Community Acquired Burkholderia cepacia Bacteraemia Presenting as MODS in an Immunocompetent Individual: An Unusual Case
Ritesh Ranjan1, Priti Chowdhary2, Aman Kamra3
1 Assistant Professor, Department of Surgery, Subharti Medical College, Meerut, Uttar Pradesh, India.
2 Resident, Department of Microbiology, Subharti Medical College, Meerut, Uttar Pradesh, India.
3 Resident, Department of Surgery, Subharti Medical College, Meerut, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Priti Chowdhary, Flat No. Y-11, Narayan Guru Bhawan, Subharti University, NH 58, Meerut-250005, Uttar Pradesh, India.
E-mail: prettypritiever@yahoo.com
Burkholderia cepacia has been recognized as a group of highly virulent organisms known as Burkholderia cepacia complex (Bcc). Bcc are ubiquitous in nature and most commonly found in moist environment, on plant roots and soil. Because of its high intrinsic antibiotic resistance, Bcc is a major cause of morbidity and mortality in hospitalized patients. It is reported most commonly in immunocompromised patients especially in patients with cystic fibrosis. Here, we report a rare case report of bacteraemia by Burkholderia cepacia in an immunocompetent male, who presented with fever and Multiple Organ Dysfunction Syndrome (MODS). Burkholderia cepacia was isolated from his blood culture, which he acquired from his work place. He was treated successfully and discharged after negative blood culture.
Ciprofloxacin, Cystic fibrosis, MicroScan
Case Report
A 21-year-old male, who was a cook in a fast food shop, was brought to the outpatient clinic of our hospital in July 2014 with complaint of high temperatures with chills and rigor. He also complained of, on and off diffuse abdominal pain, which was pricking type, moderate to severe in intensity and non-radiating in nature. The abdominal pain was associated with vomiting which was non-projectile in nature and contained food particle. The patient complained of yellow discolouration of skin and sclera. There was no history of any pre-morbid illness or Cystic Fibrosis (CF). The patient also gave history that his younger brother, who was his co-worker, was also suffering from similar symptoms and was under treatment in some other hospital.
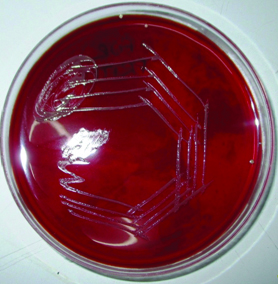
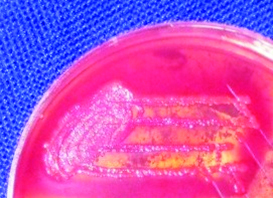
General examination of the patient revealed that the patient was febrile and icteric. His pulse rate at the time of admission was 110 beats per minute. Blood pressure was 68/50 mmHg. Respiratory rate was 18 breaths per minute. His blood investigations showed haemoglobin 8.5 gram %. His Total Leukocyte Count (TLC) was 39,100/mm3 with neutrophil count 86%, lymphocyte count 11% and eosinophil count 3%. Blood urea level was 191.9 mg/dl and serum creatinine was 4.2 mg/dl. Other investigations showed deranged liver function tests as total bilirubin was 12.1 mg/dl with direct bilirubin 9.4 mg/dl and indirect bilirubin 2.7 mg/dl. Level of Alanine Aminotransferase (ALT) was 57 IU/l, Aspartate Aminotransferase (AST) was 43.0 IU/ l and Alkaline Phosphatase (ALP) level was 87.0 IU/ l. Total protein was 4.2 g/dl with albumin 1.7 g/dl and globulin 2.5 g/dl. Serum electrolytes were within normal range. The patient was negative for Hepatitis C, Hepatitis B and HIV. Microbiological tests for malaria and typhoid were also negative. Ultrasonography showed, mild liver enlargement. Plain chest X-ray was non specific. Two sets of blood samples were cultured on blood agar and MacConkey agar. Both samples yielded black colour colony on blood agar and purple coloured pigmented colony on MacConkey agar plate [Table/Fig-1,2]. The isolate was catalase positive, lactose non-fermenting, gram-negative, motile bacteria. Triple sugar iron agar showed alkaline slant with no change in butt. The isolate was identified phenotypically as Burkholderia cepacia complex. Antibiotic susceptibility by Kirby-Bauer method was done. The isolate was susceptible to ciprofloxacin, levofloxacin, imipenem and meropenem. Identification was further confirmed by MicroScan commercial test (Siemens). Minimal Inabitory Constration (MIC) detection by MicroScan was also done [Table/Fig-3].
Growth of Burkholderia cepacia on blood agar.
Growth of Burkholderia cepacia on MacConkey agar.
MIC detection by MicroScan (Siemens).
| Drug | MIC (Microgram/ml) | Drug | MIC (Microgram/ml) | Drug | MIC (Microgram/ml) | Drug | MIC (Microgram/ml) |
|---|
| Amikacin | 32 | Fosfomycin | >32 | Cefoxitin | >8 | Nitrofurantoin | >64 |
| Amoxycillin/Potassium clavulanate | >16/8 | Gentamycin | >8 | Ceftazidime | >16 | Norfloxacin | ≤4 |
| Ampicillin | >16 | Imipenem | >8 | Ceftazidime/ Potassium clavulanate | >2 | Piperacillin/Tazobactam | 64 |
| Cefazolin | >16 | Levofloxacin | ≤2 | Cefuroxime | >16 | Piperacillin | >64 |
| Cefepime | >16 | Meropenem | 4 | Ciprofloxacin | 2 | Tetracycline | >8 |
| Cefotaxime | >32 | Mezlocillin | >64 | Colistin | >4 | Tobramycin | >8 |
| Cefotaxime/ Potassium clavulanate | >4 | Moxifloxacin | ≤0.5 | Ertapenem | >4 | Trimethoprim/Sulphamethoxazole | ≤2/38 |
| | | | | | Trimethoprim | ≤8 |
The patient was treated with broad spectrum injectable cephalosporin, cefepime and clindamycin initially as empirical therapy. It was changed to ciprofloxacin after sensitivity results were available. Intravenous fluids and inotropic agent dopamine was given to correct low blood pressure. Vitamin K and ursodeoxycholic acid were given to correct deranged liver function tests. Nutritional supplements and probiotics were also given. The patient recovered within 15 days. A second blood culture was done which was negative. The patient was discharged in satisfactory condition.
Discussion
Burkholderia cepacia are complex organisms which are present everywhere. They are found most commonly on plant roots, soil and moist environment. An American microbiologist, William Burkholder, first described it as the causative agent of bacterial rot of onion bulbs [1]. Bcc consists of Burkholderia cepacia and related bacteria. They constitute a group of highly virulent organisms. Burkholderia cepacia complex is a group of phenotypically similar but genetically distinct bacteria. All bacteria of this group are motile, gram-negative aerobic bacilli with multi-trichous polar flagella. They are found both in soil and water. Bcc is intrinsically resistant to many commonly used antibiotics, such as, antipseudomonal penicillins (piperacillin, ticarcillin and carbenicillin), aminoglycosides, first and second generations of cephalosporins and polymixins [1]. All these antibiotics are commonly used in Pseudomonas infections and so the proper identification of Bcc from Pseudomonas is important. Mechanisms conferring resistance include efflux pumps, production of b-lactamases and other modifying enzymes, as well as modification of antibiotic targets [2].
Some Bcc bacteria have useful commercial properties such as breakdown of pollutants or increased crop yield [1]. The organism can also cause prolonged temperatures and a terminal disease ("Cepacia syndrome") [3]. Pathogenesis is described by identification of the flagellin glycosylation system in Burkholderia cenocepacia and the contribution of glycosylated flagellin to evasion of human innate immune responses. Flagella are required for biofilm formation, as well as adhesion to and invasion of epithelial cells. Recognition of flagellin via the Toll-Like Receptor 5 (TLR5) contributes to exacerbate lung epithelial inflammatory responses [4]. Burkholderia cepacia infection is rarely reported in immunocompetant hosts. Mostly it has been reported in patients of cystic fibrosis. These bacteria frequently cause fatal infections in vulnerable humans, such as those who have CF. All initial isolates of Bcc were from patients of CF [5]. Burkholderia cepacia has now been recognized as causing fatal disease in healthy individuals [6,7]. Matthaiou DK et al., has reported a case of bacteraemia due to Burkholderia cepacia in a patient without CF suffering from Chronic Obstructive Pulmonary Disease (COPD) [8]. Bressler AM et al., has reported a case series of ICU patients with Burkholderia cepacia complex bacteraemia in patients without CF [9]. Karanth SS et al., have also reported a case of community acquired Burkholderia cepacia infection presenting as pyopneumothorax in an immunocompetent individual [10]. Bayram M et al., has also reported two cases of community acquired pneumonia in immunocompetent individuals [11]. Our patient was also immunocompetent and there were no predisposing factors. As our patient was a cook in a fast food joint and also the fact that his co-worker and brother was also suffering from same symptoms, we speculated any source of infection at work or home such as rotten onions. Most probable route of infection was oral ingestion as the patient had abdominal pain and vomiting. Any one of them might have contracted the infection first and then transmitted to other or it might be simultaneous infection from a common source. One difference between our case and all these reported cases is that our patient had no lung complains.
Conclusion
We conclude that correct identification of Burkholderia cepacia should be done for proper administration of treatment as they are intrinsically resistant to many antibiotics. Burkholderia cepacia should be correctly differentiated from Pseudomonas aeruginosa as course of illness is unlike any clinical situation seen with Pseudomonas aeruginosa. Burkholderia cepacia can cause infection in immunocompetent individuals also and it can present without pneumonia or chest complains as MODS.
[1]. Gautam V, Singhal L, Ray P, Burkholderia cepacia complex: Beyond Pseudomonas and AcinetobacterIndian J Med Microbiol 2011 29(1):4-12. [Google Scholar]
[2]. Guglierame P, Pasca MR, De Rossi E, Buroni S, Arrigo P, Manina G, Efflux pump genes of the resistance-nodulation-division family in Burkholderia cenocepacia genomeBMC Microbiol 2006 6:66 [Google Scholar]
[3]. Jones AM, Dodd ME, Webb AK, Burkholderia cepacia: Current clinical issues’, environmental controversies and ethical dilemmasEur Respir J 2001 17(2):295-301. [Google Scholar]
[4]. Hanuszkiewicz A, Pittock P, Humphries F, Moll H, Rosales AR, Molinaro A, Identification of the flagellin glycosylation system in Burkholderia cenocepacia and the contribution of glycosylated flagellin to evasion of human innate immune responsesJ Biol Chem 2014 4;289(27):19231-44. [Google Scholar]
[5]. Mahenthiralingam E, Urban TA, Goldberg JB, The multifarious, multireplicon Burkholderia cepacia complexNat Rev Microbiol 2005 3:144-56. [Google Scholar]
[6]. Wong S, Tam AY, Yung RW, Kwan EY, Tsoi NN, Pseudomonas septicaemia in apparently healthy childrenActa Paediatr Scan 1991 80:515-20. [Google Scholar]
[7]. Hobson R, Gould I, Govan J, Burkholderia (Pseudomonas) cepacia as a cause of brain abcess secondary to chronic suppurative otitis externaEur J Clin Microbiol Infec Dis 1995 41:908-11. [Google Scholar]
[8]. Matthaiou DK, Chasoub E, Atmatzidisb S, Tsolkasa P, A case of bacteraemia due to Burkholderia cepacia in a patient without cystic fibrosisRespiratory Medicine CME 2011 4(3):144-45. [Google Scholar]
[9]. Bressler AM, Kaye KS, LiPuma JJ, Alexander BD, Moore CM, Reller LB, Risk factors for Burkholderia cepacia complex bacteraemia among intensive care unit patients without cystic fibrosis: a case-control studyInfect Control Hosp Epidemiol 2007 28:951-58. [Google Scholar]
[10]. Karanth SS, Regunath H, Chawla K, Prabhu M, A rare case of community acquired Burkholderia cepacia infection presenting as pyopneumothorax in an immunocompetent individualAsian Pac J Trop Biomed 2012 2(2):166-68. [Google Scholar]
[11]. Bayram M, Babalik M, Bakan ND, Döngel I, Community-acquired Burkholderia cepacia pneumonia: a report of two immunocompetent patientsTuberk Toraks 2011 59(4):380-83. [Google Scholar]