Post Extubation Bronchospasm in an Undiagnosed Case of Ascariasis: Anaesthetic Challenges
Ravindra Gehlot1, Shekhar Suman Saxena2, Indira Kumari3, Virendra Verma4, Aditya Bidwaikar5
1 Assistant Professor, Department of Anaesthesia, RNT Medical College, Udaipur, Rajasthan, India.
2 Junior Registrar, Department of Anaesthesia, RNT Medical College, Udaipur, Rajasthan, India.
3 Professor, Department of Anaesthesia, RNT Medical College, Udaipur, Rajasthan, India.
4 Junior Registrar, Department of Anaesthesia, RNT Medical College, Udaipur, Rajasthan, India.
5 Junior Registrar, Department of Anaesthesia, RNT Medical College, Udaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shekhar Suman Saxena, Junior Registrar, Department of Anaesthesia, RNT Medical College, Udaipur-313001, Rajasthan, India.
E-mail: drshekharsuman3@gmail.com
One of the most prevalent parasitic infestation is ascariasis which poses a great challenge to both the person being infested with and the treating medical team. We present here a case of round worm (Ascaris lumbricoides) infestation. A 40-year-old male, weighing 60 kg, diagnosed as perforation peritonitis, was scheduled for emergency exploratory laparotomy. The round worm was crawling out from duodenal perforation vent during laparotomy confirming the infestation. Patient later developed bronchospasm in post-extubation period and was managed accordingly. Surprisingly the patient expelled an adult worm in the next morning. This report highlights the importance of anticipating complications (i.e., airway obstruction, bronchospasm, etc.,) in an undiagnosed case of round worm infestation, especially if routine investigations were within normal limits.
Airway obstruction, Laparotomy, Round worm
Case Report
A 40-year-old man reported to the emergency with sudden pain in abdomen early morning. Pain was generalized and increasing in severity. His personal and past history was insignificant with no history of Upper respiratory tract infection, asthma and chronic obstructive pulmonary disease. All routine investigations were within normal range. Quick pre anaesthetic examination was not significant. His vitals were B.P 130/88 mmHg, Pulse rate 98/min, Respiratory rate 20 min, SpO2 96% on air, without any significant auscultatory findings. Patient was taken in emergency operation theatre for exploratory laparotomy.
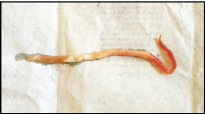
After securing two large bore 18G peripheral intravenous cannula and placement of nasogastric tube, routine premedication was given as per institutional protocol. General anaesthesia was then induced and maintained throughout the course. During exploration a small perforation (0.5 × 0.5 cm2) was found in the first part of the duodenum A live adult round worm [Table/Fig-1] came out through the perforation, which was stored in sample collection bottle and sent for microbiology department. Perforation was repaired and skin sutures were secured. After achieving adequate muscle power and respiration, patient was successfully extubated. While patient was still on O.T table, he developed sudden respiratory distress with RR 28/min, fall in saturation gradually till 80% with added expiratory wheeze. Bag and mask ventilation was done with 100% FiO2 but SpO2 further decreased to 60% with RR 40 per min, B.P 140/90 mmHg and PR 100/min. Patient was reintubated after giving propofol and supplemented with deriphyllin, hydrocortisone, dexamethasone intravenously. After ventilating with Bain’s circuit with 100% FiO2 gradually SpO2 increased till 90% and then patient was shifted to Surgical intensive care unit where he was given oxygen (FiO2 100%) through T piece. After half an hour he was able to maintain SpO2 to 98% (FiO2 40%), RR 16/min, B.P 120/76 mmHg, PR 78/min and bilateral equal air entry on auscultation with no added sounds. He was then extubated and watched for any other complications. In the morning next day patient expelled an adult Ascaris worm [Table/Fig-2] from his mouth, which was noticed by the patient’ attendant and the same was shown to on duty resident doctor in SICU following which no other complication occurred. On the first postoperative day he was given routine antibiotics, analgesic, fluids and anthelmintic drug (single dose of tab Albendazole 400 mg). He was later discharged on 7th post op day.
Worm came out from duodenal vent (in O.T).

Worm expelled from mouth (in SICU).
Discussion
Ascariasis is one of the most prevalent parasitic (Helminthic) infection worldwide (25% prevalence) [1], especially in developing countries with poor sanitation where it can prevail in 100% population [2]. The route of infection is fecooral, therefore more prevalent in areas with poor hygiene or sanitation and where feces are used as manure or as a fertilizer [1,3]. Studies conducted in children of rural and urban location in and around Chennai have reported the prevalence of intestinal parasitic diseases ranging from 60 to 91% among which A.lumbricoides was the most common helminthic parasite detected (52.8%) [4]. The worm can cause various complications during the perioperative phase like bronchospasm, respiratory obstruction, and pneumonitis depending on the developmental stage [5–9].
At this point of discussion we should know some differentiating morphological features between adult male and female worms. Adult male worm being more slender (with incurved tail), while female being as thick as pencil. The male being 15-25 cm in length and 3-5 mm in diameter while female being 20-35 cm in length and 5-6 mm in diameter [2,3]. So in our case the worm is an adult male.
The worm can cause several complications during perioperative period depending upon the stage of development. The larval stage leading to Loeffler’s syndrome and adult stage leading to erratic Ascariasis.
The Loeffler’s syndrome or pulmonary Ascariasis [10], occurs during migration of worm through lungs during larval stage. It is a self-limiting disease with respiratory symptoms like wheeze and cough which resolves within 2-3 weeks. The symptoms are associated with eosinophilia and need symptomatic treatment including bronchodilators and steroids. Anthelmintic therapy [11] is not advocated because dying larvae may do more harm than migrating ones.
Adult worm may lead to several complications including intestinal obstruction, appendicitis, obstructive jaundice and pancreatitis. May travel to lungs and cause hypersensitivity or inflammatory reaction. Adult worm can also migrate to oral cavity and upper airway leading to life-threatening complications in perioperative period like airway obstruction; endotracheal tube obstruction, bronchospasm and even a case of respiratory arrest have been reported [6–9,12]. There are various factors under anaesthesia that influence migration of worm [2], these may be provocation by anaesthetic drugs, supine position during anaesthesia, relaxed cardio-oesophageal sphincter, absence of swallowing reflex, decreased release of gastric HCL and pepsin. Only under these circumstances the parasite can reach the oral cavity [13].
In our case the post extubation findings were suggestive of bronchospasm which may be either due to hypersensitivity reaction or due to airway obstruction.
The bronchospasm due to the hypersensitivity reaction usually occurs in larval stage of infestation with associated eosinophilia presenting as Loeffler’s syndrome. Thus, it is excluded as the primary cause because the patient did not have eosinophilia and the worm was adult.
We may suspect the primary cause of post-extubation bronchospasm due to erratic ascariasis because of following reasons: The worm was adult; it may have crawled in upper airway due to provoking factors; Worm may have gone in oesophagus during reintubation and patient expelled an adult worm in the next morning.
Conclusion
Our case report highlights the consideration of anticipating Ascariasis in patients with intestinal obstruction or perforation due to the potential problems which may occur later. Stool examination and quantification of worm burden should be done. Keeping in mind the possibility of Ascariasis in these patients, one should also be prepared for the management of unanticipated complications (like hypersensitivity, airway obstruction, bronchospasm and even respiratory arrest) which may occur during post-extubation period.
[1]. Ramamoorthy K G, Anaesthesia and Ascaris pneumonia (Loeffler’s syndrome)Indian J Anaesth 2015 59(2):125-26. [Google Scholar]
[2]. Markel EK, Voge M, John DT, Medical parasitology 1992 7th EdPhiladelphiaWB Saunders:262-68. [Google Scholar]
[3]. Yilmaz H, Türkdoan MK, Akdeniz H, Kati Demiroz AP, Ascaris lumbricoides in the oral cavity: A case reportEastern Journal of Medicine 1983 3(2):75-6. [Google Scholar]
[4]. Fernandez MC, Verghese S, Bhuvaneswari R, Elizabeth SJ, Mathew T, Anitha A, A comparative study of the intestinal parasites prevalent among children living in rural and urban settings in and around ChennaiJournal of Communicable Diseases 2002 34(1):35-39. [Google Scholar]
[5]. Acar A, Oncül O, Cavuslu S, Okutan O, Kartaloglu Z, Case report: Löffler’s syndrome due to Ascaris lumbricoides mimicking acute bacterial community - Acquired pneumoniaTurkiye Parazitol Derg 2009 33:239-41. [Google Scholar]
[6]. Bailey JK, Warner P, Respiratory arrest from Ascaris lumbricoidesPediatrics 2010 126:e712-15. [Google Scholar]
[7]. Faraj JH, Upper airway obstruction by Ascaris wormCan J Anaesth 1993 40:471 [Google Scholar]
[8]. Singh R, Garg C, Vajifdar H, Near fatal respiratory obstruction due to Ascaris lumbricoidesTrop Doct 2005 35:185 [Google Scholar]
[9]. Ugras SK, Finley DJ, Salemi A, Ascaris lumbricoides infection causing respiratory distress after coronary artery bypass graftingSurg Infect Larchmt 2010 11:177-78. [Google Scholar]
[10]. Phanichyakarn P, Direkwattanachai C, Na Ayuthya PI, Loeffler’s syndrome: Report of two casesRamathibodi Med J 1979 2:147-51. [Google Scholar]
[11]. Warren KS, Mahmoud AA, Algorithms in the diagnosis and management of exotic diseases. xxii. Ascariasis and toxocariasisJ Infect Dis 1977 135:868-72. [Google Scholar]
[12]. Bharati SJ, Chowdhury T, Goyal K, Anandani J, Airway obstruction by round worm in mechanically ventilated patient: An unusual causeIndian J Anaesth 2011 55:637-38. [Google Scholar]
[13]. Christopher F, James CF, Pulmonary aspiration of gastric contents in: Gravenstein N, Kirby RRComplications in Anaesthesiology 1996 2nd EdPhiladelphiaLippicatt-Raven:184 [Google Scholar]