Choroidal Metastasis as Initial Presentation in Adenocarcinoma of Lung: A Case Report
Saroj Kumar Das1, Tapan Kumar Sahoo2, Sucheta Parija3, Saroj Kumar Das Majumdar4, Dillip Kumar Parida5
1 Senior Resident, Department of Radiation Oncology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
2 Senior Resident, Department of Radiation Oncology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
3 Associate Professor, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
4 Assistant Professor, Department of Radiation Oncology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
5 Professor, Department of Radiation Oncology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sucheta Parija, Associate Professor, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar-751019, Odisha, India.
E-mail: suchetaparija@yahoo.com
Vision impairment as an initial presentation detecting choroid metastasis in primary lung cancer is rare. Prevention or treatment of visual loss and improvement in quality of life can be achieved by treatment of intraocular metastasis. The survival of the patient in choroid metastasis with lung primary is poor with the median survival being 3.3 months. However, proper treatment may increase the quality of life and survival to an extent. We report a case of adenocarcinoma of lung in a female patient, presented initially with visual impairment as a result of choroidal metastasis and treated with external beam radiotherapy for choroidal metastasis followed by palliative chemotherapy. The patient was survived with improved vision and quality of life since last 12 months of diagnosis.
Lung primary, Prognosis, Vision impairment
Case Report
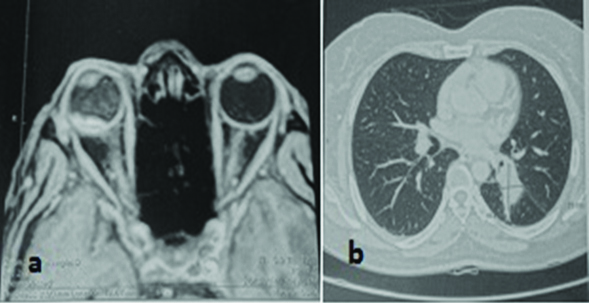
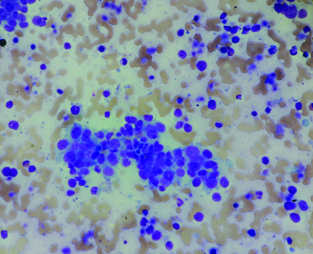
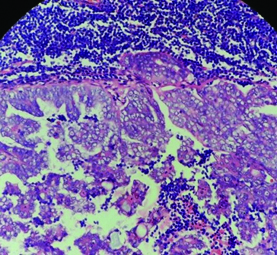
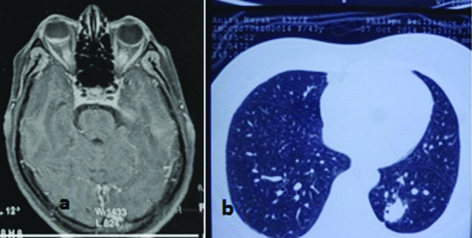
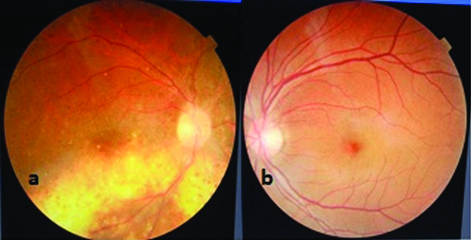
A 42-year-old female presented with blurring and diminution of vision in right eye. She was a nonsmoker and had no past relevant medical history. Ophthalmological examination revealed exudative retinal detachment with choroidal lesion compatible with metastasis in right eye. The left eye was normal. Visual acuity in right eye was hand movement and in left eye 20/20. Intraocular pressure was 12 mmHg in right eye and 14 mmHg in left eye. MRI brain and orbit with contrast revealed T2 hypointensive elliptic lesion showing some amount of T1 hyperintensity and GRE blooming in periphery of lesion situated in posterior chamber of right eye globe [Table/Fig-1a]. A choroidal mass as initial examinations without proof cannot suggest metastasis of any region, to rule out primary, further examinations were done. Contrast Enhanced Computed Tomography (CECT) scan of thorax showed multiple small solid nodules seen in bilateral lung fields and a small mildly enhancing solid mass lesion of size 40 mm x 22 mm seen in left lower lobe in posterior basal segment [Table/Fig-1b]. Ultrasound guided Fine Needle Aspiration Cytology (FNAC) from the mass lesion suggestive of adenocarcinoma [Table/Fig-2] and biopsy from left supraclavicular lymph node was metastatic adenocarcinoma [Table/Fig-3]. Epithelial Growth Factor Receptor (EGFR) mutation was positive for Exon 19.1. The patient was treated with palliative radiation therapy to both eyes 30Gy/10 fractions followed by six cycles of combined chemotherapy regimen consisting of pemetrexed and carboplatin. Post radiotherapy response evaluation with Magnetic Resonance Imaging (MRI) brain and orbit showed a small residual nodular soft tissue lesion in the right eye globe [Table/Fig-4a]. Post radiotherapy and chemotherapy MRI suggestive of 80%-90% regression in size of right eye choroidal mass lesion. Post chemotherapy CECT scan of thorax and abdomen evaluation revealed an ill-defined soft tissue attenuation lesion in left infrahilar region in apical and medial basal segment of left lower lobe with satellite metastatic nodules in left upper and right middle lobes with metastatic lymph nodes in mediastinum and left parahilar regions [Table/Fig-4b]. There was considerable regression in size and number of metastatic nodules when compared to the pretreatment CECT scan. In view of good response, she received another four cycles of maintenance pemetrexed. After four cycles of maintenance chemotherapy, she was again evaluated with contrast MRI brain and orbits, and CECT scan of thorax and abdomen. The imaging studies showed no lesion in the eye globes and brain with regression in the size and number of lesions in lung. Best corrected visual acuity was improved to 6/12. Fundus examination showed regression of choroidal lesion with no retinal detachment [Table/Fig-5a]. Left eye fundus examination was found to be within normal limits [Table/Fig-5b]. In view of good response she was planned for continuation of maintenance chemotherapy.
a) T1 contrast MRI showing enhancing hyperintense lesion noted in choroid of right globe near the optic nerve head with increased signal intensity in the vitreous; b) Lung window of axial CT scan showing solid mass lesion in left lower lobe lung.
Leishman stain 200X: Malignant cells arranged in acinar pattern in a background of inflammatory cells, macrophages and RBCs.
H&E 200X: Nests of carcinomatous deposits in the lymph node showing glandular differentiation.
a) T1 contrast MRI showing small residual lesion in choroid of right eye; b) Lung window of axial CT scan showing reduction in size of lesion in the left lower lobe lung.
a) Fundoscopy examination showing choroidal lesion regression with treatment scar; b) Fundoscopy examination showing normal fundus of the left eye.
Discussion
Melanoma is the most common primary choroid tumour. Malignant tumours from distant organs of the body can spread to eye. Breast is the most common site for choroid metastasis followed by lungs. Lung constitutes approximately 30% of choroid metastasis. The incidence of metastasis of lung carcinomas into choroid is 2%-6.7% [1]. The symptoms of vision impairment help in discovery of these tumours. Metastatic tumour of the eye presenting as the first sign of disseminated cancer is rare [2]. Loss of visual acuity as a primary symptom in lung cancer is very uncommon. The incidence of choroidal metastasis with lung cancer is 2%-7% [3,4]. Though choroid metastasis as initial presentation is rare, patient presented with an ocular tumour should undergo a thorough systemic examination. The possibility of a primary malignancy from distant organ should be ruled out before declaring primary choroidal tumour. We report a case of adenocarcinoma lung in a 42-year-old female patient with initial presentation of diminution of vision due to retinal detachment as a result of choroidal metastasis. This case report highlights that choroidal metastasis without a known primary should be supplemented with systemic as well as imaging studies.
Metastatic carcinoma to eye, particularly the choroid is uncommon. Uveal tract is most commonly involved in the ocular metastasis with choroid (88%) being the most common site of involvement among the tract followed by iris (9%), and cilliary body (2%) [5]. Breast is the most common site among female for intraocular metastasis constituting 37%-41%, whereas, the incidence of lung primary with choroid metastasis in female is not more than 7% [6,7]. Choroid metastasis involves choroid layer of the eye. The reason for this unusual site as the target for secondary metastasis is not known. High vascularity nature may be a possible explanation for choroidal metastasis [8].
Choroid is the most common metastasis into the eye. The initial presentation of retinal detachment due to ocular metastasis is rare, as in the present case [9]. The present case is with a unilateral, solitary lesion along the superior temporal arcade of the right eye. Most of the choroidal metastatic lesions are seen in the posterior pole, probably due to relatively greater blood flow to that area [10]. Multiple foci and bilateral involvement are frequently seen in choroidal metastasis. In 20%-40% of choroidal metastases are bilateral [11]. The primary site of organ in choroidal metastasis for female is the breast, followed by lung, gastrointestinal tract, pancreas, melanoma, and others. However, for male, the primary sites are the lung, followed by gastrointestinal tract, pancreas, prostate, kidney, melanoma, and others [10,12].
Choroidal metastasis diagnosed primarily on clinical findings needs supplementation of imaging studies. Ultrasonography, fluorescein angiography, Optical Coherence Tomography (OCT), FNAC are various modalities for diagnosis. MRI brain and orbit with gadolinium enhancement is necessary to rule out brain metastasis as it may associate concurrently with choroidal metastasis in 22% of cases [13]. Choroidal metastatic lesions are usually fluorescent in the early phases of fluorescein angiography study and become progressively hyperfluorescent in the late phases [14]. An echogenic sub-retinal mass with diffuse, ill-defined borders is seen on B-scan ultrasound. Retinal detachment is common and moderate sound attenuation is usually seen in the lesion [15]. Primary choroidal melanoma, haemangioma, inflammatory granuloma can be the differential diagnosis.
The survival of the patient in choroid metastasis with lung primary is no more than six months [16]. Ocular metastasis treatment is palliative as the presence of metastasis suggests haematogenous spread. The aim of treatment is to increase quality of life and preserve vision [3]. Choroid metastasis not destroying the centre of the retina offers the best hope for improving the vision. External beam radiotherapy, plaque radiotherapy, surgical resection, transpupillary thermotherapy, intravitreal chemotherapy are the treatment options available [2]. Radiotherapy is an effective treatment modality for ocular and choroidal metastasis. Almost all patients with choroid metastasis can be treated with external beam radiotherapy. The dose of external beam radiotherapy for choroidal metastasis in case of primary from distant organ is 30 Gy in 10 fractions [2]. The use of chemotherapy for choroidal metastasis is not widely reported in literature. Surgery is rarely used in the treatment of ocular metastasis. We are reporting a case of adenocarcinoma lung with bilateral lung nodules and choroidal metastasis. The patient showed encouraging response to both palliative radiotherapy and subsequent chemotherapy. The subjective response was to the tune of 70%. The present case was survived with the disease since 13 months of starting treatment.
Both the primary tumour type and local tumour invasion are the major factors determining the survival for choroidal metastasis. The survival of choroid metastasis with lung primary ranges from 0.5 months to 19 months [2]. The present case responds well to treatment and is now better 12 months after the diagnosis.
Conclusion
Any choroidal lesion should be taken as secondary spread until and unless proven otherwise. Diagnosis is mainly based upon clinical findings and imaging studies. Radiotherapy is the cornerstone of therapy for choroidal metastasis and helps to improve vision and quality of life. Whenever feasible, chemotherapy can be administered depending on primary tumour. Careful treatment of choroidal metastasis may improve the vision and possible quality of life.
[1]. Namad T, Wang J, Tilton A, Abdel Karim N, Bilateral choroidal metastasis from non-small cell lung cancerCase Rep Oncol Med 2014 2014:858265 [Google Scholar]
[2]. Singh A, Singh P, Sahni K, Shukla P, Shukla V, Pant NK, Non-small cell lung cancer presenting with choroidal metastasis as first sign and showing good response to chemotherapy alone: a case reportJournal of Medical Case Reports 2010 4:185 [Google Scholar]
[3]. Asteriou C, Konstantinou D, Kleontas A, Paliouras D, Samanidis G, Papadopoulou F, Blurred vision due to choroidal metastasis as the first manifestation of lung cancer: A case reportWorld Journal of Surgical Oncology 2010 8:2 [Google Scholar]
[4]. Simsek T, Ozdamar Y, Berker N, Choroidal mass as an initial presentation of lung cancerMed Oncol 2008 25:400-02. [Google Scholar]
[5]. George B, Wirostko WJ, Connor TB, Choong NW, Complete and durable response of choroid metastasis from non-small cell lung cancer with systemic bevacizumab and chemotherapyJ Thorac Oncol 2009 4(5):661-62. [Google Scholar]
[6]. Fernandes BF, Fernandes LH, Burnier MN, Choroidal mass as the presenting sign of small cell lungCan J Ophthalmol 2006 41:605-08. [Google Scholar]
[7]. Kreusel KM, Wiegel T, Stange M, Bornfeld N, Hinkelbein W, Foerster MH, Choroidal metastasis in disseminated lung cancer: frequency and risks factorsAm J Ophthalmol 2002 134:445-47. [Google Scholar]
[8]. Ascaso FJ, Castillo JM, García FJ, Cristóbal JA, Fuertes A, Artal A, Bilateral choroidal metastases revealing an advanced non-small cell lung cancerAnn Thorac Surg 2009 88:1013-15. [Google Scholar]
[9]. Saha K, Basuthakur S, Jash D, Maji A, Lung cancer presenting as visual impairmentSouth Asian Journal Cancer 2013 2(2):86 [Google Scholar]
[10]. Ferry AP, Font RL, Carcinoma metastatic to eye and orbit: a clinicopathologic study of 227 casesArch Ophthalmol 1974 92:276-86. [Google Scholar]
[11]. Shields JA, Diagnosis and management of intraocular tumors 1983 St LouisMosby [Google Scholar]
[12]. Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE, Survey of 520 eyes with uveal metastasesOphthalmol 1997 104:1265-76. [Google Scholar]
[13]. Koçak Z, Tabakoğlu E, Benian O, Bayir G, Unlü E, Uzal C, Bilateral choroidal metastases as an initial manifestation of small-cell carcinoma of the lungTuberk Toraks 2006 54(1):61-64. [Google Scholar]
[14]. David DL, Robertson DM, Flourescein angiography of metastatic choroidal tumorsArch Ophthalmol 1973 89:97-99. [Google Scholar]
[15]. Shammas HJ, Atlas of ophthalmic ultrasonography and biometry 1984 St. LouisCV Mosby Co [Google Scholar]
[16]. Fernando AJ, Fernandez CF, Garcia RA, Optical coherence tomography. Characteristics of choroidal metastasisOphthalmol 2005 122:1612-19. [Google Scholar]