Proliferative Fasciitis (PF) is a benign lesion with histologic and clinical features overlapping with those of malignant soft tissue tumours. Its occurrence in children is considered very rare. We present a case of PF appearing as a painful, red, gradually increasing in size lesion, during a period of a few weeks, on the finger of a five-year-old boy compromising the dermis and subcutaneous tissue. We were able to locate literature on 20 paediatric PF cases, which we review. Only five of these focus on the clinical data, the rest describing mainly histological findings. It is the first reported paediatric case appearing on the finger.
Child, Cutaneous tumour, Dermis, Finger, Pseudotumour, Sarcomatous, Soft tissue
Case Report
A small painless red papule was noticed on the pulp of the median finger of the right hand of a five-year-old boy. No medical advice was asked for and no treatment was applied for the lesion until three weeks later, when it became more painful, red and gradually increased in size. At that time the boy visited a surgery department where the lesion was incised because it was thought of being a panaris. Following this treatment the lesion continued to grow, becoming more red and painful. Ten days after, he visited our department with a firm, red, and painful mass in the pulp, extending as a firm palpable cord on the ulnar side of the middle phalanx [Table/Fig-1]. It was slightly painful and tender on pressure. The child and parents did not report any injury on the finger. The movements of the finger were only slightly compromised [Table/Fig-1].
A mass lesion on the finger. The sign of previous puncture can be seen.

The lesion was biopsied and the microscopic findings showed diffuse growth of fibroblasts with areas of increased cellularity alternating with paucicellular regions and hyalinization. The stroma showed increased capillary vascularity. The cells were spindle shaped and between them large ganglion–like cells with abundant eosinophilic cytoplasm were present. Mitoses were very few. Immunohisto-chemical staining CD-68 revealed dispersed histiocytes. The findings were reported as consistent with PF. There was no evidence of malignancy.
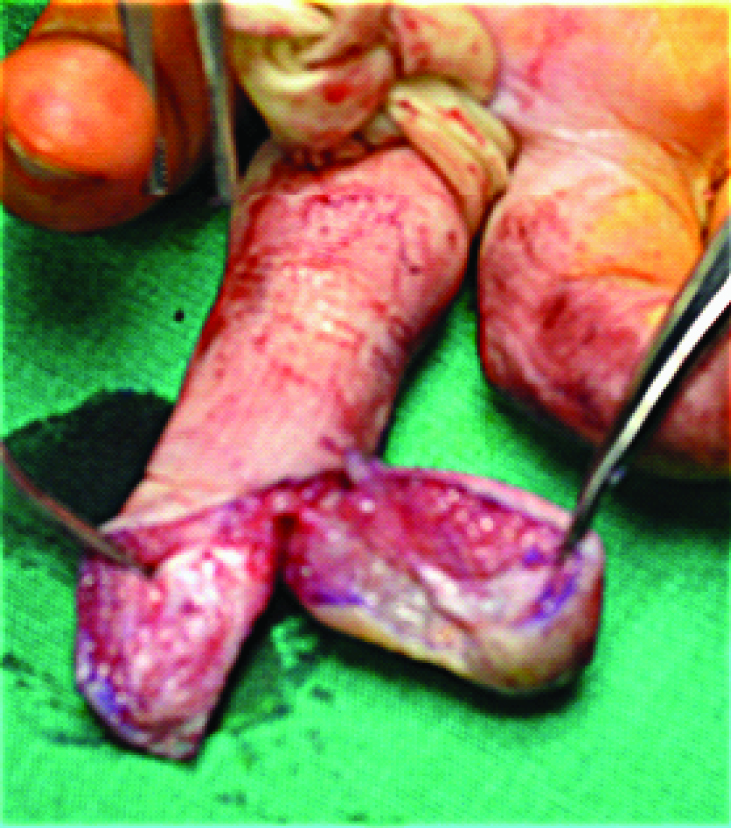
Following the biopsy, the lesion continued to grow and complete excision of the lesion was undertaken two weeks later. It was carried out through an incision conforming around the limits of the lesion [Table/Fig-2,3].
Line drawn around the limits of the lesion. (Left to right)

Incision carried out along the line and excision of the lesion.
Two free full thickness skin grafts harvested from the groin were used to cover the remaining raw area after approximation of the wound edges. The specimen was 3x1.8x1.2 cm in dimensions, whitish and with fibroelastic consistency. Histology findings confirmed those of the initial biopsy. Additionally, immunohistochemical staining with Smooth Muscle Actin (SMA) was performed, staining spindle cells with characteristics of myofibroblasts. Spindle cells as well as ganglion–like myofibroblasts were present both in the dermis and the subcutaneous tissue. Mitoses were scarce with multiplication index<5% and there was no evidence of malignancy.
The postoperative course was uneventful and the finger achieved full range of motion. No recurrence was observed during one year and a half of follow up [Table/Fig-4].
Complete healing two months postoperatively. (Left to right)

Discussion
PF is a self-limiting, benign, reactive fibroblastic proliferation considered as a pseudosarcomatous lesion because of its microscopic features overlapping with those of malignant soft tissue tumours [1–3]. It is a very rare disease, concerning mainly middle age adults and its incidence has not been estimated. A rough measure for the incidence derives from a review of the published cases in Japan until the year 2001, in which only 20 cases are assembled. The patients were 20 to 75-year-old (mean, 57.6 years) [4]. We were able to trace in literature only 20 cases of PF in children up until now. For the majority of these cases clinical data were insufficient and only histological data appear in detail [Table/Fig-5a]. For the remaining five reviewed cases clinical data could be retrieved [Table/Fig-5b] [1,5–11].
Summary of the published childhood Proliferative Fasciitis cases [1,5–11].
| Authors | M/F | Age | Size | Pain | Treatment | Localization | Time since appeared | Trauma |
|---|
| a) Pathology oriented reviews and case reports. |
| Meiss Meiss [1] | 9M 2F | 2,5-13y | 1.5-3, 11cm | | 10 excised | 5 le, 3 ue, 2 hn, 1 ch | 1- 1.5 mo | 1 yes |
| Ghadially [7] | F | 13y | 7 gr | | Excision | chest wall | | |
| Rosa [8] | M | 5y | 2 cm | | | groin | Several mo | |
| F | 7y | 2.2 cm | yes | | toe | | |
| F | 7y | 2.5 cm | | | thigh | | |
| b) Clinically oriented case reports. |
| Lorenc ZP [5] | F | 7y | 4 cm | yes | Excision | palm | 3 mo | no |
| Lorette G [9] | F | 6y | 2 cm | no | Biopsy, excision | thigh | 2 mo | no |
| Margo G [6] | M | 13y | 2.5 cm | no | excision | retroauricular | >mo | no |
| Yamaga K [10] | M | 13y | 4.5 cm | yes | Biopsy, excision | leg | 2mo | no |
| Bautista MJ [11] | M | 16y | 1.2 cm | yes | excision | orbit | 5 mo | no |
| Our case | M | 5y | 3 cm | yes | Biopsy, excision | finger | > mo | no |
(M/F: Male/Female, y: year, mo: month, hn: head and neck, ue: upper extremities, le: lower extremities, ch: chest wall)
PF is considered as a repair reaction in soft tissue, where minor traumas and inflammation are frequent [3]. However, only rarely some type of injury is reported to precede the resulting proliferation, raising the possibility that other causes may play a role in its development [2]. Among adult patients, 7-33% had a history of trauma adjacent to the involved area [4–6]. Among the reviewed children’s clinical data, as well as in our case, no trauma was reported.
One must be aware of the histological features of PF that can cause confusion with malignancies especially in paediatric lesions [1,7,8,11]. These features were pointed out by Meis JM and Enzinger FM [1] who studied the slides of 11archived cases of paediatric PF and myositis, seven of which were histologically diagnosed previously as “sarcomatous lesions” or Rhabdomyosarcomas (RMS) and were treated aggressively.
Childhood lesions are generally well circumscribed, lobulated, extremely cellular and with less collagen production than in adults [1]. Mitotic figures may be numerous, in both adult and paediatric PF cases, but are never atypical [4]. In our case these were few, less than 5%. Also, paediatric lesions are often well circumscribed, with a more solid growth pattern. Reticulohistiocytoma presents with ganglion-like myofibroblasts with more prominent nucleoli and more amphophilic cytoplasm. Xanthogranulomas have more multinucleated cells with touton giant cells and an inflammatory background which includes eosinophils [4]. No particular immunohistochemical stain would distinguish xanthogranuloma or reticulohistiocytoma from PF [4].
The clinical characteristics of PF are those of a mass-forming lesion, usually painful, demonstrating an aggressive local behaviour, which may increase in size rapidly during a few weeks time, typically attaining a maximum size of about 3 cm [3]. RMS and non-RMS soft tissue tumours are strong diagnostic alternatives to PF [4]. They usually present as painless masses without associated symptoms, except when compromising adjacent organ function. There may be palpable regional lymphadenopathy [12].
The 21 reviewed paediatric cases, including our own, concerned 14 boys and seven girls aged from 2.5 months to 16 years (Mean 7.8 years, median seven years). Four lesions appeared on the head and neck (19%), five on the upper extremity (24%), two on the trunk (10%) and nine on the lower extremity (43%) [5,9–11]. The distribution is similar to that observed in adults [4].
Twenty lesions measured from 1 to 4.5 cm in length except one measuring 11 cm. The appearance of PF on the finger has been reported only twice before, only in adults [13,14]. One case of a toe lesion in a child has been reported [8].
Among the reviewed children’s clinical data, pain was present in 4/6 cases (66%) compared to 60% among adult patients [4]. The time interval between first appearance of the lesion and treatment is reported from 1.5 to “several months” in the reviews and from more than a month to five months in the reviewed clinical case reports. The interval time is about the same in adults but in one of the cases on a finger it was two years [14]. The vast majority of PF lesions concern the subcutaneous tissue, but in our case an intradermal involvement was observed, a finding reported only three times in literature and only once in a child, in a retroauricular location [6,14].
There are no reports of involution of the lesion in our retrieved paediatric cases, even though there are reports of involution in adults [15], and all lesions reported in literature were excised, even those with a prior positive PF diagnosis in biopsy. In literature accessible to us, every single reported and followed up paediatric case has been treated by excision. No study on PF involution has been undertaken, much less a comparative study between excision and expectant treatment, especially in children.
Conclusion
PF is a very rare disease in children exhibiting some similarities and some differences with its adult form. The cause of the disease remains unknown since a preceding trauma is rarely reported. The main concern is to differentiate it from RMS, a task that is more difficult in paediatric cases, which may present atypical histology. The present case, as well as other reviewed cases, indicate that pain, tenderness, aggressive development in a few weeks time and a size of less than 4.5 cm may be good differentiating signs in favour of PF.
Uptil now, no reports on expectant treatment in children have been published. A careful follow up of cases, with definite and unequivocal histological diagnosis of PF is needed, in order to propose evidence-based guidelines on treatment strategies, other than excision.
(M/F: Male/Female, y: year, mo: month, hn: head and neck, ue: upper extremities, le: lower extremities, ch: chest wall)
[1]. Meis JM, Enzinger FM, Proliferative fasciitis and myositis of childhoodAm J Surg Pathol 1992 16(4):364-72. [Google Scholar]
[2]. Goldblum JR, Folpe AL, Weiss SW, Enzinger and Weiss’s Soft Tissue Tumours 2014 6th edPhiladelphiaElsevierBenign Fibroblastic/Myofibroblastic Proliferations, Including Superficial Fibromatoses 204 Pp [Google Scholar]
[3]. Forcucci JA, Bruner ET, Smith MT, Benign soft tissue lesions that may mimic malignancySemin Diagn Pathol 2016 33(1):50-59. [Google Scholar]
[4]. Honda Y, Oh-i T, Koga M, Serizawa H, A case of proliferative fasciitis in the abdominal regionJ Dermatol 2001 28(12):753-58. [Google Scholar]
[5]. Lorenc ZP, Brourman S, Imbriglia JE, Proliferative fasciitis of the hand in a childJ Hand Surg Am 1987 12(6):1066-70. [Google Scholar]
[6]. Magro G, Michal M, Alaggio R, D’Amore E, Intradermal proliferative fasciitis in childhood: a potential diagnostic pitfallJ Cutan Pathol 2011 38(1):59-62. [Google Scholar]
[7]. Ghadially FN, Thomas MJ, Jabi M, Rippstein P, Intracisternal collagen fibrils in proliferative fasciitis and myositis of childhoodUltrastruct Pathol 1993 17(2):161-68. [Google Scholar]
[8]. Rosa G, Billings SD, A report of three cases of paediatric proliferative fasciitisJ Cutan Pathol 2014 41(9):720-23. [Google Scholar]
[9]. Lorette G, Treffandier O, Arbeille B, Vaillant L, Grangeponte MC, [Proliferative fasciitis in a 6-year-old child] Fasciite proliférative chez une enfant de six ansAnn Dermatol Venereol 1989 116(11):809-11. [Google Scholar]
[10]. Yamaga K, Shomori K, Yamashita H, Endo K, Takeda C, Minamizaki T, Proliferative fasciitis mimicking a sarcoma in a child: A case reportJ Dermatol 2014 41(2):163-67. [Google Scholar]
[11]. Bautista MJ, Perumal B, Jones DM, Meyer DR, Proliferative Fasciitis of the OrbitOphthal Plast Reconstr Surg 2015 DOI: 10.1097/IOP.0000000000000532 [Google Scholar]
[12]. Womer RB, Barr FG, Linardic CM, Rhabdomyosarcoma 2015 8th edElsevierNathan and Oski’s Hematology and Oncology of Infancy and Childhood. 1927. Pp [Google Scholar]
[13]. Richards RH, Evans G, Fitzgerald JA, Millward-Sadler GH, Proliferative fasciitis of a finger: a case reportJ Hand Surg Br 1990 15(4):501-02. [Google Scholar]
[14]. Satter EK, Dela Rosa KM, Intradermal proliferative fasciitis on the fingerAm J Dermatopathol 2015 37(3):246-48. [Google Scholar]
[15]. Kato K, Ehara S, Nishida J, Satoh T, Rapid involution of proliferative fasciitisSkeletal Radiol 2004 33(5):300-02. [Google Scholar]