Introduction
The distal humeral fractures are common fractures of upper limb and are difficult to treat. These fractures, if left untreated or inadequately treated, leads to poor outcomes. Management of distal humeral fractures are pertained to many controversies and one among them is position of plates.
Aim
To compare the clinical and radiological outcomes in patients with intra-articular distal humerus fractures, treated using parallel and perpendicular double plating methods.
Materials and Methods
A total of 38 patients with distal humerus fractures, 20 in perpendicular plating group (group A) and 18 in parallel plating group (group B), were included in this prospective randomised study. At each follow up patients were evaluated clinically and radiologically for union and the outcomes were measured in terms of Mayo Elbow Performance Score (MEPS) consisting of pain intensity, range of motion, stability and function. MEP score greater than 90 is considered as excellent; Score 75 to 89 is good; Score 60 to 74 is fair and Score less than 60 is poor.
Results
In our study, 15 patients (75%) in group A, and 13 patients (72.22%) in group B achieved excellent results. Two patients (10%) in group A and 4 patients (22.22%) in group B attained good results. Complications developed in 2 patients in each groups. No significant differences were found between the clinical outcomes of the two plating methods.
Conclusion
Neither of the plating techniques are superior to the other, as inferred from the insignificant differences in bony union, elbow function and complications between the two plating techniques.
Introduction
The integrity of elbow joint is important for proper functioning of the entire upper limb and if it gets affected especially by distal humeral fractures leads to significant disorders. Distal humeral fractures, are those occuring within a square of lower end humerus, whose base is the distance between the epicondyles, on an anteroposterior radiograph. The treatment of these fractures is complex due to their, proximity to vital structures, complex anatomy, injury patterns, associated osteoporosis in elderly patients and limited space for instrumentation.
The available options, for this type of fractures are, crossed screws or pinning, double tension banding technique, single plating techniques, dual plating techniques, minimal osteosynthesis and mobile fixation with hinged external fixators, hemiarthroplasty, and total elbow replacement. The recent trend for displaced, intra-articular fractures of the distal humerus is, open reduction and stable osteosynthesis with early rehabilitation as the elbow joint is prone for stiffness when immobilised [1,2].
The goal of restoring a painless and functional elbow, in a fractured distal humerus, requires anatomical re-construction and stable fixation. The distal humerus consists of an articular block, connected to the shaft with two pillars (medial and lateral pillar). The main principle of managing this fractures, is re-construction of the articular block and, stable internal fixation of this re-constructed block, with the shaft by plating on both pillars [3]. Without this dual plate arrangement, stability of fixation can be inadequate and this has been proven beyond doubt [4].
The management of distal humeral fractures are pertained to controversies. Few are correct approach, fixation techniques, management of ulnar nerve, role of total elbow arthroplasty and role of prophylactic therapy for heterotopic ossification. One of the prime controversy which, decides the outcome of this fractures, is the position of plates. Among the placement, the main debate is between the perpendicular plating proposed by, AO/ASIF group and, the principle based parallel plating by, O’ Driscoll. The standard method, before introduction of parallel plating and commonly used by most surgeons is to apply two plates perpendicular to each other [5].
The complications, like implant failure and malunion, accounting for 35% of cases, are reported in perpendicular technique, particularly in a patient with lower compliance, highly comminuted and osteoporotic fractures. Less number of screws, in distal lateral column, leads to loss of screw purchase, with resultant instability at both columns, and causing non-union at supra condylar level [6].
In order, to obtain a more stable initial fixation, particularly in osteoporotic bone, parallel plating has been introduced with the concept, that the screws will interdigitate within the distal fracture fragments (adjacent to the opposing plate) and form the equivalent of a compression arch [7,8]. Biomechanical comparison studies concluded that, parallel system under physiological loads provided, significantly higher stability in terms of stiffness, and resistance to plastic deformation under axial loading, as well as a tendency for a higher stiffness under torsion [9]. The authors, who are in favour of perpendicular plating, argue that extensive soft tissue stripping in parallel plating technique may cause non-union. They further add, perpendicular technique requires less soft tissue dissection, technically easy and the reports of non-union, in this technique are stastically insignificant.
From biomechanical findings, Korner et al., concluded that the implant configuration is, more important than the implant type, in distal humeral osteosynthesis [6]. Although, parallel plating is a more superior construct than perpendicular plating, biomechanically, there is, no large group clinical studies that, have compared the two construct types.
This prospective randomised study was conducted to compare the clinical outcomes in terms of bone union, elbow function and complications following management of intra-articular distal humeral fractures by parallel or perpendicular plating techniques.
Materials and Methods
A prospective randomised study was conducted in Sawai Man Singh Medical College, Jaipur, India, between December 2009 to December 2011, in patients with distal humeral fractures who fulfilled the inclusion criteria. Randomisation was done using computer generated random numbers and were operated using perpendicular plating (Group A) and parallel plating (Group B).
Inclusion Criteria
Intra-articular fractures of distal humerus, closed fractures of < three-week-old, skeletally mature and consenting to study.
Exclusion Criteria
With vascular injuries, open fractures, old distal humeral fractures (more than 2 weeks) and associated with ipsilateral, comminuted olecranon fractures extending into elbow joint.
Surgical Techniques
All patients were operated under general anesthesia with tourniquet control and in lateral position, with the involved limb supported over bolster. A midline posterior skin incision made, deep fascia incised, the ulnar nerve was identified, dissected out and retracted gently. Chevron ‘V’ shaped olecranon osteotomy [3,4,10] and paratricipital approach [11,12] were used. Various plates available like locking compression plates, 3.5mm reconstruction plates, one third tubular plates and pre contoured distal humeral plates were placed and fixed in 90-90 plating technique and in parallel plating method.
In perpendicular plating as proposed by AO-ASIF group, reconstruction of distal articular fragments were done and fixed with canulated screws and were fixed to the columns using two plates one on the posterolateral column and another on the medial ridge [5]. In parallel plating as proposed by O’Driscoll principles, the distal articular fragments were reduced, fixed and supracondylar compression with the medial and lateral columns were achieved using two plates placed on both ridges of medial and lateral side using the standard fixation steps described [3].
After fixing the fracture segments, Tension Band Wiring (TBW) of osteotomized olecranon was carried out. Meticulous repair of soft tissues was done in layers.
Postoperative Care and Follow Up
Active and passive mobilization of elbow were allowed immediately after surgery but weight bearing avoided for 6 weeks. The stitches, were removed at 2nd week, and at the end of 6th week, the light weight lifting was allowed. By the end of 3 months we ensured that full range of movements was there in elbow and shoulder and at 6 months patients were allowed to their routine full activities. If postoperative motion failed to progress as expected, a program of patient-adjusted static flexion and extension splints were implemented as soon as the soft tissues heals. At each follow up patients were evaluated clinically and radiologically for union, and the outcomes were measured in terms of Mayo Elbow Performance Score (MEPS) consisting of pain intensity, range of motion, stability and function. MEP score greater than 90 is considered excellent; Score 75 to 89 is good; Score 60 to 74 is fair and Score less than 60 is poor.
Results
A total of 38 patients, 20 in perpendicular plating group (group A) and 18 in parallel plating group (group B), were included in the study. The mean age of group A was 44.80±12.84 years (range- 22 to 65 years) and the mean age of group B was 40.17±16.42 years (range- 18 to 65 years) There were 27 males (group A-14; group B-13) and 11 females (group A-6; group B-5) in our study [Table/Fig-1].
Demographic distribution between two groups with respect to various category.
| Category | Group-A | Group-B |
|---|
| Total Number of Patients | 20 | 18 |
| Gender DistributionMale; Female | 14;6 | 13;5 |
| Age Distribution≤ 40; >40 (in years) | 9;11 | 11;7 |
| Mode of InjuryRoad Traffic Accident; Fall from Height; Fall from Standing Heights; Others | 11;3;6;0 | 15;0;2;1 |
| LateralityLeft; Right | 12;8 | 14;4 |
| Associated InjuryPresent; Absent | 6;14 | 2;16 |
| Type of FractureC1:C2:C3 | 7:8:5 | 10:6:2 |
| Delay in SurgeryMean±SD (In days) | 4.00±1.64(2-7) | 3.78±1.35(2-6) |
These patients were followed upto a minimum of one year and analysis showed almost equal amount of range of movements, time taken for bone union between the two groups. MEPS score was 88.25 in group A and 93.61 in group B, which was stastically non-significant [Table/Fig-2]. Outcome results were excellent to fair, but there were no poor results in our study [Table/Fig-3].
Various categories in the follow up periods.
| Category | Group-A(Mean±SD) | Group-B(Mean±SD) | p-value | Significance |
|---|
| Follow up(in months) | 13.70±4.39 | 12.39±1.97 | > 0.05 | NS |
| Time for Bone Union (in weeks) | 18.21±2.74 | 17.67±2.51 | > 0.05 | NS |
| Flexion (Degree) | 108.25±11.54 | 115.00±10.13 | > 0.05 | NS |
| Extension Lag (Degree) | 19.41±6.15 | 17.31±4.64 | > 0.05 | NS |
| Arc of Motion (Degree) | 94.75±22.00 | 105.83±15.39 | > 0.05 | NS |
| MEPS | 88.25±11.76 | 93.61±10.51 | > 0.05 | NS |
*(NS-Non significant).
Distribution of outcome of Group-A & Group-B subjects.
| Result | Group A | Group B |
|---|
| n (%) | n (%) |
|---|
| Good & Fair | 5(25.00) | 5(27.78) |
| Excellent | 15(75.00) | 13(72.22) |
χ2 = 0.030; d.f.= 1; p > 0.05; Not Significant.
Two patients in each groups had complications in the form of radial nerve paresis, ulnar nerve paresis, Sudeck’s dystrophy, infection and aseptic excoriation of skin by implant and arthrofibrosis [Table/Fig-4]. In our series analysis, we found that, the age of the patient had no effect on the ultimate outcome [Table/Fig-5]. Distribution of outcome according to type of fracture is shown in [Table/Fig-6] indicating that there is not much difference in various type of fractures outcome.
Distribution of complications of group-A & group-B subjects.
| Complication | Group A | Group B |
|---|
| n (%) | n (%) |
|---|
| Present | 2(10.00) | 2(11.11) |
| Absent | 18(90.00) | 16(88.89) |
χ2 = 0.175; d.f.= 1; p > 0.05; Not Significant.
Distribution of outcome according to age of Group-A & Group-B subjects.
| Result | Group-A(n=20) | Group-B(n=18) |
|---|
| ≤ 40 yrs | >40 yrs | ≤ 40 yrs | >40 yrs |
|---|
| Good & Fair | 2(10.00) | 3(15.00) | 1(5.56) | 4(22.22) |
| Excellent | 7(35.00) | 8(40.00) | 10(55.56) | 3(16.67) |
χ2 = 1.003; d.f.= 1; p >0.05; NS
χ2 = 2.460; d.f.= 1; p >0.05; NS
Distribution of outcome according to type of fracture of Group-A & Group-B.
| Type of fracture | Group-A (n=20) | Group-B (n=18) |
|---|
| Good & Fair(%) | Excellent(%) | Total | Good & Fair(%) | Excellent(%) | Total |
|---|
| C1 | 0(0.00) | 7(35.00) | 7(35.00) | 3(16.67) | 7(38.89) | 10(55.56) |
| C2 | 2(10.00) | 6(30.00) | 8(40.00) | 1(5.56) | 5(27.78) | 6(33.33) |
| C3 | 3(15.00) | 2(10.00) | 5(25.00) | 1(5.56) | 1(5.56) | 2(11.11) |
Discussion
Many biomechanical studies have projected parallel plating to be superior to the age old perpendicular plating technique [13]. However, Schwartz et al., found no significant differences [8]. The range of motion in the study [Table/Fig-2] were comparable to the study conducted by Doornberg et al., Shin et al., Aslam et al., and Pajarinen et al., they reported, 103 to 112 degrees range of motion regardless of the plate position [14–17]. To achieve a functionally useful elbow early rehabilitation has to be started, as elbow is prone for stiffness. Except, for few cases in our series, we followed, the same early rehabilitation schedule in both groups. Patients were educated about the importance of rehabilitation and were followed-up regularly. Most patients followed the regimen, but few because of pain didn’t work up properly and these patients, were managed by injecting intra-articular steroid and lignocaine. By achieving pain relief and gaining confidence of the patient, we were able to improve the motion of the elbow.
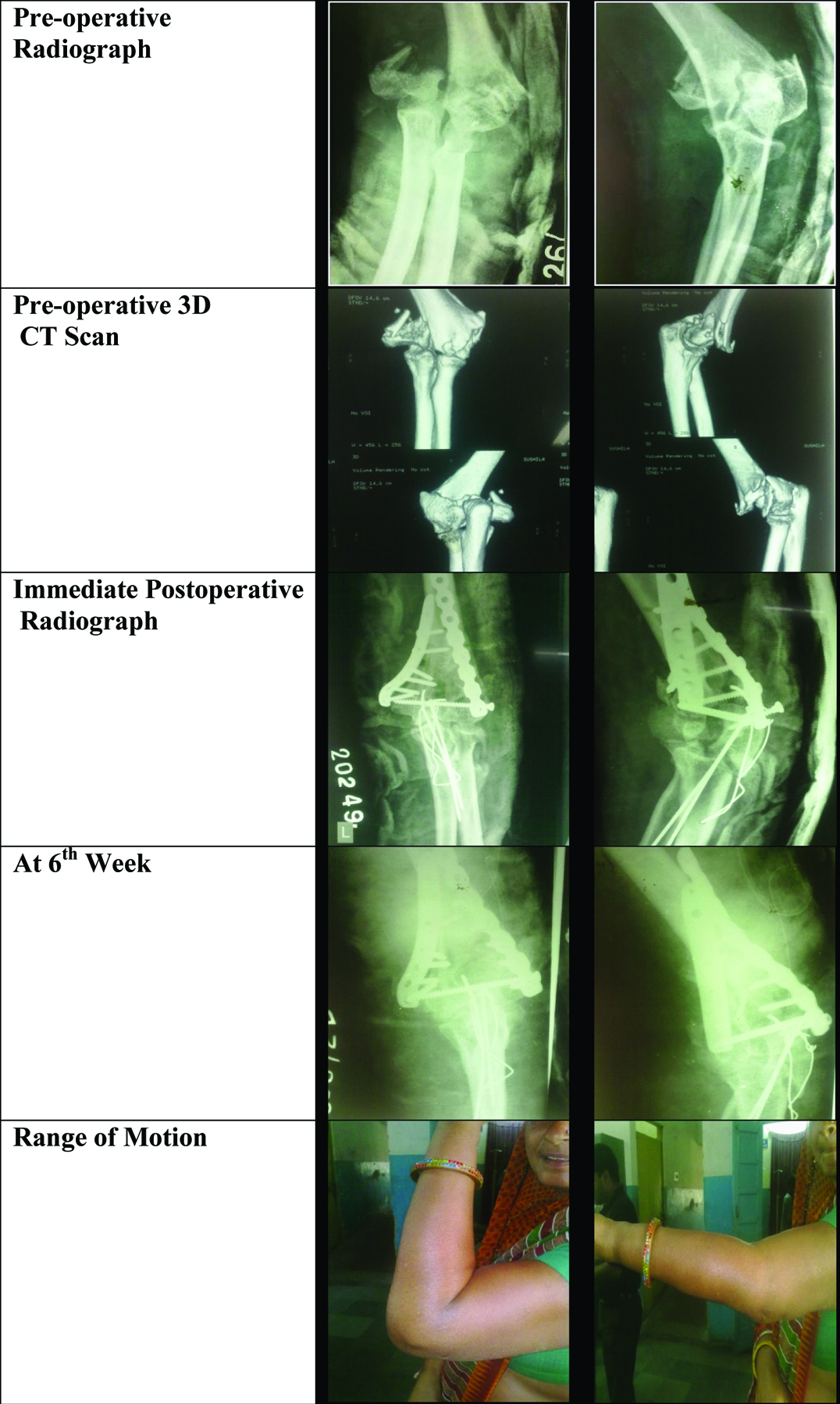
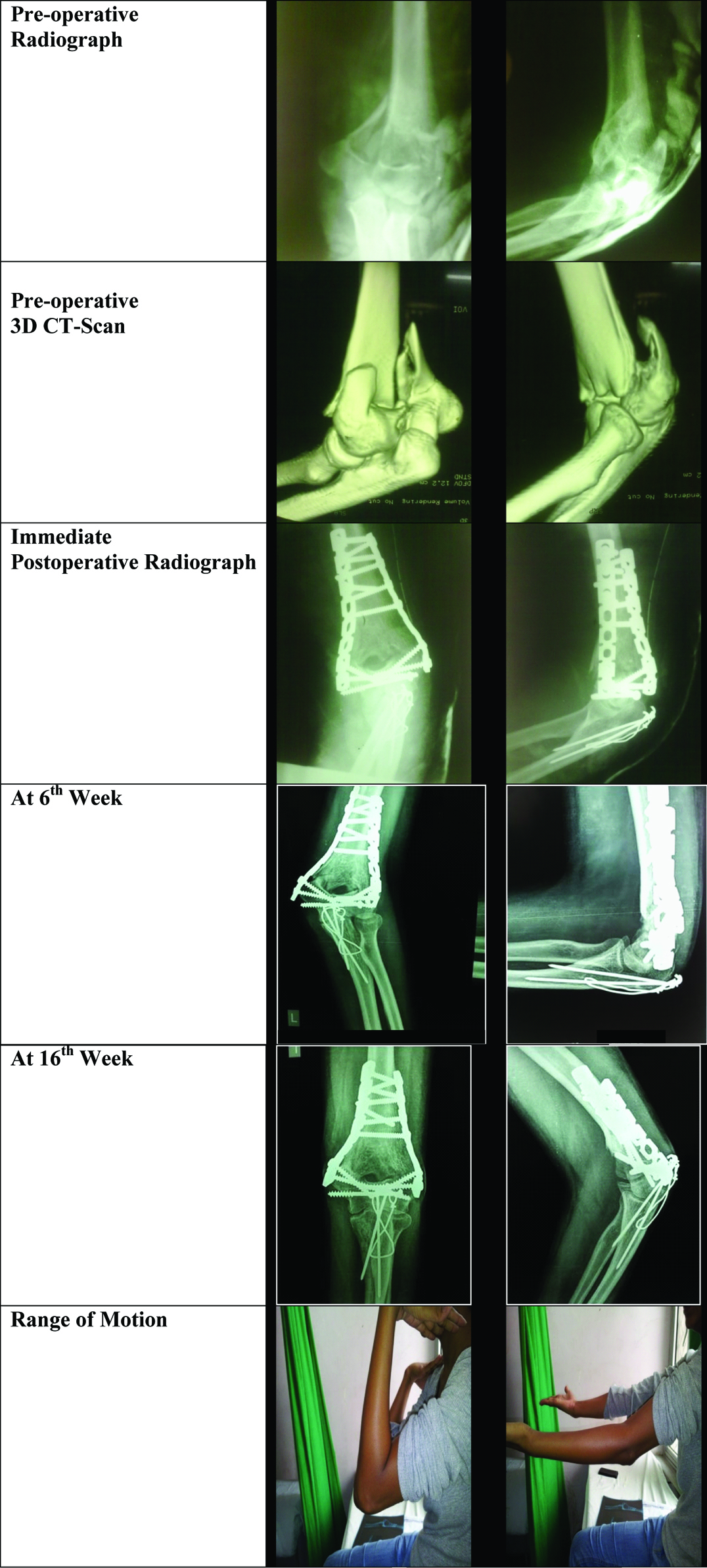
We achieved bone union in at an average of 18.21 weeks in group A and at 17.67 weeks in group B. The various clinical, radiological and post operative pictures are shown for both the intervention groups [Table/Fig-7,8]. All fractures united without implant failure, in both groups. We did not encounter non-union in osteotomy site of both groups, as well. Shin et al., reported a case of non-union in perpendicular plating group, which he managed by parallel plating and bone grafting. He reported, less number of screws in lateral column, to be the cause of implant failure and consequent non-union in their non-union case [15]. In our series of perpendicular plating, we didn’t have even a single case of implant failure and non-union.
Clinical pictures of a patient with perpendicular plating intervention.
Clinical pictures of a patient treated with parallel plating.
Surgical treatment of these fractures, in elderly patients is challenging, because of the likelihood of osteopenia, comminution, and poor general health. We had equally comparable results in old age patients as well and we support the view of Jupiter et al., [4], Srinivasan et al., [18] that age is not a contradiction for surgical fixation provided, the surgeons adhere to basic surgical and fixation principles. To achieve a stable fixation in these osteoporotic fractures, use a locking compression plate like fractures of other sites.
The most common complication, we encountered was arthrofibrosis, while ulnar nerve paresis was found common by Sang-Jin Shin et al., [15]. Two patients in group A and one in group B had arthrofibrosis. These patients were managed by arthrolysis, and we gained only few improvements in arc of motion. One patient in group A had radial nerve palsy, and another had Sudeck’s dystrophy. Radial nerve palsy recovered in one month, as it was due to traction paresis, during which he was given splint for nerve paresis. One patient in group B had aseptic excoriation of skin on medial side by implant, at the end of first year follow up. We managed this condition, by removal of all implants, as the fracture was united completely. We did ulnar nerve neurolysis along with this procedure, as patient had paresthetic sensation in little finger, which was recovered. Infection occurred in one patient of group B, which was managed initially with antibiotics and debridement till bony union. The implant was removed after bony union. We didn’t encounter heterotopic ossification, which was encountered in other series. This is due to timely surgical intervention after injury and proper soft tissue handling. We didn’t carry out any prophylactic measures for heterotopic ossification.
To summarise, parallel plating is more biomechanically stable than perpendicular plating technique, as it provides more screw purchase in distal fragment, and a rigid interlocking construct. Thus, it is more useful in low fracture patterns, comminuted, and osteoporotic bones. The perpendicular plating technique, requires less soft tissue dissection and time duration, and it is technically less demanding one. It is more useful in anterior shear fracture and one with coronal comminution. Though, perpendicular plating provides less stability when compared to parallel plating, the stability achieved by this technique is sufficient enough for bone union and early rehabilitation. This is well proved by no differences in bone union rates, movements of elbow, and MEP score.
Conclusion
Neither of the plating techniques are superior to the other and when a distal humerus fracture, fixed properly with suitable plates, both plating techniques provides an adequate stability for bone union and early rehabilitation. The position of plates, is to be decided by surgeons choice and the fracture pattern and he should have open minds to switch between two techniques.
*(NS-Non significant).
χ2 = 0.030; d.f.= 1; p > 0.05; Not Significant.
χ2 = 0.175; d.f.= 1; p > 0.05; Not Significant.
χ2 = 1.003; d.f.= 1; p >0.05; NS
χ2 = 2.460; d.f.= 1; p >0.05; NS
[1]. McKee MD, Wilson TL, Winston L, Schemitsch EH, Richards RR, Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approachJ Bone Joint Surg Am 2000 82:1701-07. [Google Scholar]
[2]. Pollock JW, Faber KJ, Athwal GS, Distal humerus fracturesOrthop Clin North Am 2008 39(2):187-200. [Google Scholar]
[3]. Sanchez-Sotelo J, Torchia ME, O’Driscoll SW, Principle-based internal fixation of distal humerus fracturesTech Hand Up Extrem Surg 2001 5:179-87. [Google Scholar]
[4]. Ring D, Jupiter JB, Fractures of the distal humerusOrthop Clin North Am 2000 31:103-13. [Google Scholar]
[5]. Bonczar M, Rikli D, Ring D. Distal humerus 13-C1 Open reduction; perpendicular (biplanar) plating (cited 2016) available from: https://www2.aofoundation.org/wps/portal/surgery?showPage=redfix&bone=Humerus&segment=Distal&classification=13-C1&treatment=&method=ORIF&implantstype=Open%20reduction;%20perpendicular%20(biplanar)%20plating&approach=&redfix_url=1285238780070&Language=en [Google Scholar]
[6]. Korner J, Diederichs G, Arzdorf M, Lill H, Josten C, Schneider E, Biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction platesJ Orthop Trauma 2004 18:286-93. [Google Scholar]
[7]. O’Driscoll SW, Sanchez-Sotelo J, Torchia ME, Management of the smashed distal humerusOrthop Clin North Am 2002 33:19-33. [Google Scholar]
[8]. Schwartz A, Oka R, Odell T, Mahar A, Biomechanical comparison of two different periarticular plating systems for stabilization of complex distal humerus fracturesClin Biomech (Bristol, Avon) 2006 21:950-55. [Google Scholar]
[9]. Stoffel K, Cunneen S, Morgan R, Nicholls R, Stachowiak G, Comparative stability of perpendicular versus parallel double-locking plating systems in osteoporotic comminuted distal humerus fracturesJ Orthop Res 2008 26(6):778-84. [Google Scholar]
[10]. Coles CP, Barei DP, Sean E, Nork SE, Taitsman LA, Hanel DP, The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerusJ Orthop Trauma 2006 20:164-71. [Google Scholar]
[11]. Schildhauer TA, Nork SE, Mills WJ, Henley MB, Extensor mechanism-sparing paratricipital posterior approach to the distal humerusJ Orthop Trauma 2003 17:374-78. [Google Scholar]
[12]. Ali AM, Hassanin EY, El-Ganainy AE, Abd-Elmola T, Management of intercondylar fractures of the humerus using the extensor mechanism-sparing paratricipital posterior approachActa Orthop Belg 2008 74:747-52. [Google Scholar]
[13]. Self J, Viegas SF Jr, Buford WL, Patterson RM, A comparison of double-plate fixation methods for complex distal humerus fracturesJ Shoulder Elbow Surg 1995 4:10-16. [Google Scholar]
[14]. Doornberg J, Lindenhovius A, Kloen P, van Dijk CN, Zurakowski D, Ring D, Two and three-dimensional computed tomography for the classification and management of distal humeral fractures. Evaluation of reliability and diagnostic accuracyJ Bone Joint Surg Am 2006 88:1795-801. [Google Scholar]
[15]. Shin SJ, Sohn HS, Do NH, A clinical comparison of two different double plating methods for intraarticular distal humerus fracturesJ Shoulder Elbow Surg 2010 19:02-09. [Google Scholar]
[16]. Aslam N, Willett K, Functional outcome following internal fixation of intraarticular fractures of the distal humerus (AO type C)Acta Orthop Belg 2004 70(2):118-22. [Google Scholar]
[17]. Pajarinen J, Bjorkenheim JM, Operative treatment of type C intercondylar fractures of the distal humerus: results after a mean follow-up of 2 years in a series of 18 patientsJ Should Elbow Surg 2002 11:48-52. [Google Scholar]
[18]. Srinivasan K, Fractures of the distal humerus in the elderlyClin Orthop Relat Res 2005 434:222-30. [Google Scholar]