A Rare Case of Unilateral Acute Idiopathic Maculopathy in Young Male
Atul Kumar Singh1, Vikas Sharma2
1 Assistant Professor, Department of Ophthalmolgy, Command Hospital, Old Air Port Road, Post-Agram, Bangalore, Karnataka, India.
2 Medical Officer, Department of Ophthalmolgy, Command Hospital, Old Air Port Road, Post-Agram, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Atul Kumar Singh, Assistant Professor, Department of Ophthalmolgy, Command Hospital, Old Air Port Road, Post-Agram, Bangalore, Karnataka-560007, India.
E-mail: draksingh78@gmail.com
Unilateral Acute Idiopathic Maculopathy (UAIM) is a rare disorder of Retinal Pigmentary Epithelium (RPE) that mainly affects the young healthy male. The variability of this disease can masquerade different entity, so diagnosis becomes cumbersome. We are reporting a case of young healthy male, who has reported to us with gross diminution of vision from right eye. Right eye examination showed a grayish yellow lesion with fluffy margins on the macula. Based on Optical Coherence Tomography (OCT) and Fundus Fluorescein Angiography (FFA) findings, he was diagnosed as a case of UAIM. He was started on topical anti-inflammatory eye drops with subsequent improvement of his vision.
Optical Coherence Tomography, Retinal pigmentary epithelium, Steroid
Case Report
A 25-year-old male presented with gross diminution of vision in right eye of three days duration, sudden in onset and associated with headache while reading. There was no past history of any fever, rashes or any other prodromal symptoms. He had no history of such kind and he had not taken treatment of long duration or any another treatment from outside. Visual Acuity (VA) was 6/36 in Right Eye (RE) and 6/6 in Left Eye (LE).
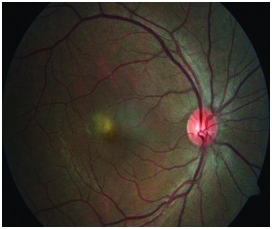
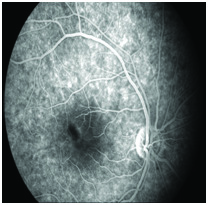
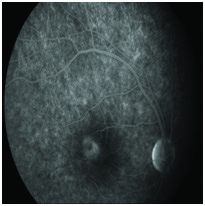
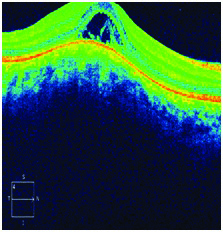
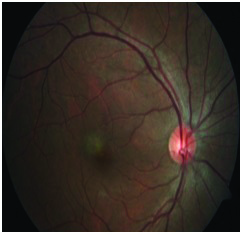
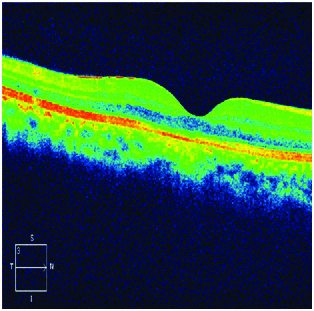
His Near Vision Acuity (NVA) was N/18 and N/6 respectively. Slit- lamp biomicroscopy examination showed normal anterior segment. The Amsler test chart showed central scotoma in his Right Eye. Fundus examination of RE revealed a grayish yellow lesion with fluffy margins 1/2 - 2/3 disc diameter in size at the level of the RPE affecting the fovea. There were no cells in the vitreous [Table/Fig-1]. The FFA showed a foveal hypofluorescent lesion in the early and mid-phases becoming hyperfluorescent in the late phase [Table/Fig-2,3]. OCT revealed spongy swelling in the outer layers of the retina with subretinal fluid [Table/Fig-4]. OCT retinal thickness was 340 microns.
Fundus examination of right eye showing a grayish yellow lesion with fluffy margins.
The FFA showing a foveal hypofluorescent lesion in the early phase.
The FFA showing a foveal hypofluorescent lesion in the late phase.
OCT image showing spongy swelling in the outer layers of the retina and the presence of subretinal fluid.
In view of the loss of VA, typical OCT and FFA findings in foveal location a presumptive diagnosis of solitary inflammatory lesion was made and the patient was started on topical anti-inflammatory eye drops three times/day. Seven days after initiation of therapy, VA in the RE had improved to 6/6 (P). Fundus examination revealed decrease in size of swelling and margins of lesion became well defined [Table/Fig-5]. OCT showed a reduction in retinal thickness (231 microns) with very minimal sub retinal fluid on thickness scan [Table/Fig-6].
Seven days post-therapy fundus examination showing a decrease in size of swelling with well-defined margins.
Seven days post-therapy OCT showing a reduction in retinal thickness with minimal sub retinal fluid.
Discussion
The initial description of UAIM was first described by Yannuzzi LA et al., in 1991 [1]. Since then very few cases have been described in literature. Yannuzi et al., reported on nine young patients with unilateral profound visual loss, serous detachment of macula and all patients had central scotoma on Amsler chart. The same group and others expanded the clinical spectrum of the disease adding the presence of papillitis and bilaterality. The natural course of UAIM varies and recovery period can be over a period of several weeks to months [2]. There are reports pointing to a viral aetiology and mode of transmission is thought to be a direct infection or through vascular route [3,4]. David et al., reported Hand, foot, and mouth disease as presenting syndrome for UAIM with Coxsackie virus A16 is an infectious entity [5].
Some studies suggests role of systemic steroids in the dosage of 1 mg/kg/day over weeks, which has shown a good visual recovery within a week time period [6]. OCT finding in UAIM is very well established [7,8] and now-a-days it is used as a diagnostic tool to diagnose as reported by others. Presence of subretinal fluid is typical finding in OCT. Our patient had a similar lesion that was reported by Yannuzzi et al., but lacking the prodromal illness. OCT retinal thickness overlying the lesion at presentation in this case was 340 microns, coming down to 231 microns after 1 week as the inflammation subsided. These could be because of hyper-reflective material which has been reabsorbed or the RPE edema had settled.
The poor VA of our patient was due to serous macular detachment involving macula. FFA finding in this case is a hypofluorescent lesion in the early phases, that became hyperfluorescent in the late recirculation times [Table/Fig-2,3]. We had assumed that the hypofluorescence as the result of oedema and the late hyperfluorescence as a result of both staining at the level of RPE and pooling of fluorescein in sub retinal space due to the breakdown of the outer blood–retinal barrier.
Conclusion
We have presented a rare case of UAIM which has shown good response to topical NSAIDs. In UAIM, a course of topical NSAIDs could hasten the resolution of inflammation and recovery of retinal anatomy. OCT seem better clinical tools to characterize and follow up the evolution of the disease.
[1]. Yannuzzi LA, Jampol LM, Rabb MF, Sorenson JA, Beyrer C, Wilcox LM Jr, Unilateral acute idiopathic maculopathyArch Ophthalmol 1991 109:1411-16. [Google Scholar]
[2]. Freund KB, Yannuzzi LA, Barile GR, Spaide RF, Milewski SA, Guyer DR, The expanding clinical spectrum of unilateral acute idiopathic maculopathyArch Ophthalmol 1996 114:555-59. [Google Scholar]
[3]. Beck AP, Jampol LM, Glaser DA, Pollack JS, Is coxsackievirus the cause of unilateral acute idiopathic maculopathy?Arch Ophthalmol 2004 122:121-23. [Google Scholar]
[4]. Agrawal R, Bhan K, Balaggan K, Lee RW, Pavesio CE, Addison PK, Unilateral acute maculopathy associated with adult onset hand, foot and mouth disease: Case report and review of literatureJ Ophthalmic Inflamm Infect 2015 5:2 [Google Scholar]
[5]. David MC, John WB, Jeffray DB, A rare presentation of unilateral acute idiopathic maculopathyRetinal Physician 2016 13(7):56-60. [Google Scholar]
[6]. Miguel A, Cuadrado R, Unilateral acute idiopathic maculopathy: Angiography, optical coherence tomography and microperimetry findingsOphthalmic Inflamm Infect 2011 1(3):125-27. [Google Scholar]
[7]. Aggio FB, Farah ME, Meirelles RL, Souza EC, STRATUSOCT and multifocal ERG in unilateral acute idiopathic maculopathyGraefes Arch Clin Exp Ophthalmol 2006 244:510-16. [Google Scholar]
[8]. Andonegui J, Maya JR, Zurutuza A, de Arcelus MP, Optical Coherence Tomography Findings in a Case of Unilateral Acute Idiopathic MaculopathyOpen Journal of Ophthalmology 2012 2:119-21. [Google Scholar]