Superficial infections | 3 | 0 |
| Harris Hip score |
| 3 months | 78.6±10 | 78.5±6.5 |
| 6 months | 82.5±8.3 | 82.5±6.2 |
| 1 year | 86.2±6 | 85.2±5.8 |
| Last Follow – up | 86.5±6 | 85.3±5.8 |
| Final clinical result |
| Poor | 0 | 1 |
| Fair | 3 | 1 |
| Good | 10 | 19 |
| Excellent | 8 | 6 |
Post-operative infection was noted in 4 patients, 3 cases were superficial infection and 1 patient had deep infection in the cemented bipolar group and superficial infection was seen at 5th-6th post-operative day, when there was congestion and inflammatory signs around the operated wound and it was painful. These cases were treated with extension of IV antibiotics for 7 days and were switched over to oral antibiotics for another 2 weeks. The outcome was satisfactory. During this period, patients were immobilized.
In one case, deep infection was noted. This patient was treated with IV antibiotics and regular wound dressings. However, even after 2 weeks, there was persistent infection. Therefore, under spinal anaesthesia, thorough wound debridement was done. After keeping drain, skin closure was done. Drain was kept till 4th day, and IV antibiotics were continued. Wound healed without any further complication. This patient had Diabetes Mellitus since 12 years and had a history of poor wound healing in previous surgery (she was operated for tendo Achilles rupture), which took about 3 months to heal. It was also noted that, there was reaction to the suture materials, which were used. Complications are significantly more in cemented group with p=0.039. In the present study, no case of deep vein thrombosis, pulmonary embolism or cerebrovascular accident was encountered.
No mortality occurred during admission and within 12 weeks after surgery. However, four patients died; two patients due to myocardial infarction (at 12 months post-surgery) and one patient died due to bronchopneumonia (at 18 months post-surgery) and one due to road traffic accident.
Total functional range of movement found in the present study for all the patients varied between 160 to 300 degrees.
Prosthesis snuggly fitted the acetabular cup and no disproportion in any case was noted. More than 4 mm joint space is indicative of smaller prosthesis and less than 2 mm indicative of bigger prosthesis. Periprosthetic osteolysis or loosening (more than 2 mm osteolysis around the implant) was not seen in the present study. No acetabular erosions were noted in any of the patients at the last follow up of 21 months [Table/Fig-4].
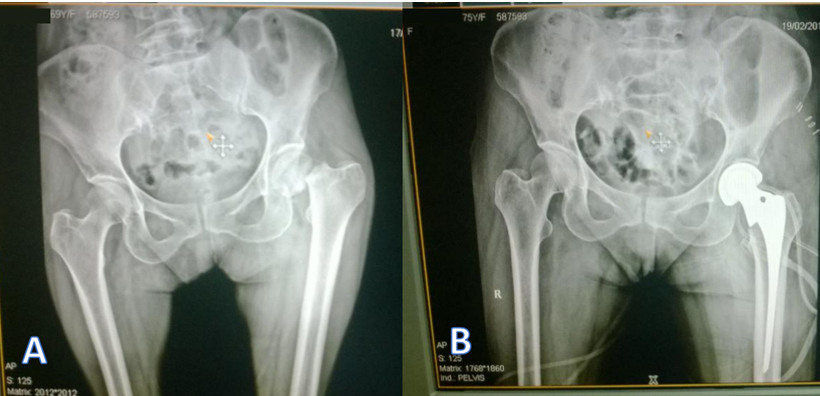
Pre-operative (a) and immediate post-operative; (b) X-rays of fracture neck of femur treated with cemented bipolar hemiarthroplasty.
Harris Hip score
There was no statistically significant difference in Harris hip scores in cemented and uncemented hemiarthroplasty patients at end of 6 months, 1 year and final follow up.
All cases were followed-up regularly and no case was lost during 1 year follow up. No cases of secondary fractures were noted and no re-operation were done.
Discussion
With increasing longevity, the problems of hip and surgical procedures to address this are also increasing. Osteoporosis and comorbid conditions add to the complexity of management. With limited evidence for cemented hemiarthroplasty for improved functional outcome and one of the meta-analysis showing increased post-operative mortality [13], this study finds a niche in bipolar hemiarthroplasty usage. A 5 year follow up randomized trial by Langslet E has shown that, there is no difference in functional outcome between two procedure [14].
All procedures were done via posterior approach as per current practices. In the present study, the blood loss ranged from 100-280 ml. Many previous surgeons report a higher blood loss during the procedure. Overall, including the present study, all agree that blood loss in uncemented hemiarthroplasty procedure is less [11–13,15]. The head sizes used in the present study varied from 37 to 51. In cases of Bipolar Prosthesis, sizes which were commonly used were 39, 41 and 43 [16].
No mortality occurred during admission and within 12 weeks after surgery. At the end of 6 months, no mortalities were noted. After one year of the surgery, four patients died due to various causes. Contrary, there are many studies revealing patients death specially after cemented hemiarthroplasty procedure [1,11–13,17]. No case of re-operation was noted in the present study. There were no case of loosening in present study, all patients were happy with the replacement procedure and they were carrying out all the routine activity of pre fall level. Reoperation rate as high as 20% is reported in some studies [15]. Soderman P and Malchau H has validated use of Harris hip score to evaluate the outcome of hip replacement procedures [18]. Figved W et al., in their study of uncemented Bipolar arthroplasty reported, an average Harris hip score was 72 after 3 months [4]. In a similar study, Annappa R et al., had reported mean Harris hip score of 89.25 in cemented bipolar group and 83.5 in bipolar group [19]. Our study is in accordance with such studies.
No case of loosening noted in the present study, with follow up of up to 21 months. Though, in literature elaborate classification regarding post-operative loosening of the prosthesis was noted, we did not make use of them as there was no radiologically detectable loosening during follow up [20–22]. Final functional outcome between cemented and uncemented bipolar prosthesis on functional basis did not show any significant difference in the long-term follow up (p=0.205.) This was the same outcome as compared with the literature [9–11,17,18]. In this study we have not considered the brand of the implant used. There are several studies reporting diversity of implants used to treat displaced hemiarthroplasty [11]. However, the design and brand of implants are not addressed in many studies.
Limitation
We could not do a long term study, this would have shown the long term outcome of cemented and uncemented hemiarthroplasty. Such studies show light on post-operative periprosthetic femoral fractures. Measure of health-related quality of life using EQ-5D index would give an objective evaluation of functional outcome.
Conclusion
No significant difference was noted between the cemented and uncemented hemiarthroplasty procedures on long term follow up in terms of functionality. No re-operations and no mortality reported. Cemented hemiarthroplasty had more blood loss and minimal post-operative complications.