Primary Ovarian Endometrioid Stromal Sarcoma Presenting with Infertility
Sandhya Ilanthodi1, Vishwanath Meghashree2, Muktha Ramesh Pai3
1 Associate Professor, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Mangaluru, Karnataka, India.
2 Postgraduate Student, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Mangaluru, Karnataka, India.
3 Professor, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Mangaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vishwanath Meghashree, 104, ‘Deepa Residency’, Warehouse Cross Road, Kodialguthu West, Mangaluru-575004, Karnataka, India.
E-mail: v.megharox@gmail.com
Endometrioid Stromal Sarcoma (ESS) is an uncommon tumour that occurs in women over wide age range of 11 years to 76 years accounting for only 0.2% of all uterine malignancies and for 15%–26% of primary uterine sarcomas. These tumours arising from ovary are extremely rare. Most of them are associated with nulliparous or perimenopausal women. It is commonly associated with endometriosis of the ovary. Here we present this rare case to emphasize on the uniqueness and histomorphology of ovarian ESS in patients with endometriosis.
Endometriosis, Ovarian neoplasms, Ovarian sarcoma
Case Report
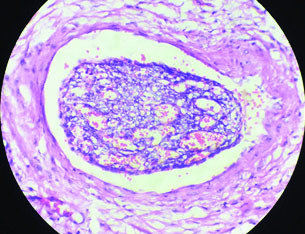
A 34-year-old woman came to gynaecology outpatient department with the complaint of infertility. She was married for 10 years. Her menstrual cycles were regular but were associated with dysmenorrhoea. As part of investigation for infertility, ultrasonogram was done which revealed a left ovarian tumour with adhesions. MRI showed an enhancing lesion with solid and cystic components measuring 11 cm x 9.8 cm x 6 cm in left adnexa with extensions anteriorly upto the anterior abdominal wall, posteriorly infiltrating the uterus and laterally upto the left ileus muscle. Left salphingo-oophorectomy was performed and specimen was sent for histopathology. Tumour arising from left ovary showed broad papillary excrescences (Tombstone appearance) with a solid, yellowish cut surface [Table/Fig-1].
Gross appearance of left ovarian tumour (Tombstone appearance).

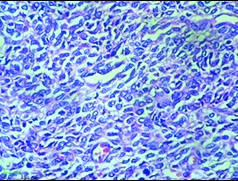
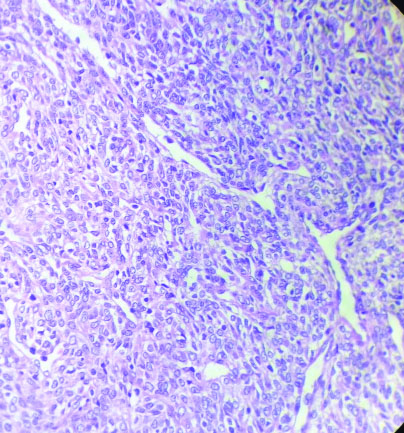
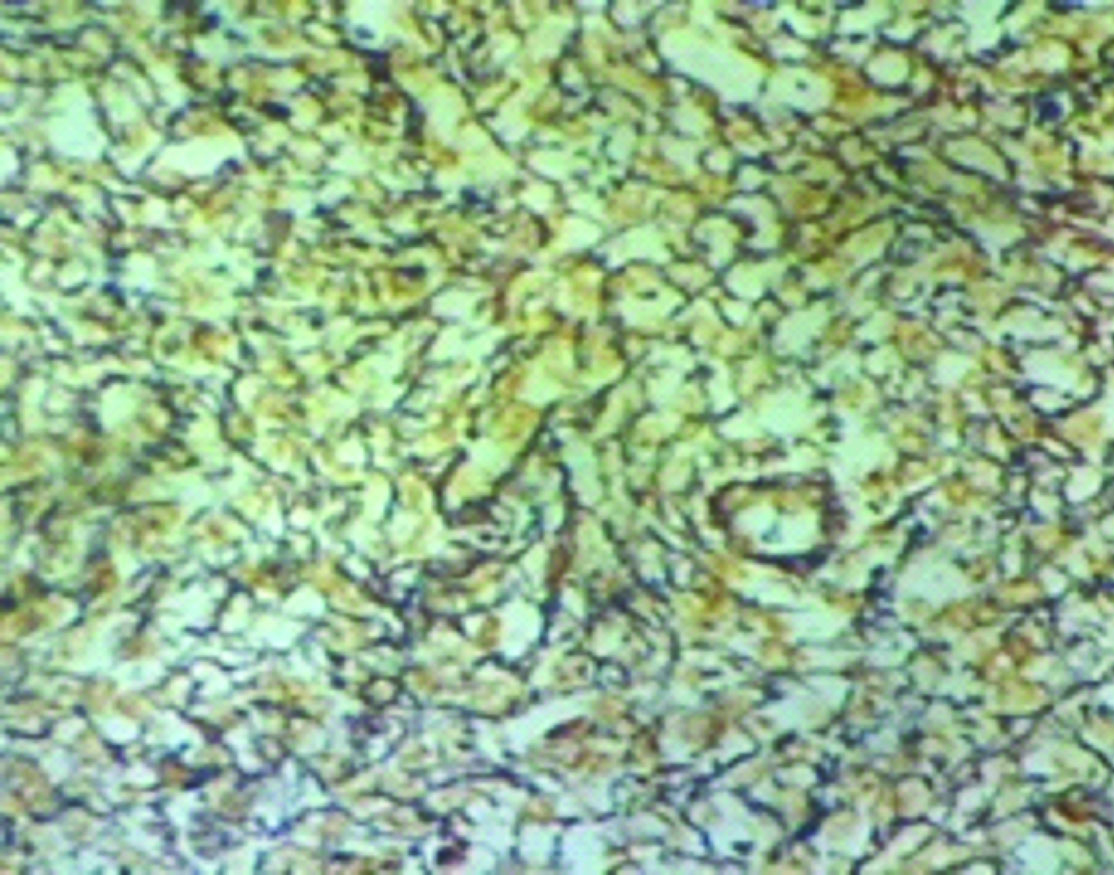
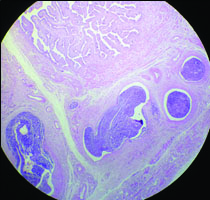
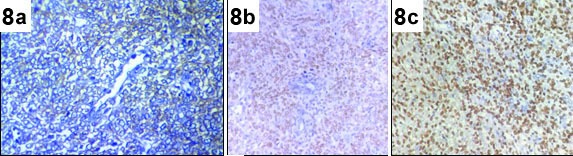
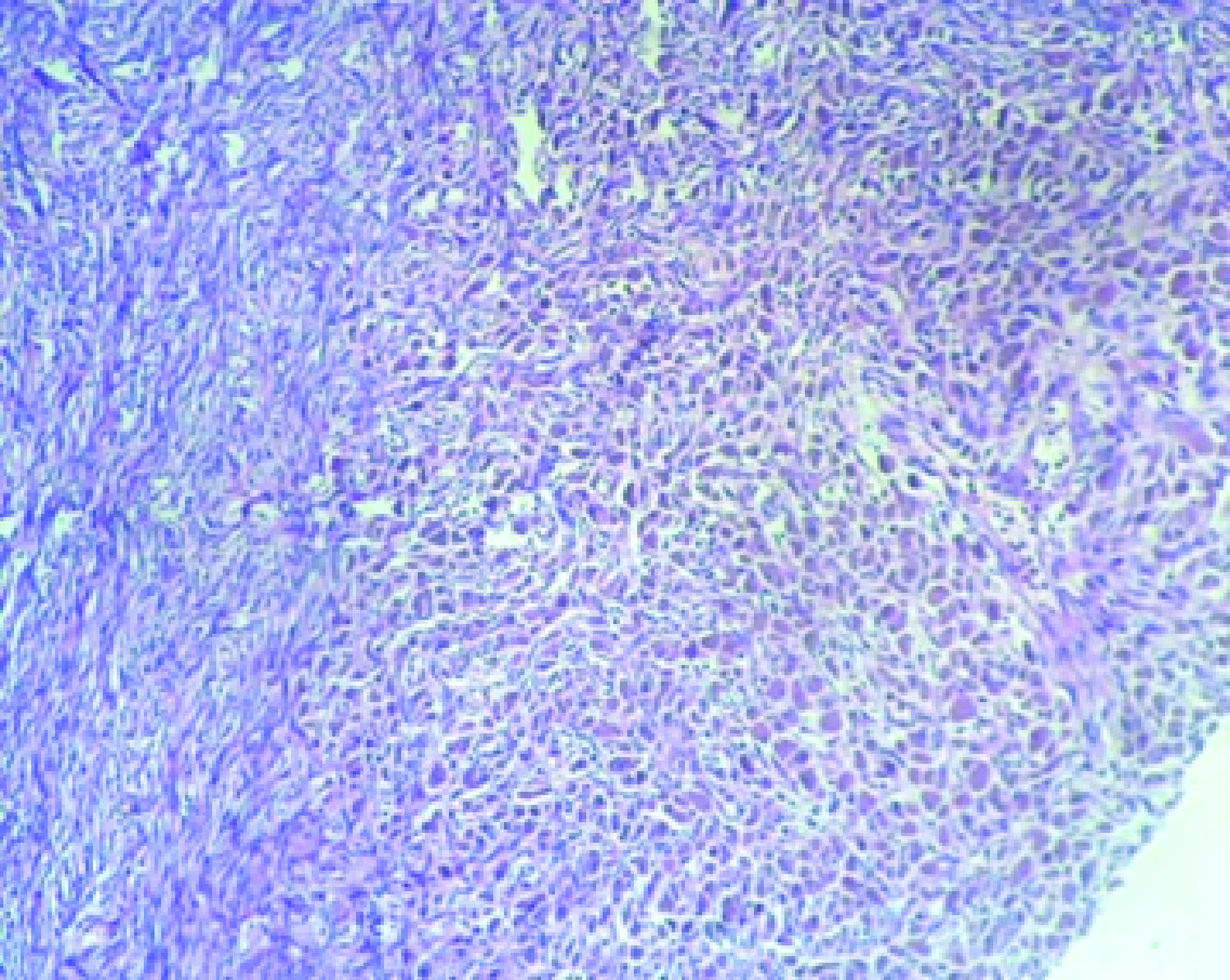
Microscopy showed ovarian stroma along with tumour tissue having infiltrating borders with moderately pleomorphic round to oval cells arranged haphazardly in a diffuse pattern and separated by thick band of fibrous septa forming distinct nodules [Table/Fig-2]. The nodules were punctuated by thick walled blood vessels [Table/Fig-3] with focal haemangiopericytomatous pattern [Table/Fig-4]. These vessels were surrounded by whorls of neoplastic cells. Reticulin stain showed delicate fibrils characteristically enveloping individual tumour cells [Table/Fig-5]. There were about six to eight mitotic figures /10 High Power Fields (HPF). Gonadal vessels showed tumour invasion [Table/Fig-6]. Left fallopian tube showed endolymphatic stromal myosis [Table/Fig-7]. A diagnosis of ovarian ESS was made. Immunohistochemistry with Oestrogen Receptor (ER), Progesterone Receptor (PR) and CD10 marker was strongly positive in tumour cells confirming the diagnosis [Table/Fig-8].
Thick fibrous band separating tumour cells into nodules (H&E x100).
Punctuated arterioles and tumour cells having round to oval nuclei (H&E x400). (Images left to right)
Hemangiopericytomatous patten (H&Ex200).
Reticulin Stain showing delicate fibrils enveloping individual tumour cells(X400)
Infiltration of Left gonadal vessels (H&E x200).
Infiltration of left fallopian tube in the form of endolymphatic stromal myosis (H&E x200).
Strong positivity of immunohistochemical markers (x400): a) CD10; b) ER; c) PR. (Images left to right)
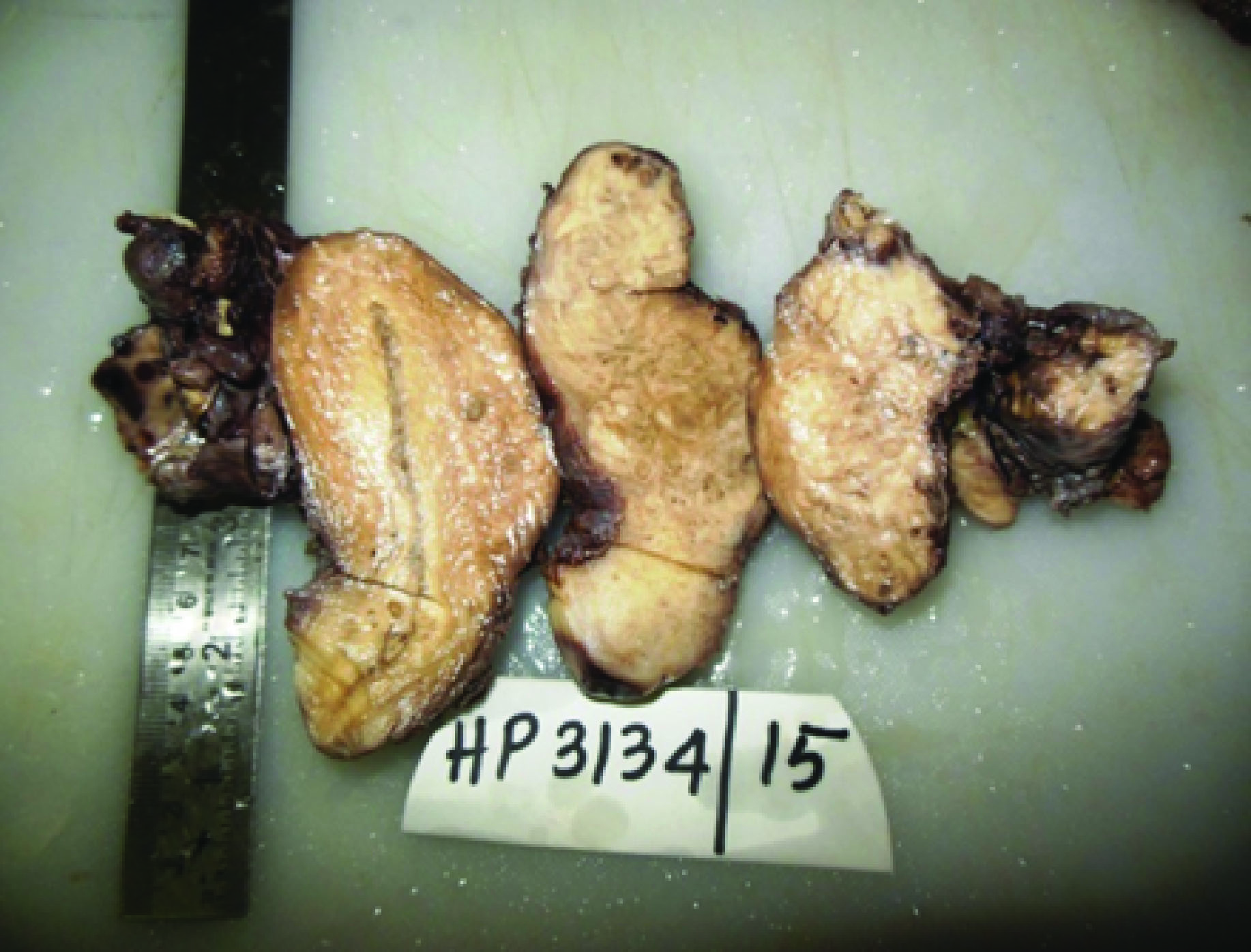
Further hysterectomy with right salphigo-oophorectomy was done. The tumour was seen infiltrating into the left fallopian tube, cervix and posterior aspect (muscular part near the serosa) of the uterus sparing the endometrium [Table/Fig-9]. Parametrium showed tumour deposits. Sections from uterus confirmed tumour infiltration into the fundus but sparing the endometrium. Sections from the right ovary showed presumptive endometriosis with haemosiderin laden macrophages surrounded by endometrial stroma [Table/Fig-10]. After analyzing histomorphological features with the special stains and immunohistochemical markers, diagnosis of extra uterine ESS was considered.
Gross appearance of uterus with invasion of the tumour from posterior aspect sparing endometrium.
Presumptive endometriosis in the ovary (H&E X200).
The cytoreductive surgery was followed by six cycles of chemotherapy (paclitaxel and carboplatin) which was started one month after the surgery followed by vaginal cuff brachytherapy. The patient was then put on letrozole. Vaginal brachytherapy though a form of treatment modality for uterine variant of endometrial stromal sarcoma, was given to the patient in this case, as there was involvement of cervix and posterior myometrium by the tumour. A reassessment contrast enhanced computed tomography of whole abdomen was done after three and half months of starting chemotherapy which revealed an osteolytic lesion with cortical erosion in the ala of the sacrum along with iliac lymphnode enlargement- suggesting metastases. Injection zoledronic acid and palliative radiotherapy was administered for bony metastases. The patient was on maintenance of megestrol acetate and lost to follow up.
Discussion
Endometrioid stromal tumours comprise a spectrum of mesenchymal neoplasms occuring predominantly in the uterus and are rare in extra uterine sites including ovary. They arise from the mesenchymal component of the endometrium or the mesenchymal component of the endometriosis in extrauterine sites. These tumours occur in women over wide age range of 11-76 years [1]. These are monophasic sarcomas characterized by diffuse proliferation of tumour cells similar to the stroma of proliferating endometrium.
Primary ovarian ESS (commonly occur as metastasis from the uterus) are rare and 60% of them are associated with endometriosis [2]. In a study by Chang KL et al., and Young RH et al., among their 23 reported cases, 63% were found associated with endometriosis [3,4]. Though the pathogenesis of sarcoma is not well established, an association with endometriosis is noted [5]. Sarcomas are the second and third most frequent endometriosis-associated extra ovarian and ovarian tumours, respectively [5].
Endometriosis though a common benign gynaecologic condition, it is estimated that upto 1% of women develop endometriosis associated malignancy [6]. ESSs arising due to malignant transformation of endometriotic foci were first established in 1920s [6]. Since then only a handful of cases have been reported. Most of the ESSs reported in literature are arising from the uterus of patients with menometrorrhagia [7]. Gastrointestinal tract is the most common extra uterine site for endometriosis associated ESS, although cases have been reported in ovary, omentum, mesentry, vagina, cervix, rectovaginal septum, parametrium, fallopian tube, liver and sciatic nerve [6]. Patients usually are nulliparous with irregular vaginal bleeding, pelvic pain/pressure and an abdominal mass or discomfort.
When ESS occurs in ovary, first differential diagnosis to be considered is metastasis from the uterus. But in our case, tumour was primarily seen in the ovary metastatic to the posterior surface of the uterus into the myometrium sparing the endometrium with evidence of presumptive endometriosis (haemosiderin laden macrophages and endometrial stroma) both in affected ovary as well as the contralateral ovary, thus ruling out a primary uterine tumour.
Grossly, ESS often forms distinctive finger-like projections that invade the myometrium, veins, and lymphatics. Microscopically low grade sarcomas mimic the stroma of proliferative phase of endometrium punctuated by arterioles and separated into nodules by thick fibrous septa [1]. These fibrous areas can mimic thecoma of ovary. There were about six to eight mitotic figures noted per 10 hpf in the present case. It is said that primary ovarian ESS behave like low grade uterine ESS and have mitotic rate ranging from 7-17/10 hpf. High grade sarcomas have moderate nuclear atypia with frequent mitosis. Primarily ovarian ESS needs to be differentiated from granulosa cell tumour. Nuclear features of granulosa cell tumour help us to differentiate it. Other sex cord stromal tumours such as thecoma of ovary and carcinosarcoma are to be considered in the differential diagnosis. ESSs are positive for immunohistochemical markers ER, PR and CD10 thus, differentiating from carcinosarcoma, granulosa cell tumour and other sex cord stromal tumours of ovary.
Management strategy includes cytoreductive surgery, hormone therapy (is effective in ESS because of oestrogen and progestron receptors in it) with megestrol/medroxy progesterone, Gonadotropin Releasing Hormone (GnRH) analogues and aromatase inhibitors [8]. Radiotherapy in the form of brachytherapy with or without pelvic radiation is used as adjuvant therapy for control of local recurrences. At FIGO Stage I, the five-year survival rate for ESS is 54% to nearly 100% and at Stage III is 30%. For advanced disease (Stage III and IV) the survival is only 11%.
Although ESS are slow growing and have an indolent course with a better prognosis than other ovarian sarcomas, they are known to recur. The risk of recurrence is as high as 50% along with interval for recurrence and a median interval of about five years from hysterectomy to relapse [7]. But in the present case, metastases were seen within a year of surgery.
Young age at presentation, seeking medical help for infertility with metastases within a year of tumour excision makes this case an unusual one.
Conclusion
Ovarian tumours display a wide spectrum of tumours including sarcomas. ESS primarily occurring in ovary should be considered in cases of work up with infertility as well as in cases of endometriosis in the differential diagnosis. Grossly, these tumours display a wide spectrum of presentation and microscopically resemble granulosa cell tumour. Although, ESS have an indolent course and behave like low grade ESS of their uterine counterpart, this case presented with metastases within a year of diagnosis thus creating awareness on the potential behaviour of these tumours.
[1]. Lee KR, Tavassoli FA, Prat J, Dietel M, Gersell DJ, Surface epithelial-stromal tumours. In: Tavassoli FA, Devilee P(Eds): World Health Organisation Classification of TumoursPathology and Genetics of Tumours of the Breast and Female Genital Organs 2003 4th edLyonIARC Press:134-35. [Google Scholar]
[2]. Jeffrey D, Seidman Peter Russel, Robert JK, Surface epithelial tumours of the ovary. In: Robert J.KurmanBlaustein’s Pathology of the Female Genital Tract 2002 5th edNew YorkSpringer:887 [Google Scholar]
[3]. Chang KL, Crabtree GS, Lim-Tan SK, Kempson RL, Hendrickson MR, Primary extrauterine endometrial stromal neoplasms: A clinicopathologic study of 20 cases and a review of the literatureInt J Gynecol Pathol 1993 12:282-96. [Google Scholar]
[4]. Young RH, Prat J, Scully RE, Endometrioid stromal sarcomas of the ovary-a clinicopathologic analysis of 23 casesCancer 1984 53(5):1143-55. [Google Scholar]
[5]. Baiocchi G, Kavanagh JJ, Wharton JT, Endometrioid stromal sarcomas arising from ovarian and extraovarian endometriosis- report of 2 cases and review of the literatureGynecol Oncol 1990 Jan 36(1):147-51. [Google Scholar]
[6]. Wong J, Tan G, Chia C, Selvarajan S, Teo M, A rare case of multiple malignancies arising in endometriosis: diffuse extra-uterine high-grade endometrial stromal sarcoma and ovarian carcinomaAmerican Journal of Cancer Case Reports 2015 3:1-8. [Google Scholar]
[7]. Berceanu S, Patrascu A, Berceanu C, Tica AA, Badulescu A, Endometrial stromal sarcoma: clinico-pathological report of four cases and review of the literatureRomanian Journal of Morphology and Embryology 2008 49(2):251-55. [Google Scholar]
[8]. Puliyath G, Nair MK, Endometrial stromal sarcoma: A review of the literatureIndian J Med Paediatr Oncol 2012 33(1):1-6. [Google Scholar]