Urinary Tract Infections (UTIs) are one of the most common infections for which patient seek attention from healthcare personnel for both therapeutic and diagnostic purposes. E.coli is the most common etiological agent for the UTIs. Fluoroquinolones and cephalosporins and other β-lactams have been the most commonly prescribed antibiotics for treating these infections [1,2]. With the emergence of resistance to these drugs, antibiotics like fosfomycin and Nitrofurantoin are gaining importance. Fosfomycin, the phosphonic antibiotic was discovered in Spain in 1969. It is available both orally as well as systemically. Fosfomycin trometamol and fosfomycin calcium are the oral forms of the drug whereas, fosfomycin disodium is used intravenously. It is a broad spectrum anti-microbial agent with activity against various gram-positive and gram-negative bacterial isolates which includes staphylococci, enterococci, E.coli and other gram-negative bacteria [3,4]. It is a bactericidal antibiotic which intereferes with cell wall synthesis by inhibiting phosphoenolpyruvate transferase which is the first enzyme involved in the peptidoglycan synthesis [3]. There is no cross resistance of this antibiotic with others and it can be administered safely in combination with many other antibiotics [3,4].
Fosfomycin is rapidly absorbed orally with a bio-availability of 40% and majority of the drug is excreted unchanged in urine with very high concentration levels achieved in urine after a single oral dose [3]. Fosfomycin has a renal elimination of 95% and no tubular secretion occurs [4]. It has a relatively long elimination half-life, which varies between 4 and 8 hour [4]. Urine levels remain high for prolonged period which makes it a suitable drug in the treatment of UTI. Fosfomycin has good distribution into tissues, achieving clinically relevant concentrations in serum, kidneys, bladder wall, prostate, lungs, inflamed tissues, and other body fluids [3–6].
Materials and Methods
This was a prospective study done in the Department of Microbiology SVS Medical College, Mahbubnagar from Jan 2016 to Mar 2016. The study was approved and ethical clearance was obtained by the Institutional Ethics Committee. A total of 564 urine samples were processed in the microbiology laboratory. All the samples obtained from clinically suspected UTI before taking any antibiotic were included. Only one sample per patient is included. Samples obtained from patients who are already on antibiotics and also repetitive samples from the same patients were excluded from the study.
Samples were processed according to the standard protocols and the isolated organisms were speciated by routine bio-chemical testing [9]. Out of 564 samples 375 were from female patients and 189 from males. A total of 170 E.coli were isolated from these samples and antibiotic sensitivity testing was done by Kirby-Bauer disc diffusion testing and interpretation was done according to the CLSI guidelines (M100-S23) [10]. As there are no CLSI guidelines for cefoperazone sulbactum, interpretive criteria used by Ghafur et al., were adopted [11]. The list of antibiotics used were amoxyclav (20/10 μg), gentamicin (10 μg), amikacin (30 μg), norfloxacin (10 μg), ofloxacin (5 μg), ciprofloxacin (5 μg), levofloxacin (5 μg), nitrofurantoin (300 μg), co-trimoxazole (25 μg), doxycycline (30 μg), cefixime (5 μg), ceftriaxone (30 μg), cefaperazone/sulbactum (75/30 μg), piperacillin/tazobactum (100/10 μg), imipenem (10 μg), fosfomycin (200 μg), methenamine mandelate (3 mg) (Hi-Media, Mumbai). American Type Culture Collection (ATCC) E.coli 25922 was used as control strain. Statistical analysis was done by using chi-square test.
Results
Out of 564 urine samples processed a total of 170 E.coli were isolated and were tested for antibiotic susceptibility. Out of 170, males were 60 (35.30%) and females were 110 (64.70%) with male to female ratio of 1: 1.83 with predominance of female patients.
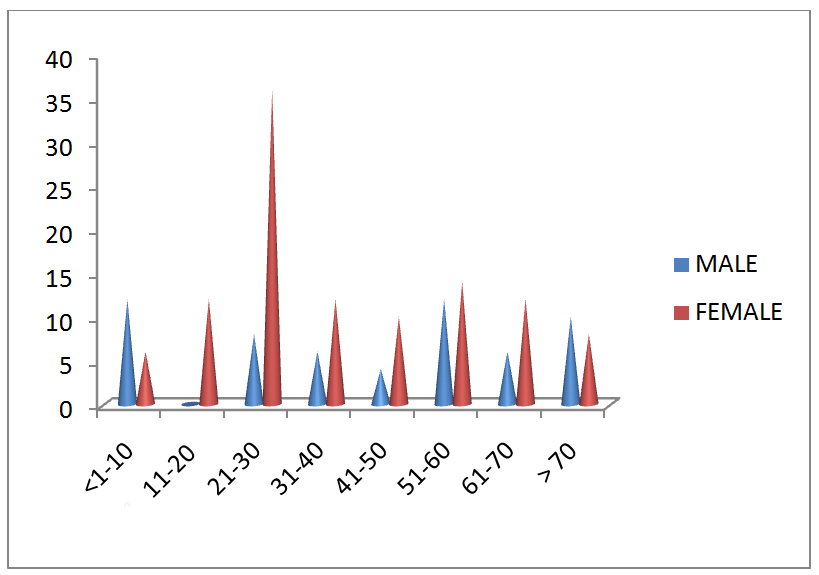
Majority of the isolates were obtained from the age group of 21-30 years accounting to 44 (25.8%) of the total isolates followed by 51-60 years accounting to 26 (15%). Female predominance was significantly seen in the age group of 21-30 years and 11-20 years. Male predominance over females was seen in the age groups of 1-10 years and >70 years [Table/Fig-1]. Female predominance was observed in inpatients (42.35% females vs 24.70% males) as well as outpatients (22.3% females vs 10.50% males). Among inpatients the predominant age group was >60 years with 48 (42.1%) out of 114 isolates belong to that age group followed by 40-60 years (28%) whereas, the least number of isolates from inpatients were in the age group of 20-40 years (12.2%). In contrast majority of the isolates from out patients were in the age group of 20-40 years (64.2%) followed by 40-60 years (17.8%). Only two isolates (3.5%) were from the age group above 60 years among outpatients.
Age wise distribution of patients (in years).
In the present study fosfomycin, imipenem and methenamine mandelate showed the highest sensitivity with all the isolates (100%) being susceptible to these drugs. Whereas, least sensitivity was observed for amoxyclav (15.2%) followed by cefixime (16.4%) and norfloxacin (21%). Other oral antibiotics like co-trimoxazole has shown activity in 45.8% of the isolates where as 82.3% of the isolates were sensitive to nitrofurantoin. More than 80% of the isolates were sensitive to amikacin, cefaperazone/sulbactum and piperacillin/tazobactum [Table/Fig-2].
antibiotic sensitivity pattern of inpatients and outpatients.
| Sr. No. | Antibiotics | In patient (n=114) | Out patient (n=56) | Total (n=170) |
|---|
| Sensitive | Percentage | Sensitive | Percentage | Sensitive (%) |
|---|
| 1 | Amoxyclav | 14 | 12% | 12 | 21% | 26 (15.2%) |
| 2 | Gentamycin | 46 | 40% | 28 | 50% | 74 (43.5%) |
| 3 | Amikacin | 96 | 84% | 42 | 75% | 138 (81%) |
| 4 | Norfloxacin | 24 | 21% | 12 | 21% | 36 (21%) |
| 5 | Ofloxacin | 26 | 23% | 14 | 25% | 40 (23.5%) |
| 6 | Ciprofloxacin | 30 | 26% | 16 | 28% | 46 (27%) |
| 7 | Levofloxacin | 26 | 23% | 16 | 28% | 42 (24.7%) |
| 8 | Nitrofurantoin | 96 | 84% | 44 | 78% | 140 (82.3%) |
| 9 | Co- trimoxazole | 48 | 42% | 30 | 53% | 78 (45.8%) |
| 10 | Doxycycline | 42 | 37% | 22 | 39% | 64 (37.6%) |
| 11 | Cefixime | 14 | 12% | 14 | 25% | 28 (16.4%) |
| 12 | Ceftriaxone | 24 | 21% | 20 | 36% | 44 (25.8%) |
| 13 | Cefoperazone/ sulbactum | 90 | 79% | 50 | 89% | 140 (82.3%) |
| 14 | Piperacillin/ Tazobactum | 92 | 81% | 46 | 82% | 138 (81.1%) |
| 15 | Methenamine mandelate | 114 | 100% | 56 | 100% | 170 (100%) |
| 16 | Imipenem | 114 | 100% | 56 | 100% | 170 (100%) |
| 17 | Fosfomycin | 114 | 100% | 56 | 100% | 170 (100%) |
Fosfomycin was highly active against all the isolates of E.coli including the hospital acquired UTI strains of E.coli. No statistical difference was observed between the inpatient and outpatient strains with regards to fosfomycin activity by using chi-square test, as all the isolates were uniformly sensitive to it. But the same when applied to other antibiotics like nitrofurantoin, co-trimoxazole and ciprofloxacin in comparison to fosfomycin, statistically significant difference (p<0.001) was observed both for inpatients and out patients.
Discussion
In the olden days simple antibiotic like penicillin was highly effective against many bacterial isolates. Now-a-days even the high end antibiotics like carbapenems and colistin are also not active against many pathogenic bacteria because of the development of multidrug resistance [7]. E.coli being the most common organism in the causation of UTIs, is also an important pathogen which shows multiple drug resistance by various mechanisms like Extended Spectrum Beta Lactamases (ESBL) production etc., [7,8]. In view of these resistant pathogenic bacteria where cross-resistance is common to multiple antibiotics either newer and high potent antibiotics should be discovered or the old and unused antibiotics should be revived.
In the present study, majority of the isolates were resistant to most of the antibiotics, with amoxyclav topping the list where only 15.2% of the total E.coli isolates were sensitive to this drug. Next to Amoxyclav, Fluoroquinolone are the most commonly used urinary antibiotics whose sensitivity ranged from 21% (norfloxacin) to 27% (ciprofloxacin). Among the third generation cephalosporins, cefixime has shown a sensitivity of only 16.4% where as ceftriaxone has shown a sensitivity of 25.8%. Similar findings were observed in other studies. In Niranjan B et al., study 26% of E.coli were susceptible to amoxyclav and only 25% isolates were susceptible to ciprofloxacin and 29% were susceptible to ceftriaxone [12].
In the present study majority of the isolates were resistant to third generation cephalosporins like cefixime (83% resistant) or fluoroquinolones like norfloxacin (79%) making them inappropriate choice for choosing as empirical therapy for the treatment of UTIs in our hospital.
Among the aminoglycosides, amikacin has shown very good sensitivity over gentamycin with 81% isolates being susceptible to amikacin whereas, only 43% were sensitive to gentamycin, making amikacin as preferred drug over gentamycin. In Niranjan B et al., study 82.6% of the isolates were sensitive to amikacin which is similar to our study [12].
In the preset study only 45.8% of the isolates are sensitive to co-trimoxazole and more than half of the isolates being resistant. In Simon A et al., study only 27% of the E.coli isolates were susceptible to Co-trimoxazole [13]. In Niranjan B et al., study 35.8% were susceptible and in Biswas D et al., study 59.7% of the E.coli isolates were susceptible to co-trimoxazole which are similar to our study results [12,14].
Combination drugs of beta lactams with beta-lactamase inhibitors like piperacillin/tazobactum and cefaperazone/sulbactum are increasingly being used now-a-days in health care set-up especially when nosocomial infections are suspected [15,16]. In the present study 82.3% of isolates were susceptible to cefaperazone/sulbactum and 81% to piperacillin/tazobactum.
Oral antibiotic nitrofurantoin has also shown very good activity against majority of the E.coli with 82.3% isolates being susceptible to it. In a study conducted by Simon A et al., 94% of the E.coli was susceptible to nitrofurantoin [13]. Similarly in Lai B et al., study 89% of the E.coli isolates was susceptible to nitrofurantoin [17]. Nitrofurantoin, an age old antibiotic has been forgotten with the availability of more user friendly cephalosporins and fluoroquinolone group of drugs. With the advent of multidrug resistance this antibiotic has gained importance once again. Availability in oral form and attaining high levels in the urine and less resistance makes this drug a preferred drug over the others [18,19].
The present study also included methenamine mandelate in the drug susceptibility panel. Methenamine is an age old drug and is a classic example of forgotten drug. It is a urinary antiseptic agent acts by unique mechanism of formation of formaldehyde in the acidic urine and is used especially in recurrent UTIs. It is available in two forms methenamine hippurate and methenamine mandelate. Methenamine mandelate is available for oral use as film-coated tablets and is used for adults in the dosage of 1 gm four times a day. When used as recommended, this drug is especially suitable for long-term therapy and no resistance to formaldehyde develops because of which the pathogens resistant to other anti-bacterial agents may respond to this drug [20]. Though there are no CLSI guidelines for the disc diffusion testing of this drug, in the preset study we tried to evaluate the in-vitro susceptibility testing following the manufacturer guidelines (SD068- Himedia, India) and using the control strain ATCC E.coli 25922.
In our study, all the isolates were uniformly sensitive to imipenem, and fosfomycin (100%). As no isolate has shown resistance to these antibiotics they can be considered effective for the treatment purpose. Out of these, fosfomycin is the only drug which is cheap, available in the oral formulation, can be used as single dose (3g sachet costing Rs 400 approx.) and also reaches high concentration in the urine [3,4]. Hence, this drug can be preferred and can be used effectively especially in resource poor settings. Similar results were found in different studies conducted all over the world. In ARESC (Antimicrobial Resistance Epidemiological Survey on Cystisis) study group 98.1% of the E.coli isolated from urine samples was susceptible to fosfomycin [21]. In a huge study conducted by Falgas ME et al., 1604(96.8%) of the 1657 ESBL producing E.coli isolates were susceptible to fosfomycin [22]. Apart from in-vitro studies, clinical studies conducted on patients has also shown effective results with regards to fosfomycin. In Pullukcu H et al., study 94.3% of clinical success was noted in the treatment of ESBL producing E.coli related lower UTI [23]. Also, fosfomycin has also shown to have immunomodulatory effects by various researchers [24].
Limitation
The study was a short study with limited number of isolates and only E.coli were included and also emphasis on ESBL detection was not given in these isolates which is an important aspect to consider in nosocomial infections.
Conclusion
There has been an increase in the drug resistance of E.coli isolates to commonly used antibiotics like fluoroquinolones, cephalosporins and other β-lactams which was observed in the present study. Inappropriate use of antibiotics has always been a threat for the emergence of multidrug resistant pathogens. As the antibiotic pipeline is empty with only few alternative drugs available for these resistant pathogens, testing for old and forgotten antibiotics like fosfomycin is recommended. Because of its unique mechanism of action and low incidence of resistance and availability in oral form and single dose administration it can be a potential therapeutic alternative over many other antibiotics in the treatment of UTIs. At the same time it should be remembered that inadvertent use of fosfomycin may also lead to the development of resistance to this drug. It is always necessary to know the surveillance patterns in a particular health care setup and use the drugs appropriately, which will not only prevent the emergence and spread of drug resistance but also helps in preserving the few leftover antibiotics for future use.