Introduction
Pelvic Inflammatory Disease (PID) is a common and serious complication of sexually transmitted diseases in young women but is rarely diagnosed in the postmenopausal women. Very few studies have been done regarding post-menopausal PID.
Aim
To determine the burden of PID, associated micro-organisms, pathophysiology and risk factors among post-menopausal women of the community.
Materials and Methods
A cross-sectional study was conducted among 530 post-menopausal women in the registered field practice areas of the JN Medical College and Hospital, Aligarh, Uttar Pradesh, India. A pre designed and pre tested proforma was used to obtain data regarding socio-demographic details and factors associated with PID. Clinical and laboratory examinations were done to confirm the diagnosis of PID. Data was analyzed using SPSS 23.0. Association between categorical variables was tested with chi-square test and logistic regression analysis was used to find independent risk factors. The value of p<0.05 was considered as significant.
Results
About 11.55% of the study subjects were diagnosed with PID (12.5% in rural areas and 10.6% in urban areas). Bacterial vaginosis followed by Trichomonas vaginalis were most common. Among the important risk factors, significant association was found with occupation of the women, increasing parity, multiple sexual contacts, and associated pelvic organ prolapse. Association with smoking, chronic illnesses, diabetes mellitus and hypertension, and associated urinary tract infection were not found to be significant.
Conclusion
The study shows the hidden burden of the disease in the community and the associated risk factors, which can be prevented by life style and cultural changes if incorporated earlier in the lives.
Cervico-vaginal flora, Gynaecological morbidity, Postmenopausal women
Introduction
PID is an infection of upper female genital tract, including uterus, fallopian tubes and ovaries, which may spread to contiguous pelvic structures and present with pain, abnormal or excessive discharge, lower backache, lower abdominal ache, associated fever, vulval itching and burning [1–3]. PID affects predominately in the reproductive age years with its highest prevalence being in the second and third decades [4]. It is an important public health problem in all women but seldom identified in the postmenopausal females [5–8]. Although it is a rare entity in the postmenopausal woman, early recognition of the diagnosis and appropriate therapy can decrease the considerable morbidity and mortality it can cause otherwise.
Risk factors associated with PID include young age at first intercourse, high frequency of intercourse, number of sexual partners, promiscuous partner. It is rare in postmenopausal women and in those who had tubal ligation [9]. Women suffering from this infection are at higher risk of chronic pelvic pain, ectopic pregnancy, infertility and unexpected hospital visits [10,11].
A definitive diagnosis of PID is done by laparoscopic visualization of inflamed, purulent fallopian tubes; PID is generally a clinical diagnosis and thus represents a diagnostic challenge [12]. The pathophysiology involves the cervical factors such as everted columnar epithelium of the endo-cervix, smaller cervical transformation zone, and tenacious cervical mucus in post menopausal women which lower the susceptibility to infections. But, instrumentation, vaginal douching, barrier contraceptives increase the risk [9–12].
In older women, direct spread is more likely to be associated with PID. Diverticulitis, Crohn’s disease, colonic cancers, appendicitis, fistula formation from an abscess cavity to the genital tract has been associated with a direct spread of infection to the ovaries, oviducts, and uterus [13–15]. Although many studies have been done which describe the course of this disease in reproductive age females, not many studies are done on the post menopausal women in the community.
Largely, the exact prevalence of PID in postmenopausal women in India is unknown. Therefore, the aim of this study was to determine the burden of PID, associated micro-organisms, pathophysiology and risk factors among post menopausal women.
Materials and Methods
It was a community based cross-sectional study. All the households registered under Urban Health and Training Centre (UHTC) and Rural Health and Training Centre (RHTC), Department of Community Medicine, JN Medical College, Aligarh, Uttar Pradesh, India was taken under the sampling frame. The study period was one year i.e., from June 2012 to May 2013. All postmenopausal women who had completed at least one year of menstruation free period were included. Women who did not give consent, those who had not attained menopause, those who were receiving hormone replacement therapy and those who were suffering from severe, debilitating illness were excluded [16,17].
Systematic random sampling and proportionate to Population Size Method (PPS) were used. The distribution of sample with respect to the areas has been shown in [Table/Fig-1]. The sample size was taken according to the study conducted by Puri S et al., in the urban and slum areas of Chandigarh, Punjab, India, where out of 71.4% of the total females who had attained menopause at the time of study, 42.7% had vaginal irritation/discharge, which was used for calculating the sample size for this study [18]. The total sample size was calculated according to the formula;
Distribution of study subjects according to the area.
| Name of area | Registered households | Sample size | Sampling interval |
|---|
| Rural Areas |
| Jawan | 926 | 105 | 9 |
| Sumera | 594 | 67 | 9 |
| Tejpur | 267 | 28 | 9 |
| Chotajawan | 266 | 29 | 9 |
| G.bhojpur | 185 | 17 | 10 |
| Jawansikandarpur | 137 | 14 | 10 |
| Sumerajhal | 47 | 5 | 10 |
| Total | 2422 | 265 | |
| Urban Areas |
| Firdousnagar | 764 | 118 | 6 |
| Naglaquila | 578 | 85 | 6 |
| Shahanshahbad | 286 | 44 | 7 |
| Patwarikanagla | 125 | 18 | 7 |
| Total | 1753 | 265 | |
| Total sample size=530 |
N = z2pq/L2
where z=1.96, p stands for prevalence (42.7%), q = 100- p, L = relative error = 15% of p, the corrected sample size was 262.
Considering design effect and taking equal sample size from rural as well as urban areas, a total of 530 postmenopausal women were approached. Informed and written consent was taken. The study tool comprised of pre tested and pre structured proforma with information about personal details including the name, age, address, marital status, religion, occupation, educational status, total family income, type of family, place of residence, locality etc., and detailed history of uro gynaecological complains, if present. The locality of the area was assessed as congested by the number of houses in the given area and presence of other houses on all three sides [9]. If there were any complains suggestive of PID, patients were taken for gynaecological examination at the respective centres. Abdominal examination and local gynaecological examinations were done. The cervical discharge was collected by three different techniques for pathological and microbiological investigations.
With the first technique, cotton swab was introduced for collection of discharge on two slides for wet mount smear method (for isolation of protozoa) and 10% Potassium Hydroxide (KOH) application test (for isolation of Candida and for Whiff’s test).
With the second technique, a cervical swab culture stick was introduced for culture and sensitivity and for gram staining. With the third technique, an Ayre’s spatula was introduced for making a Papanicolaou (Pap) smear slide.
The presence of PID was confirmed by microscopic and histopathology Pap examinations. Bacterial vaginosis is a poly microbial disorder characterized by an increase in the vaginal pH over 4.5, a reduction in or absence of colonization of lactobacilli on the vaginal mucosa and overgrowth of several facultative and obligate anaerobic bacteria. Its diagnosis was made by the presence of a minimum of 20% of “clue” cells in the squamous cell population on microscopic examination of a saline suspension of vaginal discharge, associated with two of the following three findings [18]:
Anterior fornix vaginal pH equal or greater than 4.7.
Release of a fishy odour on addition of 10% KOH to the vaginal discharge (positive “whiff test”).
Presence of an increased thin homogenous white vaginal discharge.
The Pap smear slide was sent to the department of pathology after fixing in 10% formaldehyde. The cervical swab culture was sent to the department of microbiology in standard culture bottles for Gram staining, culture and sensitivity. Wet mount smear method was used for isolation of Trichomonas vaginalis. 10% KOH application was used for isolation of Candida with the help of microscope. Whiff’s test was used for detecting Gardenella vaginalis, confirmed by the presence of clue cells on wet mount examination, confirmed by the presence of clue cells on wet mount examination. These were done in the respective labs of UHTC and RHTC. Various parameters of relevance along with socio-demographic profile of patients were studied and correlated with the above findings. The diagnosis of urinary tract infection was confirmed by microscopic examination of urine. The diagnosis of pelvic organ prolapse was made by clinical examination by a trained gynaecologist at the respective centres.
Statistical Analysis
Data was analyzed using the SPSS version 23.0. Standard error of difference between the two proportions, chi-square test and logistic regression analysis was applied wherever applicable. The value of p<0.05 was considered as significant for this study.
Ethical considerations: Informed written consent was taken from each subject before interview. Health education and counselling regarding the risk factors for development of different problems were provided to all the respondents. Permission from the Institutional Ethics Committee, Faculty of Medicine, AMU, Aligarh, Uttar Pradesh, India, was taken. Management or referral of the patients was done at the respective centres wherever needed as per requirement.
Results
The mean age of the study population was 58.14±8.45 years. Median age was 57.0 years and mode was 50.0 years. Out of the 530 post menopausal women, 385 were having a gynaecological or urinary complain. A total of 219 (41.3%) complained of increased frequency, 116 (21.9%) complained of pain/burning micturition, 60 (11.3%) complained of discharge per vaginum out of which 41 (7.7%) said it was foul smelling, 195 (36.8%) had lower abdominal pain and 21 (3.9%) vaginal itching. These were examined by a gynaecologist and confirmatory diagnosis was made in 61 women after laboratory examination results. The average prevalence of PID was found to be 11.55% with 12.5% in rural areas and 10.6% in urban areas [Table/Fig-2]. It varied over the different age groups and the prevalence was seen to be increasing with age.
Prevalence of PID compared with area of residence.
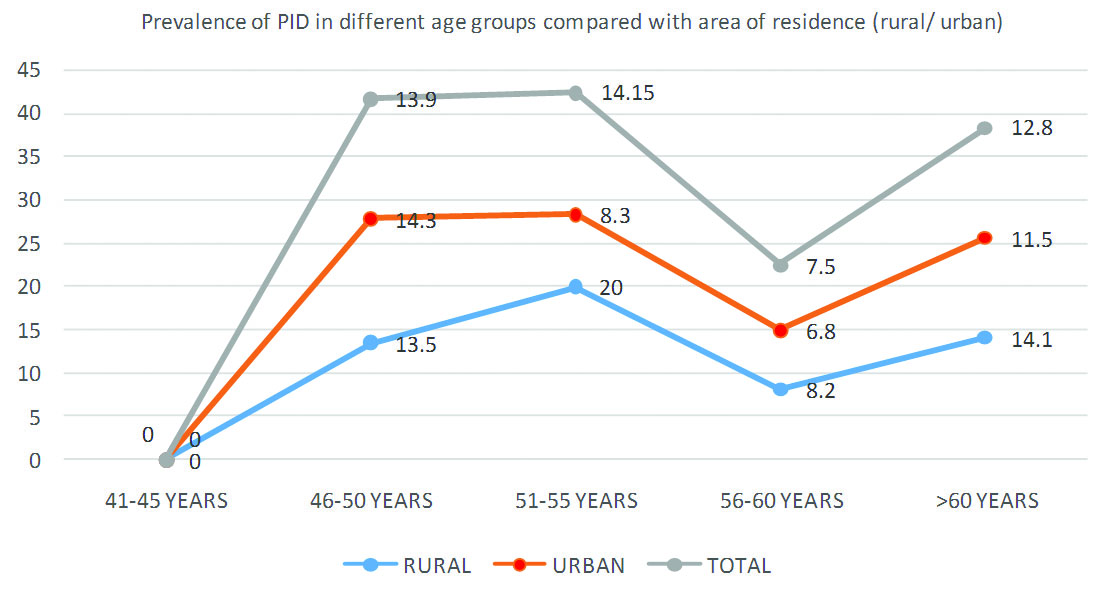
As seen in [Table/Fig-3], higher prevalence was found in rural areas compared to the urban areas. This difference in prevalence of PID over age groups in rural and urban areas was found to be significant (p<0.05). The difference with respect to occupation was found to be significant. The personal habits of the study subjects were analyzed for the presence of risk factors and it was found that presence of obesity, smoking habits and tobacco chewing were not found to be significantly associated.
Association of PID with socio-demographic factors.
| Variable | Absent*N (%) | Present*N (%) | Chi square value | p-value | Odd’s ratio | 95% Confidence Interval(Upper limit-Lower Limit) |
|---|
| Residence |
| Rural | 232 (87.5) | 33 (12.5) | 0.463 | 0.293 | 1.204 | 0.705-2.056 |
| Urban | 237 (89.4) | 28 (10.6) | 1 (ref) | |
| Religion |
| Hindu | 232 (91.0) | 23 (9.0) | 3.494 | 0.174 | 1.190 | 0.148-9.566 |
| Muslim | 225 (85.9) | 37 (14.1) | 1.973 | 0.249-15.629 |
| Others | 12 (92.3) | 1 (7.7) | 1 (ref) | |
| Marital Status |
| Married | 294 (87.2) | 43 (12.8) | 2.470 | 0.291 | 1.560 | 0.841-2.896 |
| Single | 15 (83.3) | 3 (16.7) | 2.133 | 0.554-8.211 |
| Widowed | 160 (91.4) | 15 (8.6) | 1 (ref) | |
| Education Status€ |
| Illiterate, Non-formal education | 377 (88.3) | 50 (11.7) | 1.014 | 0.798 | 0.696 | 0.230-2.111 |
| Primary | 39 (90.7) | 4 (9.3) | 0.538 | 0.122-2.375 |
| High school | 32 (91.4) | 3 (8.6) | 0.492 | 0.100-2.426 |
| Intermediate and above | 21 (84.0) | 4 (16.0) | 1 (ref) | |
| Occupation€ |
| Unemployed/retired/homemaker | 388 (90.2) | 42 (9.8) | 10.020 | 0.040 | 0.216 | 0.019-2.438 |
| Unskilled/semi-skilled | 55 (78.6) | 15 (21.4) | 0.545 | 0.046-6.432 |
| Skilled | 4 (100.0) | 0 (0.0) | 0.000 | 0.000 |
| Clerical/shopkeeper/farmer | 20 (87.0) | 3 (13.0) | 0.300 | 0.020-4.418 |
| Professional | 2 (66.7) | 1 (33.3) | 1 (ref) | |
| Source of Income |
| Self | 71 (80.7) | 17 (19.3) | 9.319 | 0.054 | 3.592 | 0.443-29.104 |
| Spouse | 107 (86.3) | 17 (13.7) | 2.383 | 0.295-19.228 |
| Children | 248 (91.9) | 22 (8.1) | 1.331 | 0.168-10.552 |
| Old age pension schemes | 28 (87.5) | 4 (12.5) | 2.143 | 0.219-20.935 |
| Others | 15 (93.8) | 1 (6.2) | 1 (ref) | |
| Standard of Living Index |
| Low | 170 (89.5) | 20 (10.5) | 0.348 | 0.840 | 0.805 | 0.383-1.695 |
| Medium | 210 (88.2) | 28 (11.8) | 0.913 | 0.452-1.844 |
| High | 89 (87.3) | 13 (12.7) | 1 (ref) | |
| Socio-economic Classification† |
| V | 174 (89.7) | 20 (10.3) | 4.676 | 0.322 | 0.815 | 0.373-1.783 |
| IV | 161 (90.4) | 17 (9.6) | 0.749 | 0.335-1.675 |
| III | 29 (80.6) | 7 (19.4) | 1.712 | 0.606-4.838 |
| II | 27 (81.8) | 6 (18.2) | 1.576 | 0.532-4.671 |
| I | 78 (87.6) | 11 (12.4) | 1 (ref) | |
| Locality of Home |
| Congested | 291 (89.3) | 35 (10.7) | 0.497 | 0.284 | 0.823 | 0.480-1.414 |
| Not Congested | 178 (87.3) | 26 (12.7) | 1 (ref) | |
| Over-Crowding |
| Present | 272 (86.9) | 41 (13.1) | 1.897 | 0.107 | 1.485 | 0.844-2.613 |
| Absent | 197 (90.8) | 20 (9.2) | 1 (ref) | |
| Ventilation |
| Present | 165 (87.3) | 24 (12.7) | 0.408 | 0.307 | 1.195 | 0.691-2.066 |
| Absent | 304 (89.1) | 37 (10.9) | 1 (ref) | |
* N= Number of study participants, € Adapted from Kuppuswamy’s Socioeconomic status scale (2016), † Modified B. G. Prasad classification (2014)
Risk Factors for PID:
Age at menopause: There seemed to be no significant difference in the onset of earlier menopause and presence of PID [Table/Fig-4]. Also, the number of years spent in menopause did not play a significant role.
Association of PID with personal factors.
| Variable | Absent*N (%) | Present*N (%) | Chi square value | p-value | Odd’s ratio | 95% Confidence Interval(Upper limit-Lower Limit) |
|---|
| Obesity |
| Present | 166 (87.8) | 23 (12.2) | 0.126 | 0.412 | 1.105 | 0.637-1.917 |
| Absent | 303 (88.9) | 38 (11.1) | | | 1 (ref) | |
| Smoking |
| Present | 102 (90.3) | 11 (9.7) | 0.444 | 0.315 | 0.792 | 0.398-1.576 |
| Absent | 367 (88.0) | 50 (12.0) | | | 1 (ref) | |
| Pack-year |
| <10 years | 7 (87.5) | 1 (12.5) | 1.402 | 0.705 | 1.049 | 0.126-8.701 |
| 10-20 years | 63 (92.6) | 5 (7.4) | | | 0.583 | 0.224-1.517 |
| >20 years | 32 (86.5) | 5 (13.5) | | | 1.127 | 0.427-3.080 |
| Non-smokers | 367 (88.0) | 50 (12.0) | | | 1 (ref) | |
| Tobacco Chewing |
| Present | 92 (85.2) | 16 (14.8) | 1.455 | 0.150 | 1.457 | 0.788-2.693 |
| Absent | 377 (89.3) | 45 (10.7) | | | 1 (ref) | |
| Hypertension |
| Present | 99 (88.4) | 13 (11.6) | 0.001 | 0.542 | 0.868 | 0.411-1.833 |
| Absent | 370 (88.5) | 48 (11.5) | | | 1 (ref) | |
| Diabetes Mellitus |
| Present | 32 (86.5) | 5 (13.5) | 0.157 | 0.425 | 1.219 | 0.456-3.258 |
| Absent | 437 (88.6) | 56 (11.4) | | | 1 (ref) | |
| Parity |
| <3 | 45 (88.2) | 6 (11.8) | 4.056 | 0.132 | 1.297 | 0.510-3.298 |
| 3-5 | 142 (84.5) | 26 (15.5) | | | 1.780 | 1.010-3.137 |
| >5 | 282 (90.7) | 29 (9.3) | | | 1 (ref) | |
| History of Multiple Sexual Contacts |
| Present | 17 (70.8) | 7 (29.2) | 7.541 | 0.014 | 3.408 | 1.352-8.590 |
| Absent | 447 (89.2) | 54 (10.8) | | | 1 (ref) | |
| All Vaginal Deliveries |
| Yes | 460 (88.5) | 60 (11.5) | 0.023 | 0.677 | 1.174 | 0.146-9.429 |
| No | 9 (90.0) | 1 (10.0) | | | 1 (ref) | |
| Age at Menopause |
| 30-39 years | 2 (100.0) | 0 (0.0) | 5.476 | 0.065 | 0.000 | 0.000 |
| 40-49 years | 362 (86.8) | 55 (13.2) | | | 2.659 | 1.114-6.348 |
| 50-59 years | 105 (94.6) | 6 (5.4) | | | 1 (ref) | |
| History of Abdomino-pelvic Surgery |
| Yes | 99 (86.1) | 16 (13.9) | 0.833 | 0.2224 | 1.329 | 0.721-2.451 |
| No | 370 (89.2) | 45 (10.8) | | | 1 (ref) | |
| Years Spent in Menopause |
| 1-5 years | 146 (89.0) | 18 (11.0) | 0.881 | 0.830 | 0.783 | 0.397-1.545 |
| 5-10 years | 117 (89.3) | 14 (10.7) | | | 0.760 | 0.367-1.573 |
| 11-15 years | 78 (89.7) | 9 (10.3) | | | 0.733 | 0.318-1.690 |
| >15 years | 127 (86.4) | 20 (13.6) | | | 1 (ref) | |
| Associated Urinary Tract Infection |
| Present | 72 (86.7) | 11 (13.3) | 0.294 | 0.351 | 1.213 | 0.603-2.441 |
| Absent | 397 (88.8) | 50 (11.2) | | | 1 (ref) | |
| Associated Pelvic Organ Prolapse |
| Present | 84 (82.4) | 18 (17.6) | 4.672 | 0.027 | 1.919 | 1.054-3.491 |
| Absent | 385 (90.0) | 43 (10.0) | | | | |
* N= Number of study participants
Parity: PID was reported as 11.8%, 15.5% and 9.3% in women with parity >5, 3-5 and <3 respectively. As shown in [Table/Fig-4], this difference is not found to be significant. On applying binary logistic regression, the odds for parity 3-5 was 1.780 (95% CI, 1.010-3.137) and this was a significant finding. The association with the history of all vaginal deliveries and abdomino-pelvic surgery with PID was not significant as shown in [Table/Fig-4].
History of multiple sexual contacts: A significant association was found and presence of history of multiple sexual contacts was found to be having an odds of more than 3 in the presence of PID (95% CI 1.352-8.590) [Table/Fig-4].
Associated urinary tract infection and pelvic organ prolapse [Table/Fig-4]: 11 (33%) patients of PID were found to be having symptoms of urinary tract infection confirmed by routine and microscopic urine examination. The odds were 1.213 although the difference was not found to be significant. The odds of PID with pelvic organ prolapse was 1.919 (95% CI: 1.054-3.491), nearly two times, the result being significant.
Cervico-vaginal flora in postmenopausal women: In the present study, it was observed [Table/Fig-5] that out of the total 61 cases of PID found in rural and urban areas of the community, the maximum cases were of bacterial vaginosis (36.06%) and 3.27% of all cases of PID were associated with intra-epithelial lesions or malignancy of cervix.
Cervico-vaginal flora/ findings in study subjects diagnosed with PID.
| Study findings | PID Absent*N (%) | PID Present*N (%) |
|---|
| *Non-specific inflammation | 52 | 9 |
| *Bacterial Vaginosis | 11 | 22 |
| *TrichomonasVaginalis | 0 | 13 |
| *Fungal Smear | 0 | 10 |
| ‡Chlamydia trachomatis | 0 | 3 |
| ‡Neisseria gonorrhoeae | 0 | 2 |
| *Malignancy | 21 | 2 |
*According to Pap smear, ‡ five patients showed normal findings in Pap smear. They were diagnosed as cases of PID on the basis of clinical findings and microbiological analysis showing positive for Neisseria gonorrhoeae (two patients) and Chlamydia trachomatis (three patients).
Chronic diseases [Table/Fig-6]: 161 study subjects were suffering from a chronic illness (30.4% of the total). We included hypertension, diabetes mellitus, cardio-vasular disease, stroke and asthma in our study. Out of these, 20 were diagnosed with PID. This association (Pearson’s chi-square=0.189, p value=0.382) was statistically not significant.
Association of chronic diseases with PID.
| Chronic Disease | PID Absent*N (%) | PID Present*N (%) | *p-value |
|---|
| Hypertension | 89 (16.7) | 10 (18.7) | 0.270 |
| Diabetes Mellitus | 17 (3.2) | 2 (0.3) |
| Hypertension+ Diabetes Mellitus | 4 (0.6) | 2 (0.3) |
| *Others | 30 (5.7) | 7 (1.3) |
| None | 329 (62.0) | 40 (7.5) |
*CVS/ CNS/ Respiratory illness etc
Addiction: There was a high prevalence of smoking found in the study areas (21.3%), higher in rural areas (22.6%) than urban areas (20.0%) [Table/Fig-4]. As observed, smoke from local items like chillum and bidi was a common practice amongst elderly women in the community to sit together especially in the evenings of summer months, and during the day of the winter months and about 9.7% of the patients of PID were smokers although no significant relation between PID and smoking was found in the present study.
Discussion
PID is a predominately reproductive age illness and its highest prevalence is in the second and third decades of life. It is a very uncommon diagnosis in menopause. It is estimated that less than 2% of patients admitted to hospitals for salpingitis and tubo-ovarian abscess are postmenopausal [6]. In the present study, the average prevalence of PID was found to be 11.55% with 12.5% in rural areas and 10.6% in urban areas [Table/Fig-1,2]. It needs to be emphasized that no similar study has been done in the area before, so baseline measures for comparison are seriously inadequate.
Cervico-vaginal flora in postmenopausal women: In the present study, the cases were first screened on the basis of history and then confirmatory diagnostic methods were done. Apart from early studies very few reports on both the aerobic and anerobic flora of postmenopausal patients have been published. It is suggested by the literature review that menopause results in decrease in lactobacillus colonization.
A study done to reveal upper vaginal and cervical bacterial flora in menopausal women found majority of the culture samples to be sterile. One study reported that vaginal flora of menopausal women is not different from that found in children, young women, in pregnancy or postpartum. They documented that anaerobic germs isolated in their study are normal inhabitants of the vagina and cervix which may occasionally become pathogens [19]. According to the study by Tashijan JH et al., lactobacilli were the most commonly detected organism in postmenopausal group of study subjects [20]. Hillier SL et al., studied the vaginal microflora of postmenopausal women who had never received oestrogen replacement therapy and found Lactobacilli, Gardnerella vaginalis and coliforms [19]. The prevalence of bacterial vaginosis found in the present study (4.1%) is similar to that found by Cauci S et al., who reported that the prevalence of bacterial vaginosis was significantly lower overall in postmenopausal women (6.0%) (p=0.02) [21].
Risk factors for PID: Older women do not usually have risk factors, which can expose them to sexually transmitted microorganisms. With advancing age there are behavioural, physiologic and anatomic alterations that offer barriers to the usual means of developing PID. Uterine instrumentation is a risk factor associated with the development of PID in the postmenopausal woman [22]. Structural abnormalities of the genital tract, such as cervical stenosis, uterine anatomic abnormalities, and tubal disease, are also associated with an increased risk of developing PID. On pelvic examination, palpable indurated masses may be present, suggesting a possible genital tract malignancy [6]. The present study determined the association of prevalence of PID in postmenopausal women with smoking and chronic diseases, and did not find a significant association. A meta-analysis done to find out the factors responsible for chronic pelvic pain showed that it is predisposed by smoking, increased parity and chronic conditions although this study was not specific for postmenopausal women [23,24].
Limitation
In our study, we examined only the symptomatic women for clinical and laboratory examinations. This is a definite limitation of the study as a lot of women present in the community might be asymptomatic and harbouring the disease in its early stages. Better diagnostic modalities like ultrasonography could not be incorporated in the study due to increased cost.
Conclusion
Pelvic inflammatory disease is a significant public health issue with certain repercussion on women’s health and wellbeing in the long run. The study shows the hidden burden of the disease in the community and the associated risk factors, which can be prevented by life style and cultural changes if incorporated earlier in the lives. There is a pressing need to create awareness among the women of the community regarding the identification and early reporting of symptoms. Other than the chronicity of lower abdominal pain ruining the wellbeing of the affected women, infertility and the associated stigma, the absolute dearth of literature on the subject compounds the need to study this issue in developing countries.
* N= Number of study participants, € Adapted from Kuppuswamy’s Socioeconomic status scale (2016), † Modified B. G. Prasad classification (2014)
[1]. Findik FM, Agacayak E, Icen MS, Evsen MS, Fırat U, Uterine abscess caused by the use of intrauterine device in a 62-year-old patient: A case reportJ Clin Case Rep 2015 5(12):676 [Google Scholar]
[2]. Thakur JS, Swami HM, Bhatia SPS, Efficacy of syndromic approach in management of reproductive tract infections and associated difficulties in a rural area of ChandigarhIndian Journal of Community Medicine 2002 27(2):77-79. [Google Scholar]
[3]. Balamurugan SS, Bendigeri ND, Community based study of reproductive tract infections among women of reproductive age group in urban health training centre area in Hubli, KarnatakaIndian Journal of Community Medicine 2012 37(1):34-38. [Google Scholar]
[4]. Garcia G, Vera R, ElMasri W, Pelvic inflammatory disease in a postmenopausal patient with bilateral tubal ligationEl Paso Physician 2006 30(1):21-22. [Google Scholar]
[5]. Bhurt AW, Fikree FF, Bhurt AM, Prevalence and risk factors of symptoms of pelvic inflammatory disease in a rural community of Jamshoro, Sindh, PakistanJ Pak Med Assoc 1999 49(8):188-94. [Google Scholar]
[6]. Jackson SJ, Soper DE, Pelvic Inflammatory disease in the postmenopausal womanInfectious Diseases in Obstetrics and Gynecology 1999 7:248-52. [Google Scholar]
[7]. Chappell CA, Wiesenfeld HC, Pathogenesis, diagnosis and management of severe pelvic inflammatory disease and tuboovarian abscessClinical Obstetrics & Gynecology 2012 55(4):893-903. [Google Scholar]
[8]. Nandan D, Misra SK, Sharma A, Jain M, Estimation of prevalence of RTIs/STDs among women of reproductive age group in district AgraIndian Journal of Community Medicine 2002 27(3):110-13. [Google Scholar]
[9]. Centers for Disease Control and PreventionSexually transmitted diseases treatment guidelinesMMWR 2006 55(RR-11):56-61.Available at https://www.cdc.gov/std/treatment/2006/rr5511.pdf Accessed on 23.01.2017 [Google Scholar]
[10]. Hollier LM, Workowski K, Treatment of sexually transmitted diseases in womenObstet Gynecol Clin North Am 2003 30(4):751-75. [Google Scholar]
[11]. Rathore M, Swami SS, Gupta BL, Sen V, Vyas BL, Bhargav A, Community based study of self-reported morbidity of reproductive tract among women of reproductive age in rural area of RajasthanIndian Journal of Community Medicine 2003 28(3):117-21. [Google Scholar]
[12]. Mitchell C, Prabhu M, Pelvic Inflammatory disease: current concepts in pathogenesis, diagnosis and treatmentInfectious Disease Clinics of North America 2013 27(4):793-809. [Google Scholar]
[13]. Bang RA, Bang AT, Baitule M, Choudhary Y, Sarmukkadam S, Tale O, High prevalence of gynaecological diseases in rural Indian womenThe Lancet 1989 1:85-88. [Google Scholar]
[14]. Bhole VD, Bendale TU, A descriptive study of PID at a tertiary care hospitalMed Pulse-International Medical Journal 2015 2(9):512-14. [Google Scholar]
[15]. Schwebke JR, Hillier SL, Sobel JD, Validity of the vaginal gram stains for the diagnosis of bacterial vaginosisObstet Gynecol 1996 88(4):573-76. [Google Scholar]
[16]. Brotman RM, Shardell MD, Gajer P, Fadrosh D, Chang K, Silver M, Association between the vaginal microbiota, menopause status and signs of vulvovaginal atrophyMenopause 2014 21(5):450-58. [Google Scholar]
[17]. Soules MR, Sherman S, Parrott E, Executive summary: Stages of Reproductive Aging Workshop (STRAW)5th ed:874-78. [Google Scholar]
[18]. Puri S, Bhatia V, Mangat C, Perceptions of menopause and postmenopausal bleeding in women of Chandigarh, IndiaThe Internet Journal of Family Practice [Internet] 2007 6(2)Available from: http://ispub.com/IJFP/6/2/11408 [Date of access: 25 Nov 2013] [Google Scholar]
[19]. Hillier SL, Lau RJ, Vaginal microflora in postmenopausal women who have not received estrogen replacement therapyClinical Infectious Diseases 1997 25(2):123-26. [Google Scholar]
[20]. Tashjian JH, Coulam CB, Vaginal flora in asymptomatic womenMayo Clin Proc 1976 51(9):557-61. [Google Scholar]
[21]. Cauci S, Driussi S, De Santo D, Penacchioni P, Lannicelli T, Lanzafame P, Prevalence of bacterial vaginosis and vaginal flora changes in peri- and postmenopausal WomenJ Clin Microbiol 2002 40(6):2147-52. [Google Scholar]
[22]. Lipscomb GH, Ling FW, Tubo-ovarian abscess in postmenopausal patientsSouth Med J 1992 85(7):696-99. [Google Scholar]
[23]. Latthe P, Mignini L, Gray R, Hills R, Khan K, Factors predisposing women to chronic pelvic pain: systematic reviewBMJ 2006 332:749 [Google Scholar]
[24]. Luborsky JL, Meyer P, Sowers MF, Gold EB, Santoro N, Premature menopause in a multi-ethnic population study of the menopause transitionHum Reprod 2003 18(1):199-206. [Google Scholar]