With an incidence rate of 9%, dry eye syndrome is a common condition that causes different amounts of discomfort and disability, especially in patients over 40 years of age. It can result in visual disturbance and instability in the tear film, due to the increase of tear film osmolarity and inflammation of ocular surface, or the overall lack of an appropriate and stable tear film [1,2].
A well-formed tear film is required for nourishing, lubricating, and protecting the ocular surface. Tear film instability may be caused by the dysfunction of any lachrymal or meibomian gland: eyelids, cornea, conjunctiva, or the connecting neural reflex circles.
Dry eye has been divided into two distinct etiological groups: Aqueous Tear Deficiency (ATD) and evaporative dry eye. The first group is further divided into Sjögren’s syndrome and non-Sjögren causes of lachrymal gland dysfunction. The second group includes intrinsic MGD and extrinsic causes (contact lens wear or ocular surface diseases, such as allergy) [1,2].
MGD is characterized by a chronic abnormality in the meibomian glands, which can be determined by way of an obstruction in its terminal duct, qualitative and quantitative changes in secretion and consecutive tear film instability, inflammation, and ocular surface diseases. Meibomian gland secretions (consisting of different polar and non-polar lipids) spread across the tear film and facilitate slow evaporation of aqueous components, thereby, maintaining a translucent optical surface. Thus, it can prevent any adhesion of microbial agents and organic matter, such as dust and pollen [3]. A high level of inflammatory mediators has also been identified in the tear films of patients with MGD [4].
Various drugs and anti-inflammatory agents are used in the treatment of dry eye and MGD, but due to the chronic nature of dry eye, long-term treatment with drugs often leads to side-effects, such as the incidence of glaucoma or cataract, in many patients. Green tea exhibits anti-oxidative, anti-bacterial, anti-androgen and immunomodulatory properties. One of the main components extracted from green tea is Epigallocatechin Gallate (EGCG). The substance has an inhibitory effect on inflammation, through the suppression of IL-1, IL-6, MCP-1 and TNF-α and through inhibition of NF-kB’s activation. Ointment made from plant extracts is useful in the treatment of impetigo contagiosa [5,6]. In addition, green tea extract has been used in the treatment of acne vulgaris. Its effect on acne vulgaris may be due to modulation in the androgenic activity; however, this observation needs further evaluation [6]. Another use of green tea is the safe, effective, and tolerable topical application of 10% and 15% of sinecatechins ointment for anogenital warts [7]. In addition, green tea has important benefits in reducing the incidence of selenite cataract, which further indicates the anti-cataract potential of green tea [8]. It was also found effective in treatment of vernal keratoconjunctivitis by suppressing of TNF-α, which plays an important role in causing allergic reactions [9].
Green tea seems to be potentially effective against UV damage in cultured human retinal pigmented epithelial cells. This was demonstrated by increased cell count and activity after UV irradiation [10–12]. The same research was directed at cultured human lens epithelium with the idea that green tea can support lens epithelial cells against UV damage [13].
This study was conducted to assess the efficacy of green tea extract in cases with dry eye and Meibomian Gland Dysfunction (MGD).
Materials and Methods
Study Design: For the double-blind randomized controlled clinical trial, 60 patients were selected from February to April 2014, based on the incidence rate of dry eye (9%) and an anticipated dropout rate of 10%.
Formula for calculating the sample size with prevalence rate of 9% and α=5% and drop out 10% is: n= (Z1 – α/2)2 p (1-p)/d2=56
These patients were further divided into two equal groups by the blocked randomization method. For all patients, scores of the right eye were recorded for statistical analysis. The study has been approved by the Ethics Committee of Shiraz University of Medical Sciences and the patients have provided informed consent prior to inclusion. Withdrawal from the study was allowed at any time after following standard treatment.
The study was also registered to the Iranian Registry of Clinical Trials (IRCT2014042117374N1). The inclusion criteria comprised of mild-to-moderate dry eye and MGD. Exclusion criteria consisted of the use of oral Tetracyclines and Corticosteroids up to three months before start of the trial, and any ophthalmic medication one month before the trial. Patients with other ocular surface disorders (except MGD) such as corneal surface damage and eyelid complications also fell within the exclusion criteria. In addition, patients with any previous ocular surgery, history of topical ocular drug allergy, use of medication to treat other ophthalmic conditions, as well as those with severe MGD and dry eye requiring systemic treatment, patients with nasolachrymal duct disorders, and those undergoing pregnancy, lactation, and other systemic disorders were excluded from the study. Standard treatment in the control group included artificial-tear eyedrops thrice a day for one month. In the intervention group, artificial tears were administered at the same frequency, combined with topical green tea extract three times a day for a month.
Preparation of the topical green tea extract: Firstly, fresh leaves from the tip of the green tea plant stem were collected from farms in the northern region of Iran. The leaves were then promptly transferred and dried in a laboratory environment. The dried leaves were gritted and the powder inserted in a sterile shaker to achieve uniformity. Following this, it was extracted by a percolator and hydro-alcoholic solution in 75°C for 72 hours. The extracts were concentrated to up to 4.5% of the dry remains after filtration, by a rotary device. It was then transferred to a refrigerator as a source of drop preparation. All processes were completed under sterile conditions. Each millilitre of the prepared extract was mixed with 5 ml of distilled water and allotted in to 10 ml-eyedrop-bottles for one week of usage by patients. After a week, the drop was replaced and the process was continued for a month. All patients were evaluated at the beginning and end of the study, under the following parameters.
1) Ocular symptoms were evaluated based on a standard questionnaire that included itching, burning sensation, reduced vision, foreign body sensation, photophobia, and redness. The response ‘0’ correlated to ‘never’, while a value of ‘4’ referred to ‘all of the time’. Finally, scores from these seven symptoms were summarized to arrive at a cumulative score of 28. For evaluation purposes, the symptoms were classified as Never-0, Rarely-1, Sometimes-2, Often-3, All of the time-4 [14].
2) Schirmer’s test [2,14] with anaesthesia was used to check for tear production. Results below 10 mm were considered within the dry eye category.
3) Tear film stability [2,14] was checked through TBUT. This was done through fluorescein paper with one drop of saline solution and without preservative material. If it lasted less than ten seconds, the eye was considered dry.
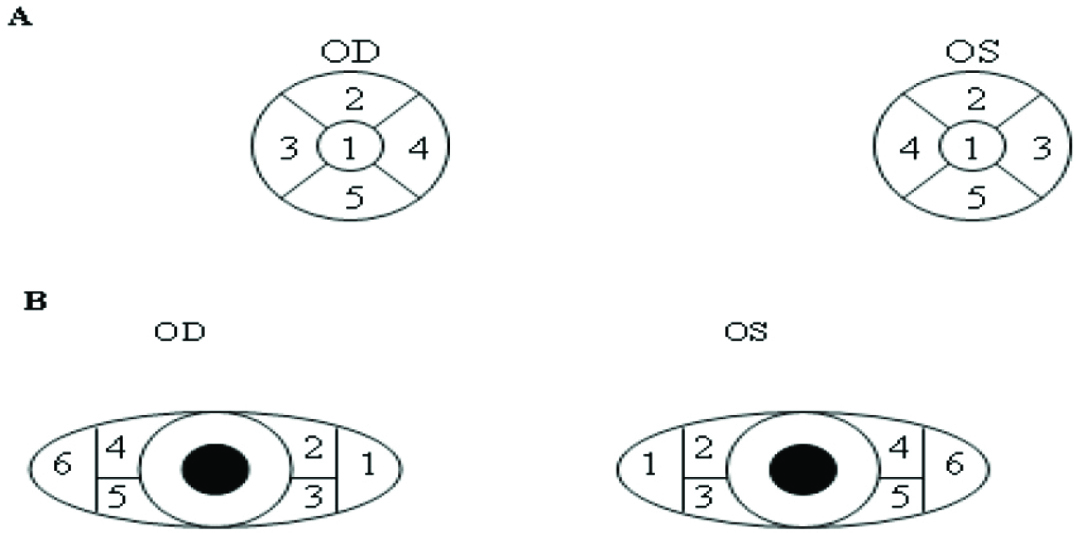
4) Ocular surface health [14] was evaluated by staining the cornea and conjunctiva with fluorescein [Table/Fig-1]. So, the cornea was divided into five areas: central, superior, inferior, nasal, and temporal {Grade 0 = no staining, Grade 1 = mild staining (micro-punctate), Grade 2 = moderate staining (macropunctat), Grade 3 = severe staining (confluent macro-punctate)}. Eventually, the scores of these items were added together to record a total of 15. For conjunctival staining, the conjunctiva is divided into six areas: supranasal, inferonasal, centronasal, supratemporal, inferotemporal, centrotemporal. {Grade 0 = no staining, Grade 1 = mild staining (micro-punctate), Grade 2 = moderate staining (macro-punctate), Grade 3 = severe staining (confluent macro-punctate)}. For evaluation of the scores, corneal and conjuctival staining were classified as None-0, Mild-1, Moderate-2, and Severe-3.
A. The five regions of the cornea were evaluated using fluorescein staining. B. The six areas of conjunctiva were evaluated using Rose Bengal staining.
5) For evaluation of meibomian-gland health [14], the patient was seated with the head resting comfortably on the slit lamp. Both lower lids were examined with the slit lamp illumination and 10X to 16X magnification. One sterile wooden-stemmed cotton-tipped applicator was used to press the lids against the globe, right at the margin, to express the gland contents [Table/Fig-2]. Meibomian gland health was evaluated in terms of its orifice and quality of sebum concentration {liquid (0), thick (1), granular (2), toothpaste (3)}, and its colour {clear (0), yellow (0.5), white (1)}. For final registration, scores of these items were added together.
Evaluation of Meibomian glands health based on its orifice and quality of sebum, concentration and colour of discharge [2,6].
| Score | AQuality | BColour |
|---|
| Liquid | Thick | Granular | Toothpaste | Clear | Yellow | White |
|---|
| Score | 0 | 1 | 2 | 3 | 0 | 0.5 | 1 |
Statistical Analysis
Finally, the data was analysed with statistical package for social science (SPSS-version 21) software, where it was presented as mean±standard deviation and percentages. Chi-square test was used for comparison of data. Means between differences were compared using Student’s t tests. Values of p less than 0.05 were considered to be statistically significant.
Results
Overall, 60 patients with impressions of mild-to-moderate dry eye with MGD were evaluated in the study. Most of patients in the green tea group (N=18) were female. Most patients in the control group were also females (N=20). Participants in the green tea group ranged from 30 to 70 years of age, with a mean age of 61 years. In the control group, participants were between 35 and 69 years, with a mean age of 64 years. At the baseline, patient characteristics in both groups did not significantly differ [Table/Fig-3]. The symptom scores of itching, burning, reduced vision, foreign body sensation; pains, photophobia, and redness in the green tea group were 9±0.86, which improved to 4.86±0.55 after a month. For the control group, the scores were 9.03±0.75, which improved to 6.63±0.46. The changes in the green tea group were statistically significant as compared to the control (p=0.002).
Changes from baseline in the objective clinical measures after one month from using green tea.
| Variables | Green tea group | Control group |
|---|
| Baseline | One Month Later | Baseline | One Month Later | p-Value* |
|---|
| Symptoms score(0 to 28) | 9±0.86 | -4.1±2.27 | 9.03±0.75 | -2.4±1.88 | 0.002 |
| Schirmer test score (mm) | 8.2±0.30 | 0.4±0.72 | 8.16±0.29 | 0.3±0.91 | 0.641 |
| Tear breakup time (s) | 6.1±0.23 | 3.03±1.29 | 6.3±0.25 | 1.03±0.80 | 0.001 |
| Corneal staining score (0 to 15) | 3.8±0.22 | -0.13±0.73 | 4.06±0.20 | +0.10±0.71 | 0.215 |
| Conjunctival staining score (0 to 18) | 8.06±0.24 | -0.16±0.69 | 7.56±0.25 | -0.43±0.81 | 0.180 |
| Meibum quality score (0 to 4) | 1.06±0.09 | -0.35±0.26 | 1.03±0.09 | -0.13±0.26 | 0.002 |
*The P-value is associated with comparing two groups of control and green tea one month later using green tea.
Differences in the Schirmer’s test score as a measure of tear production were not too significant between the two groups, both at the baseline and the end of the study. Furthermore, changes in the score for each group at the baseline and end of the study were not significant.
Significant improvement was seen in TBUT in the green tea group at the end of study. In the control group, the change was not significant. The difference between both groups was statistically significant (p=0.001).
Corneal fluorescein staining scores did not show significant change in both groups. Besides, the difference in corneal fluorescein staining scores between the two groups was not statistically significant. Conjunctival staining scores were also not significantly enhanced in both groups.
The health of meibomian glands and their secretions improved in both the groups after a month. The average medium quality significantly improved, and this difference between the two groups was statistically significant (p=0.002). Changes from the baseline in impartial clinical measures at the one-month time point, with pertinent p-values for both groups, are summarized in [Table/Fig-3].
Discussion
Dry eye and MGD are the most common causes behind clinical complaints in ophthalmology [1,15]. Inflammation of the meibomian glands induces MGD, which in turn causes evaporative dry eye. MGD may result in alteration of the tear film, symptoms of eye irritation, and ocular surface diseases [15]. There are many drugs and anti-inflammatory preparations used to counter this, but in the long-term, the chronic nature of the problem can result in the emergence of side-effects from conventional treatment [2,16]. So, green tea extract was evaluated as a potentially safe anti-inflammatory agent. To determine the effect of green tea on MGD and evaporative dry eye, we conducted a double-blind clinical trial where patients were randomly assigned to either the green tea group or the control group. The main parameters used to evaluate the participants were Schirmer’s test, TBUT, corneal and conjunctival staining, and meibum content, at a one-month time point.
Evaluation of both groups at the baseline showed similar characteristics. Overall, dry eye and MGD is seen more commonly in women than men, and this was compatible with our study results. Even though the mechanism of inflammation in men and women is similar, the function and levels of androgens, which play an important role in the function of meibomian glands, were not alike.
We evaluated the symptoms of patients according to OSDI scores. Patients in the green tea group had statistically-significant improvement in their overall OSDI scores. Thus, the clinical score could be used as a therapeutic determinant.
Another interesting finding was the significant improvement in both TBUT and meibum quality in the green tea group, which suggests, an enhancement in lipid layer and improvement in tear film stability.
There was no statistically-significant increase in Schirmer scores for either group. A number of probable causes could be responsible for this, such as the dosing schedule, time and frequency of topical administration, and the length of the study for patients with dry eye syndrome.
Ocular surface health was assessed by corneal and conjunctival fluorescein staining, but this did not deliver any statistically-significant improvement in scores for both groups.
The absence of correlation between significant increases in OSDI scores and the lack of significant improvement in staining in the green tea group could be due to the short period of the study. In addition, the use of Rose Bengal staining for conjunctiva could be effective in yielding better results.
Limitation
Some of limitations of the study were poor cooperation from elderly patients and resulting in difficulty in conducting and evaluating the mentioned tests on them. In addition, many patients were affected by anxiety due to the chronic nature of dry eye syndrome. Continuing the study proved difficult for them, and these patients were referred to a psychiatrist for simultaneous treatment of non-pharmaceutical problems.
Conclusion
Our study shows that, green tea extract improves ocular surface inflammation, TBUT and meibum score in patients with evaporative dry eyes and MGD, based on the OSDI symptoms questionnaire. Thus, this treatment can decrease the clinical signs and inflammatory changes in evaporative dry eyes and MGD by suppressing the inflammatory cytokine expression. Furthermore, EGCG could be used therapeutically for the treatment of dry eye and MGD. Additional studies are needed to establish the favourable dosage of green tea extract. Our study shows that, the most hopeful endpoints for further clinical trials would include dry eye and MGD.
Financial support: This study was financially supported by Shiraz University of Medical Sciences.
*The P-value is associated with comparing two groups of control and green tea one month later using green tea.