Azygous Vein Aneurysm (AVA): A Case Report
Charles Albert Tujo1, Robert A. Jesinger2
1 Medical Faculty, Department of Radiology, David Grant Medical Center, Uniformed Services University, California, United States.
2 Medical Faculty, Department of Radiology, David Grant Medical Center, Uniformed Services University, California, United States.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Robert A. Jesinger, 60MDTS/SGQX-Radiology, 101 Bodin Circle, Travis AFB, 94535, California, United States.
E-mail: robert.jesinger@us.af.mil
Azygous Vein Aneurysm (AVAs) is an uncommon cause of mediastinal mass. They are typically asymptomatic and do not commonly require treatment. They may mimic mediastinal adenopathy on chest radiographs. We present a case of AVAs found during evaluation of chest pain in a patient who was also found to have pulmonary thromboembolism. The mass was worked up with cross-sectional imaging techniques using both Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI) and ultimately Positron Emission Tomography (PET). Due to recurrent symptomatology, the aneurysm was coiled.
Chest mass, Middle mediastinal mass, Vascular mass, Venous aneurysm
Case Report
A 70-year-old retired male physician presented to the Emergency Department with acute onset left sided chest pain for 1 day which started suddenly and progressively worsened. His symptoms evolved to include chest pain worsening with deep inspiration. He reported a history of hypertension and mild memory loss.
Initial vital signs were, afebrile with a pulse of 77 beats per minute, respiratory rate of 18 breaths per minute, pulse oximeter 96% on room air, and blood pressure 138/91 mmHg. Pain score was 3/10. Examination findings revealed normal heart and lung auscultation and no pitting oedema. Thoracic imaging was suggested in the workup of presumed pulmonary embolism.
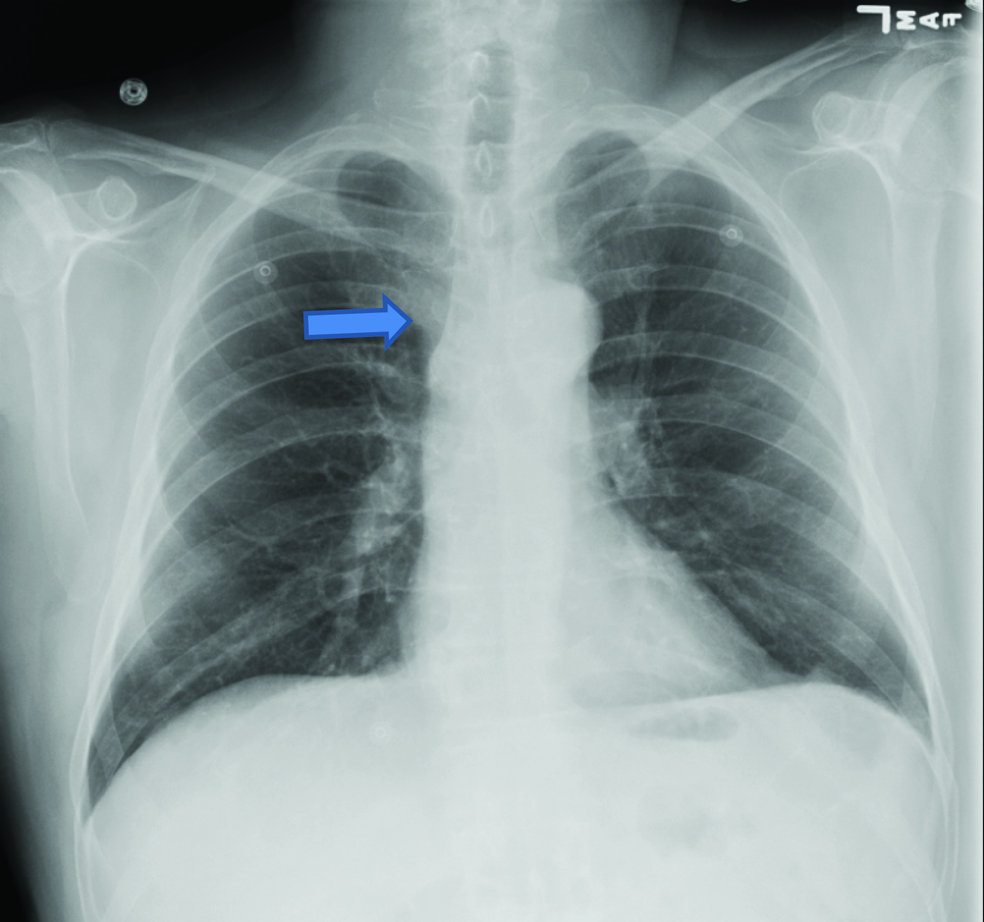
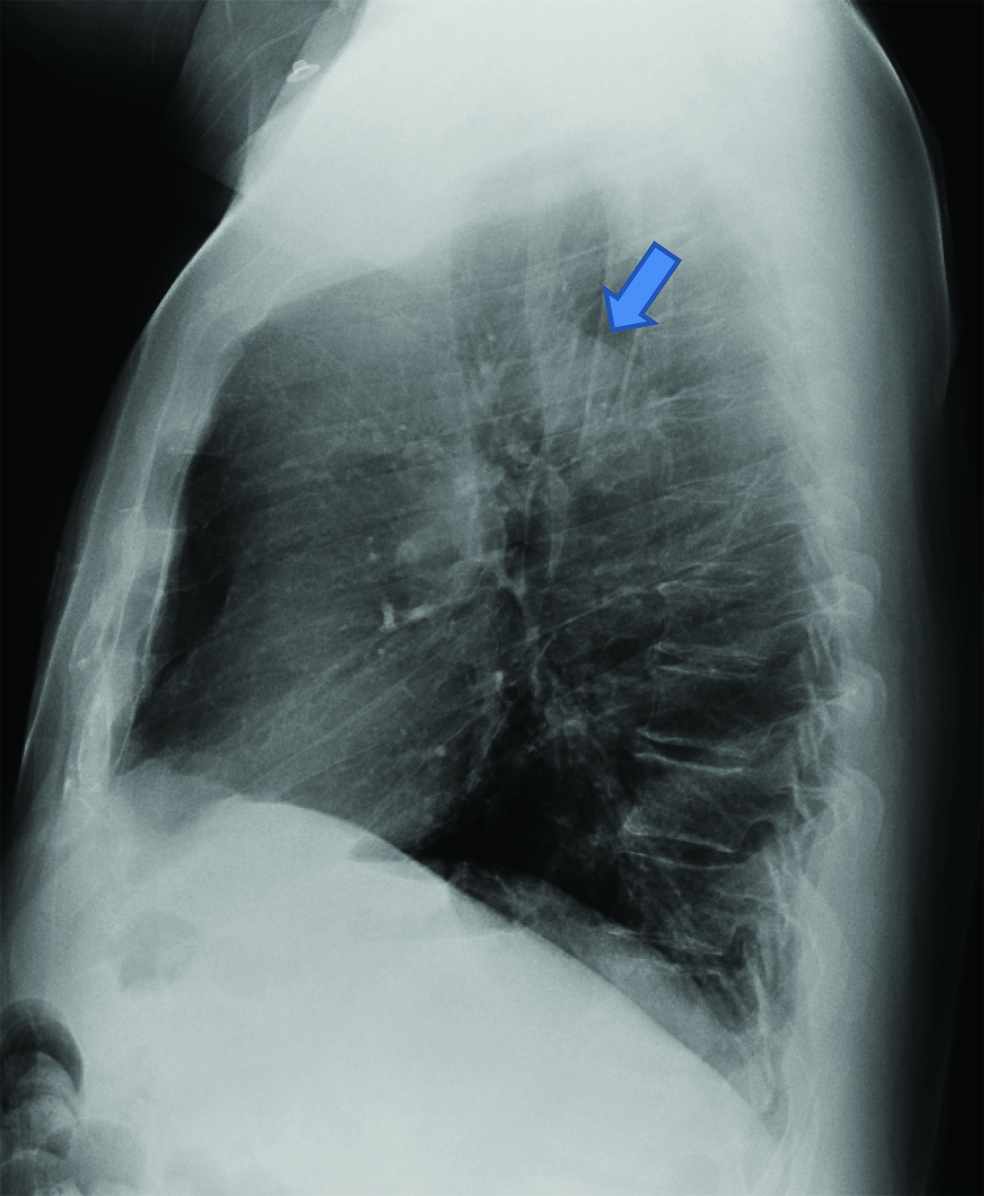
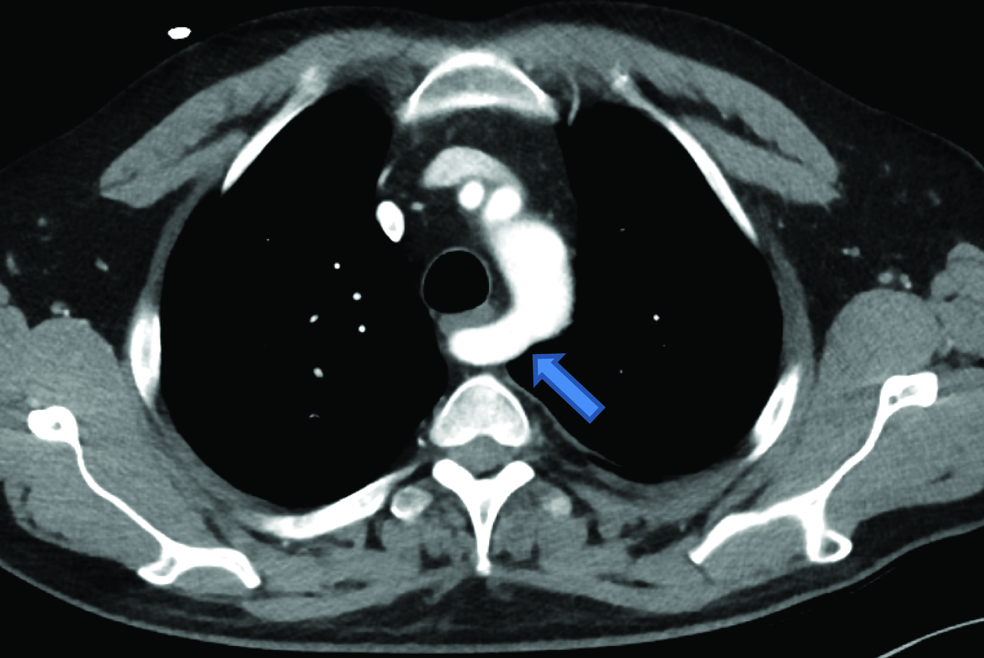
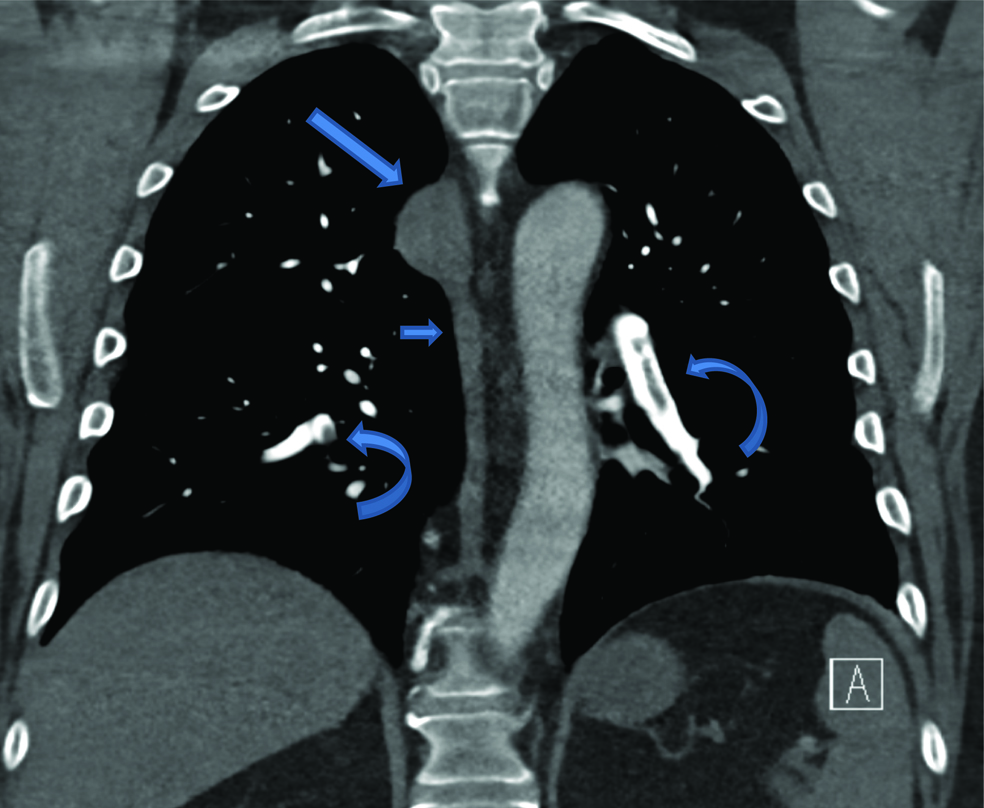
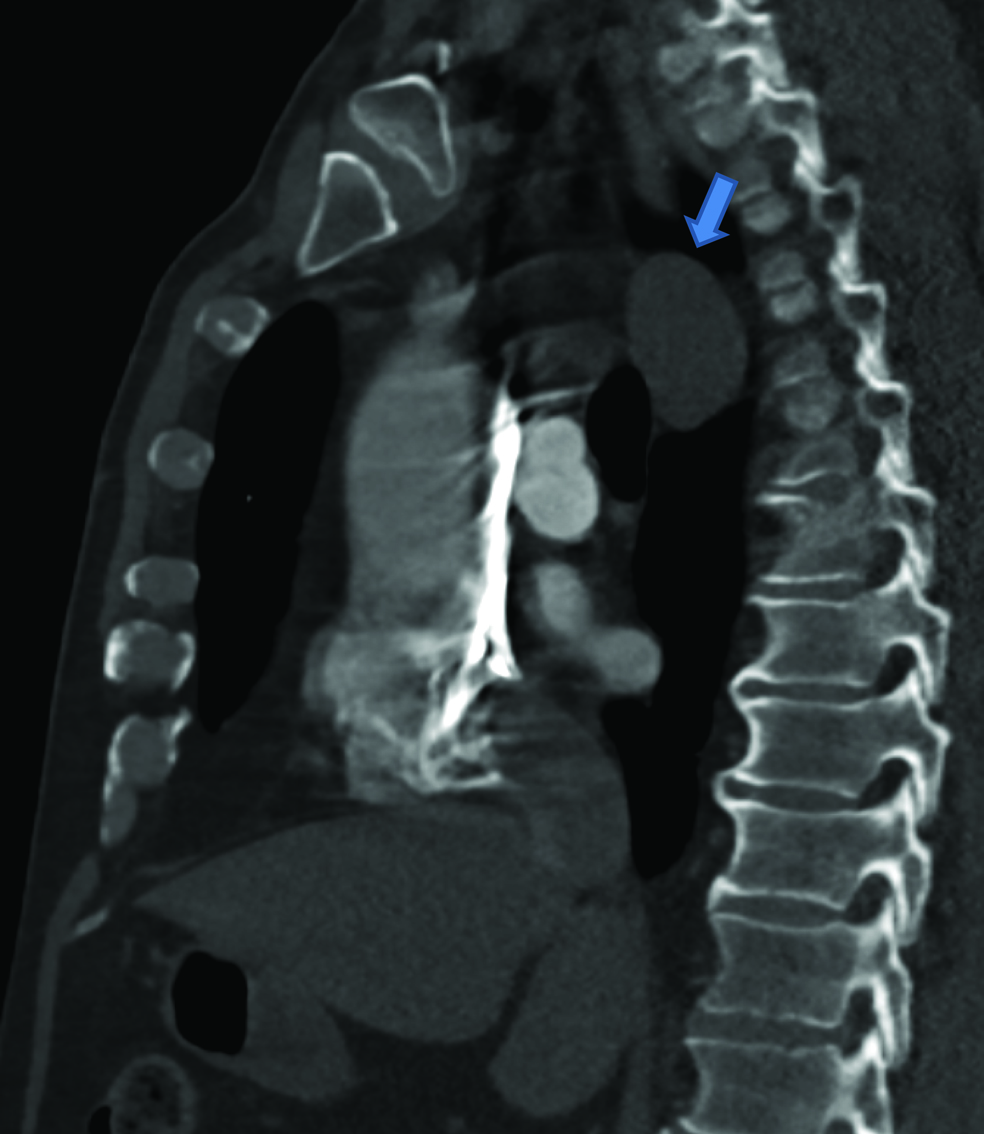
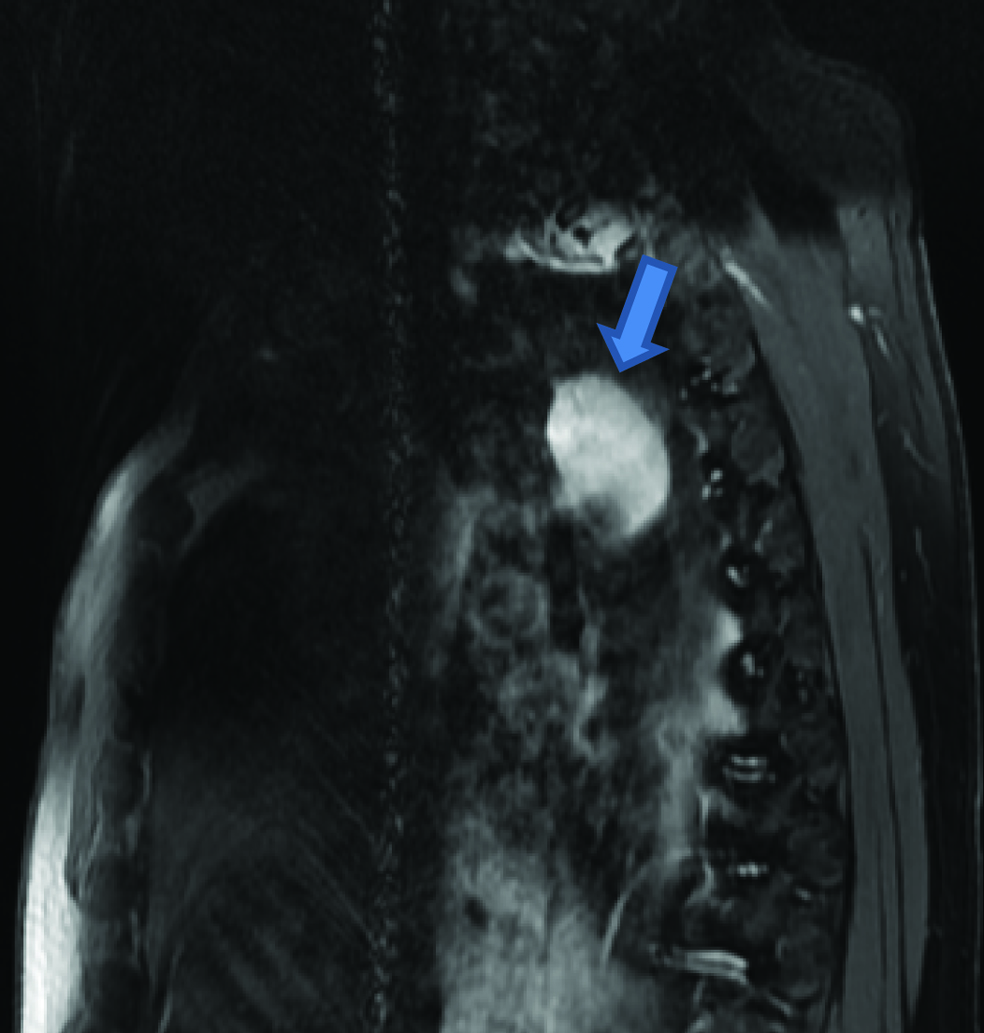
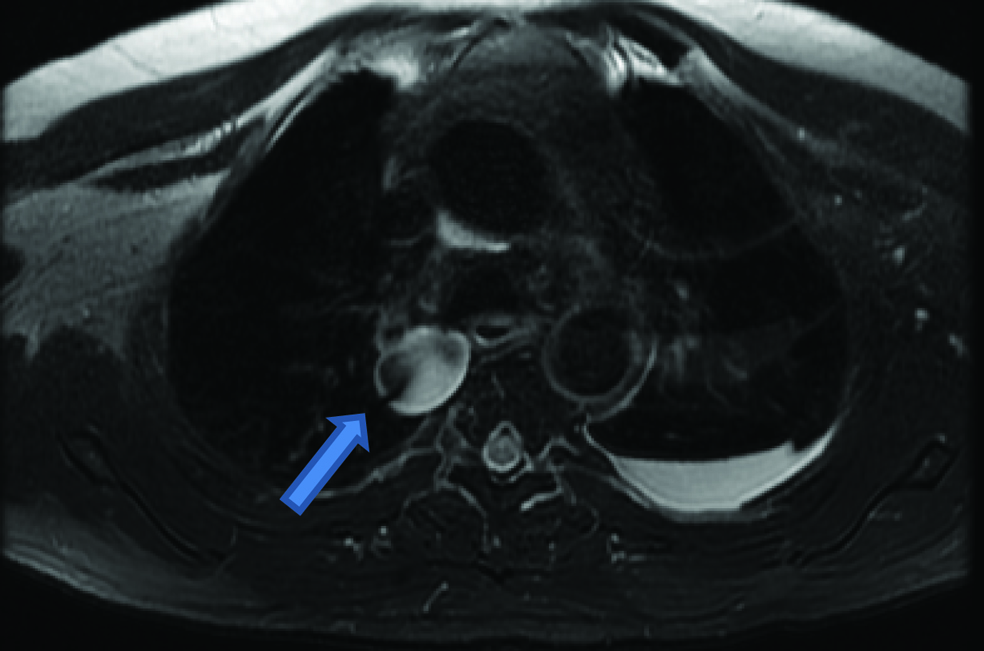
Radiographs of the chest were performed showing widening of the paratracheal stripe [Table/Fig-1] and prominent retrotracheal soft tissue density [Table/Fig-2]. Contrast-enhanced pulmonary arterial phase CT of the chest demonstrated acute bilateral pulmonary arterial emboli, a middle mediastinal mass, and an aberrant right subclavian artery [Table/Fig-3,4,5 and 6]. He was admitted for treatment of pulmonary thromboembolism, and a clinical evaluation for presumed malignancy (given mediastinal mass). An MRI was performed one day later [Table/Fig-7,8,9,10,11 and 12] to further characterize the mediastinal mass.
Frontal (PA view) chest radiograph, right paratracheal stripe thickening (arrow).
Lateral chest radiograph demonstrating increased density posterior to the trachea and above the level of the pulmonary arteries (arrow) which may in retrospect demonstrate increased density both correlating with the proximal descending aorta and a posterior mediastinal mass.
Enhanced axial CT (pulmonary arterial enhancement phase) through the level of the aortic arch demonstrates a mediastinal mass (thin arrow) contiguous with the azygous vein anteriorly. Filling defects in the pulmonary arterial system (thick arrow) represent acute pulmonary emboli (Left to Right)
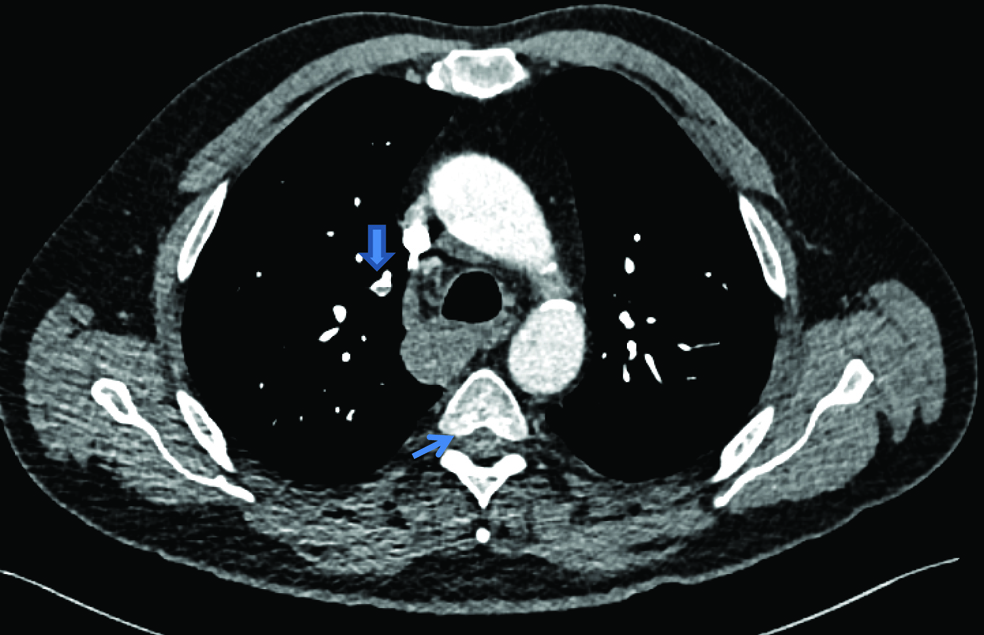
Enhanced axial CT through the level of the aorta demonstrates incidental identification of an aberrant right subclavian artery (arrow).
Enhanced coronal reconstructed CT of the chest demonstrating a homogenous well- circumscribed right middle mediastinal mass (long arrow) contiguous with and similar in density to the azygous vein inferiorly (short arrow). Pulmonary emboli are identified bilaterally (curved arrows).
Sagittal reconstructed post contrast image of the chest at the level of the ascending aorta demonstrates a middle mediastinal mass (arrow) that may correlate with the region of increased density seen in retrospect on the lateral chest X-Ray view [Table/Fig-1,2]. (Left to Right)
Sagittal T2w FS MR (1.5T) image demonstrates a high T2 signal mass that correlates with the CXR location of a region of increased density.
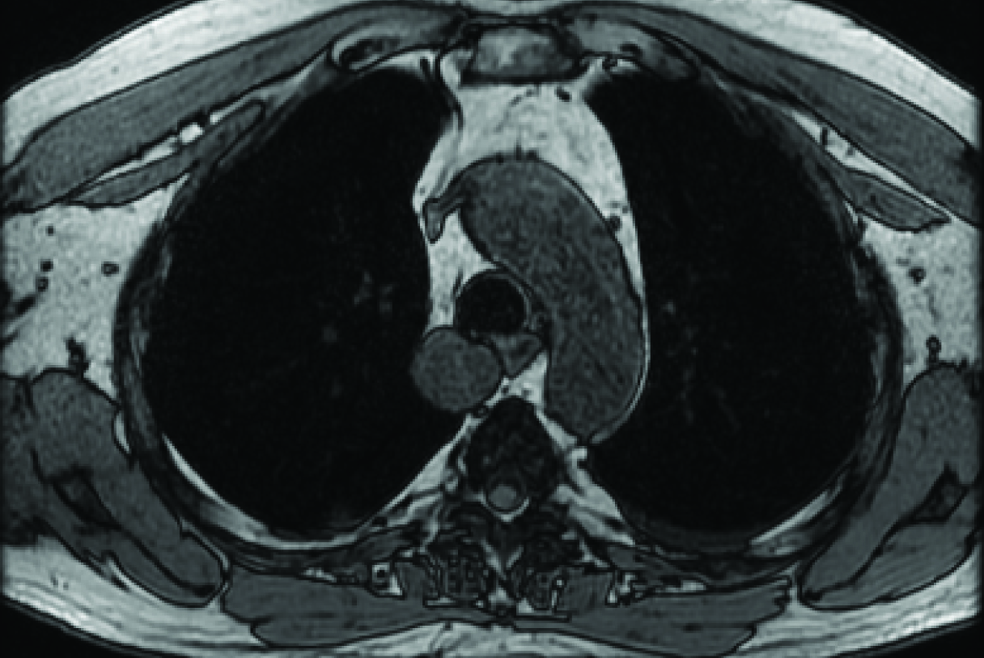
Axial T2w FIESTA (1.5 T) MR image demonstrating the mass to contain heterogeneous signal similar in intensity to a layering left pleural effusion. A linear low signal region in the mass is artifactual.
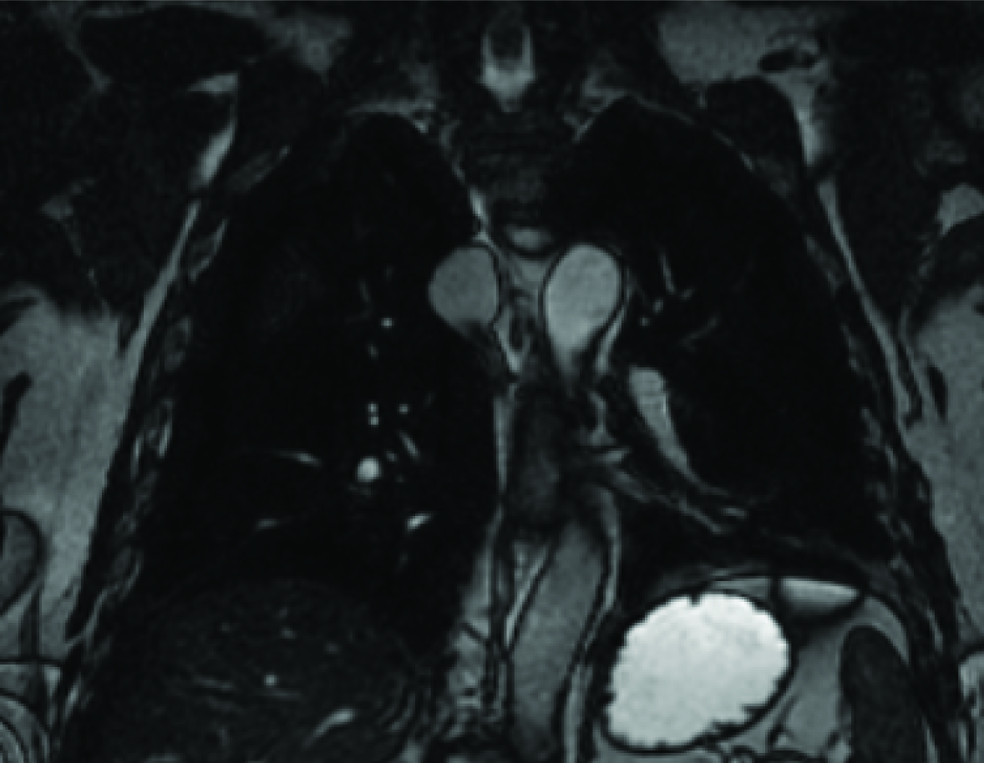
Coronal 2D FIESTA (1.5 T) MR image shows the mass to be contiguous with the azygos vein inferiorly. (Left to Right)
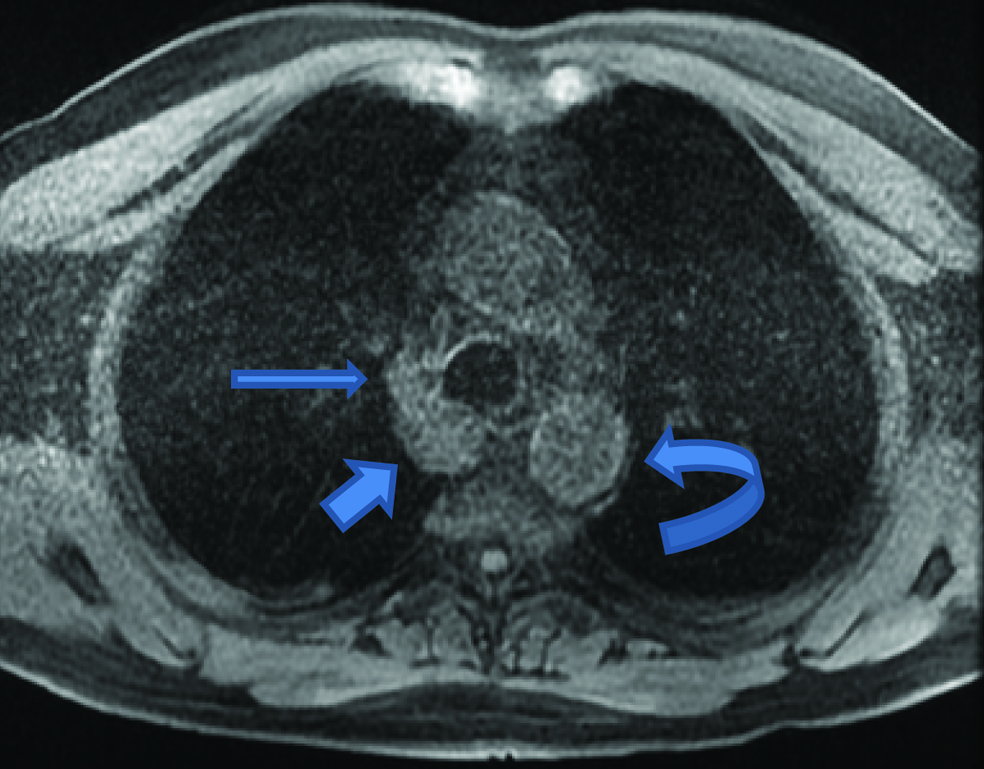
Axial T1w out-of-phase (1.5 T) MR image of the mass demonstrates its signal to be similar to the adjacent thoracic aorta.
Precontrast axial T1w FS LAVA (1.5 T) MR image demonstrates the mass (short arrow) to be contiguous with azygous vein anteriorly (long arrow) and similar in intensity to the aorta (curved arrow).
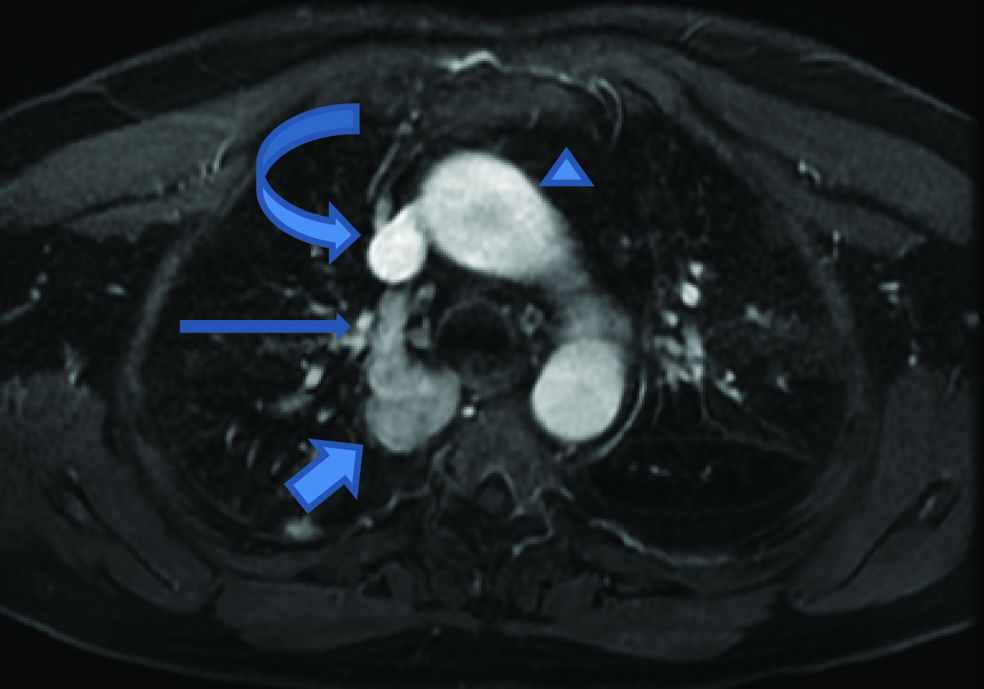
Post contrast axial T1w FS LAVA (1.5 T) MR image demonstrates contrast opacifying the mass (short arrow) of similar intensity to the azygos vein anteriorly (long arrow). The aorta (triangle) is of increased intensity as is the SVC (curved arrow). (Left to Right)
On the initial chest CT examination, the mediastinal mass measured 3.4 cm and was positioned adjacent to the azygous vein and located in the middle mediastinal space. The mass was homogeneous (49 HU) and non-calcified. On the initial CT, the azygous vein had a density of 53 HU superior to the mass and 24 HU inferior to the mass. Mild clot burden was seen in the pulmonary arteries, greatest in the right main pulmonary artery. No saddle embolus was seen, and there was no CT evidence of right heart strain. The lungs demonstrated tiny pleural effusions and basilar atelectasis. An aberrant right subclavian artery was present, but no adenopathy.
The chest MRI demonstrated a 3.3x2.6x3.9 cm enhancing vascular structure, inseparable from the adjacent azygous vein in the middle mediastinum, with signal characteristics compatible with a low-flow (venous) vascular structure.
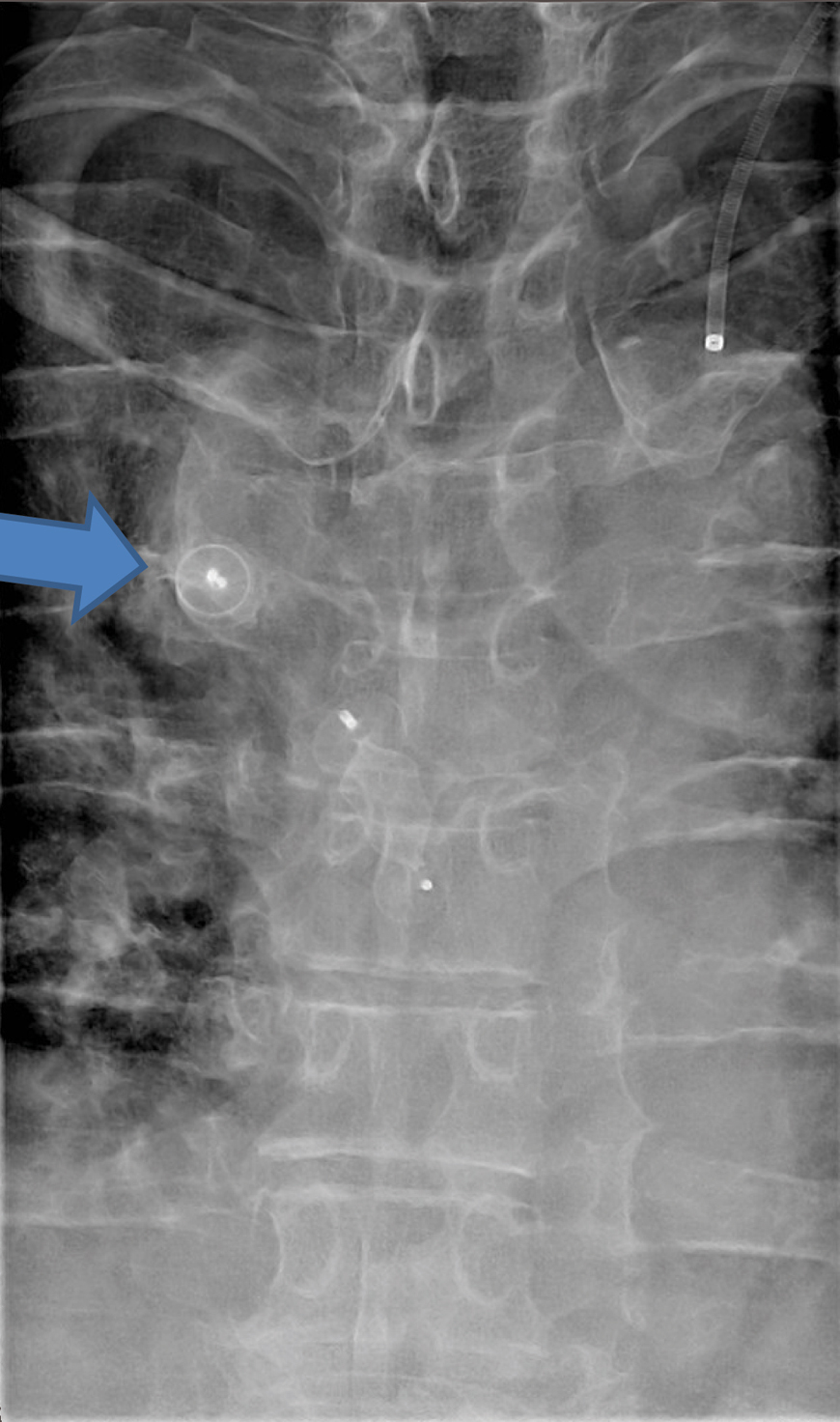
The patient was seen by a cardiothoracic vascular surgeon to decide if any intervention was warranted. He was discharged on apixaban oral anticoagulant 10 mg BID, as an outpatient, and after weighing the risks and benefits of anticoagulation vs. non-invasive intervention, he was proceeded for embolization. Interventional Radiologist successfully coiled the aneurysm with amplatzer devices [Table/Fig-13]. Follow up was planned in three months to monitor symptomatology and potentially discontinue anticoagulation.
AP fluoroscopically obtained view of the chest showing the amplatzer device (arrow) in the region of the azygous aneurysm.
Discussion
While middle mediastinal masses are frequently encountered during evaluation of chest radiographs and chest CT exams, few cases of AVA been clinically encountered or described in the literature [1]. In fact, AVA is a rare entity. The AVA in this case was thought to be an idiopathic incidentally-discovered congenital anomaly, perhaps made more visible by increased central venous pressure, as acute Pulmonary Thromboembolism (PE) serves as a marker for increased central venous pressure. It is difficult to determine whether the patient’s PE was due in part to the presence of AVA or developed due to increased central venous pressure as a result of the AVA. As the patient did not have a history of chronic PE, we favour the aneurysm being a congenital anomaly.
AVA is usually asymptomatic and identified serendipitously upon routine chest imaging [2]. The azygous vein can dilate temporarily, but commonly returns to normal size after events such as cardiac failure, portal hypertension, or pregnancy [3]. Acquired aneurysms may result from high blood flow possibly from collateral flow. The exact aetiology for a venous aneurysm is uncertain, though some researchers have postulated venous hypertension, inflammation, infection, congenital vein weakness, trauma, and hemodynamic changes (secondary to localized tissue degeneration) as possible theories. Most authors accept connective tissue loss in the venous media as contributing to the development of venous aneurysm [4]. Recently, research has identified focal structural changes in the venous wall that may be related to increased expression of select matrix metalloproteinases as contributing to aneurysm development [5].
Idiopathic aneurysms are rare [2]. Although usually asymptomatic they can exert mass effect on adjacent structures, predispose to pulmonary embolism and may grow. In a review of 10 cases, 2 cases were thought to have chest tightness related to aneurysm mass effect [2]. Presumably symptoms abated after surgical resection in both patients. While aneurysm enlargement and rupture would be a serious concern, there are no published reports of venous aneurysm rupture. Theoretical symptoms could relate to compression of the adjacent oesophagus, i.e., dysphagia or trachea, i.e., dyspnea [2]. Both complete and partial thrombosis has been reported, which could predispose to PE possibly due to turbulent flow dynamics within the AVA [3]. PE and thrombosis are not uncommonly cited in the literature to be attributed to AVA [3]. Initial diagnosis is by chest radiographs. Definitive diagnosis was usually accomplished with CT or MRI showing a right paratracheal mass along the course of the azygous vein that follows enhancement of the vein. A venous aneurysm is a focal region of venous dilation that communicates with an otherwise non-dilated vein through a single channel, in contradistinction to a varicose vein, which is diffusely enlarged (and often tortuous). Venous aneurysm has been defined as a short axis length of 2.5 times the normal diameter [2].
Mediastinal compartments have been radiologically divided into three compartments. The anterior mediastinum is bounded anteriorly by the posterior sternum and anterior pericardium posteriorly. The middle mediastinum lies between the anterior pericardium and the posterior pericardium. The posterior mediastinum is demarcated by the posterior pericardium to the ventral spine [6]. Based upon the three compartment model, the azygous aneurysm lies in the middle mediastinum.
Although, complications have been described such as mass effect and thrombosis, there is no universally accepted management strategy. Treatment options vary from surgical resection and embolization to conservative. The 10 case review report reported surgical resection in 5 of 10 [2]. Non-surgical management such as amplatzer vascular plugs have been utilized to thrombolyse the aneurysm with success [7]. Conventional and Video Assisted Thoracoscopic Surgery (VATS) was successfully used to resect an idiopathic aneurysm [1]. Despite many reports of AVA being excised or thrombolysed, they can safely be followed as proven in a 4 year survey of a patient followed with CT [8].
The patient described in this case report had PE, which could have been precipitated by the azygous aneurysm; however, no imaging evidence of thrombus in the venous aneurysm was found during evaluation. The aneurysm was ultimately coiled one month later and at the time of publication, the patient remained on anticoagulation, though the plan was to discontinue should symptoms improve.
Conclusion
This case describes a mediastinal mass visible on a chest radiograph (lateral view) and characterized on cross-sectional imaging as a 3.9 cm AVA, with MRI signal characteristics and enhancement similar to the adjacent azygous vein. The aneurysm was treated with coil embolization.
[1]. Ueda Y, Tokuno J, Shoji T, Huang C, An azygos vein aneurysm resected by video-assisted thoracic surgery after preoperative evaluation of multidetector computed tomographyInteractive Cardiovascular and Thoracic Surgery 2014 18:135-36. [Google Scholar]
[2]. Ko SF, Huang CC, Lin JW, Lu HI, Kung CT, Ng SH, Imaging features and outcomes in 10 cases of idiopathic azygos vein aneurysmAnnals of Thoracic Surgery 2014 97(3):873-78. [Google Scholar]
[3]. Miguel G, Mirapeix RM, Castaner E, Domingo Ch, Mata JM, Marin A, Idiopathic azygos vein aneurysm: a rare cause of mediastinal massThorax 1999 54:653-55. [Google Scholar]
[4]. Gabrielli R, Rosati MS, Siani A, Irace L, Management of symptomatic venous aneurysmScientific World Journal 2012 (2012)Article ID 386478 [Google Scholar]
[5]. Benjamin MM, Khalil RA, Matrix metalloproteinase inhibitors as investigative tools in the pathogenesis and management of vascular diseaseExs 2012 103:209-79. [Google Scholar]
[6]. Liu W, Deslauriers J, Mediastinal divisions and compartmentsThoracic Surgery Clinics 2011 21(2):183-90. [Google Scholar]
[7]. Weber H, Transcatheter occlusion of an azygous vein aneurysmCatheterization and Cardiovascular Interventions 2011 77:99-102. [Google Scholar]
[8]. Chiu HSS, Lau S, Kam CK, Azygous vein aneurysm CT scan follow-upJournal of Thoracic Imaging 2006 21:66-68. [Google Scholar]