Acute Total Lung Collapse in a Woman with Acute Stroke and Atrial Fibrillation
Karanam Gowrinath1, Gangapatnam Vamsidhar Reddy2
1 Senior Consultant, Department of Pulmonary Medicine, Apollo Speciality Hospital, Nellore, Andhra Pradesh, India.
2 Consultant, Department of Anaesthesiology, Apollo Speciality Hospital, Nellore, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Karanam Gowrinath, 103, Bhavanipark Centra Apartments, 9th Street, Ramjinagar, Nellore-524002, Andhra Pradesh, India.
E-mail: drkgowrinath@gmail.com
Bronchoscopy, Hemithorax, Mucous plug
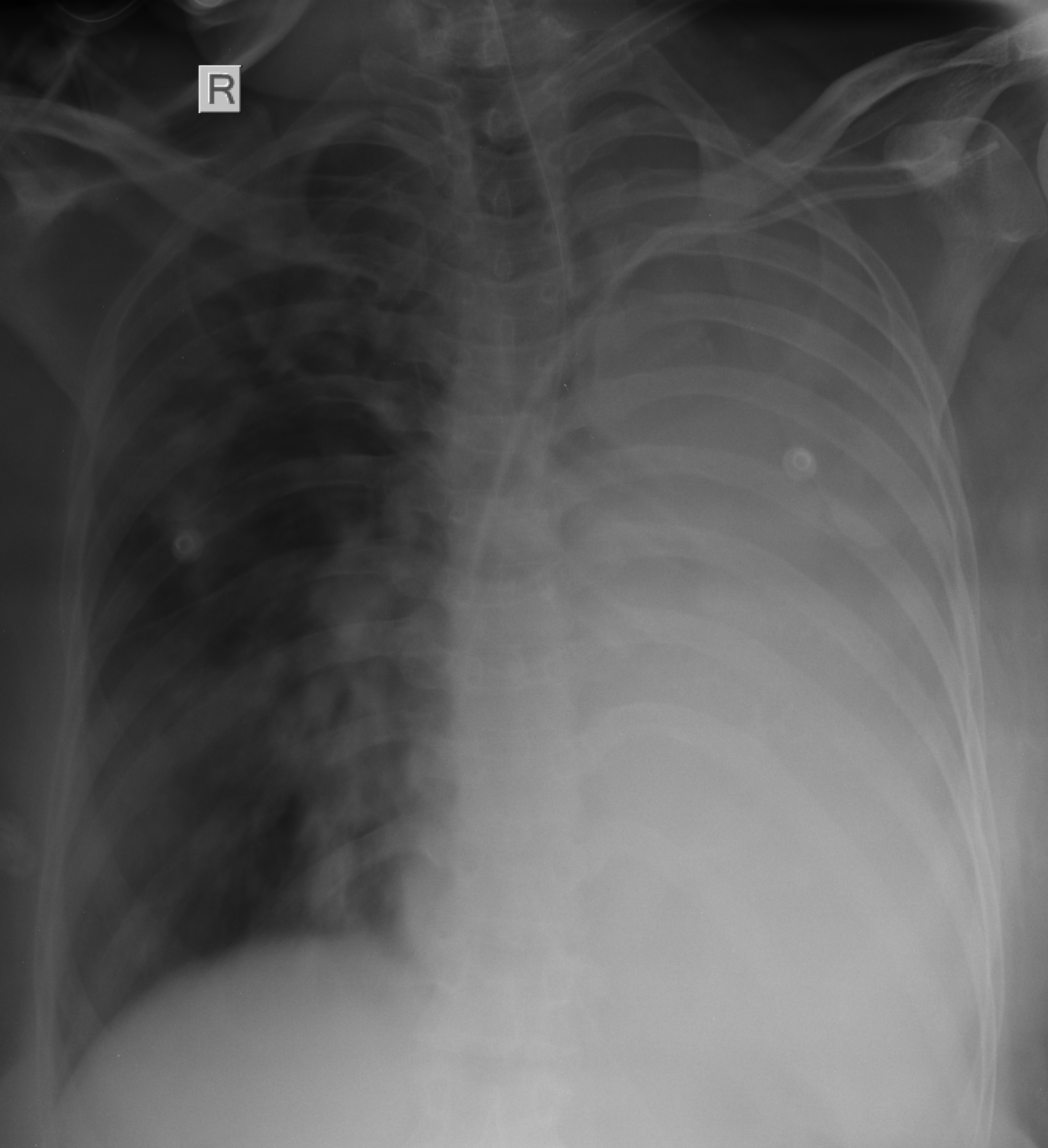
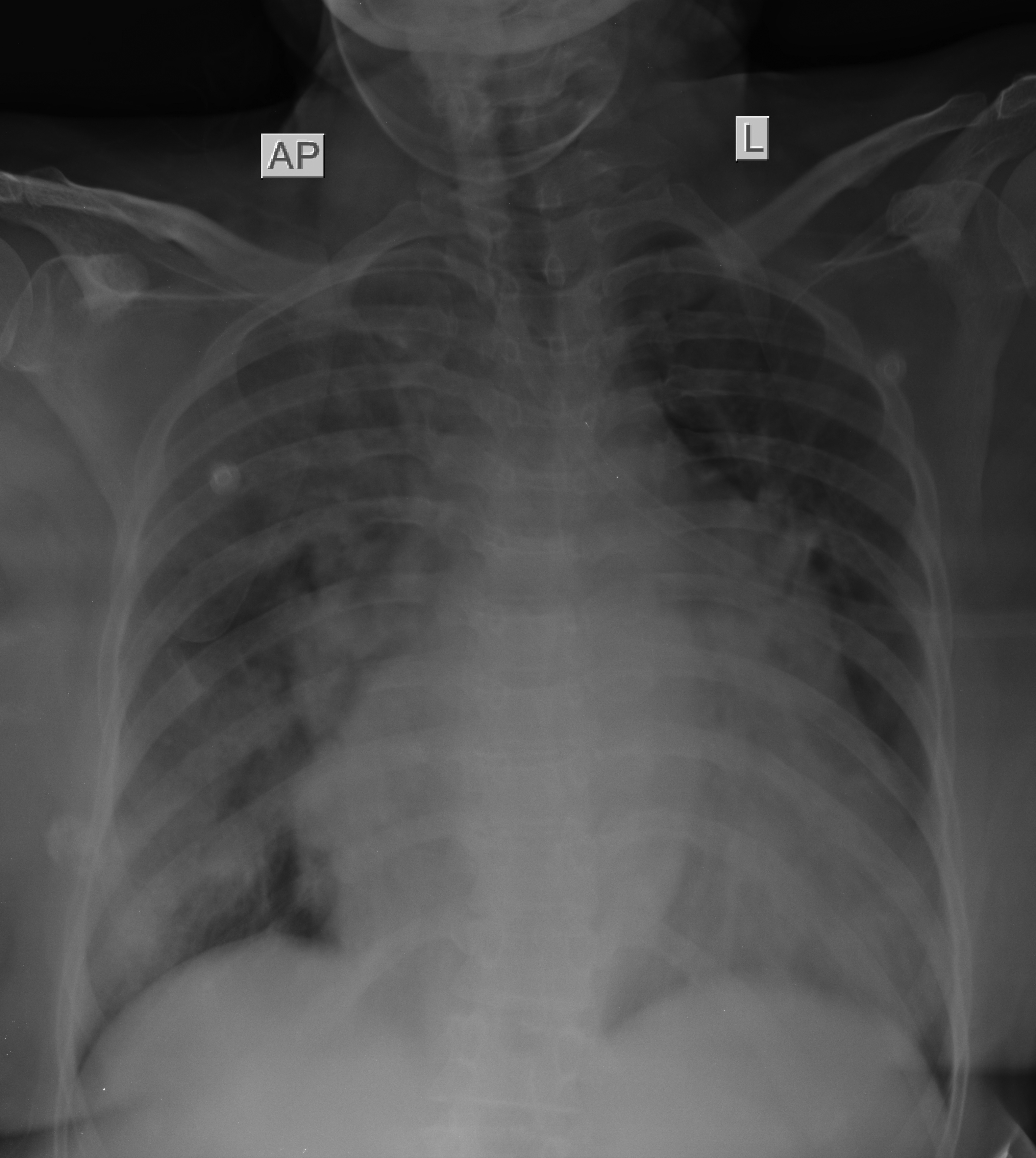
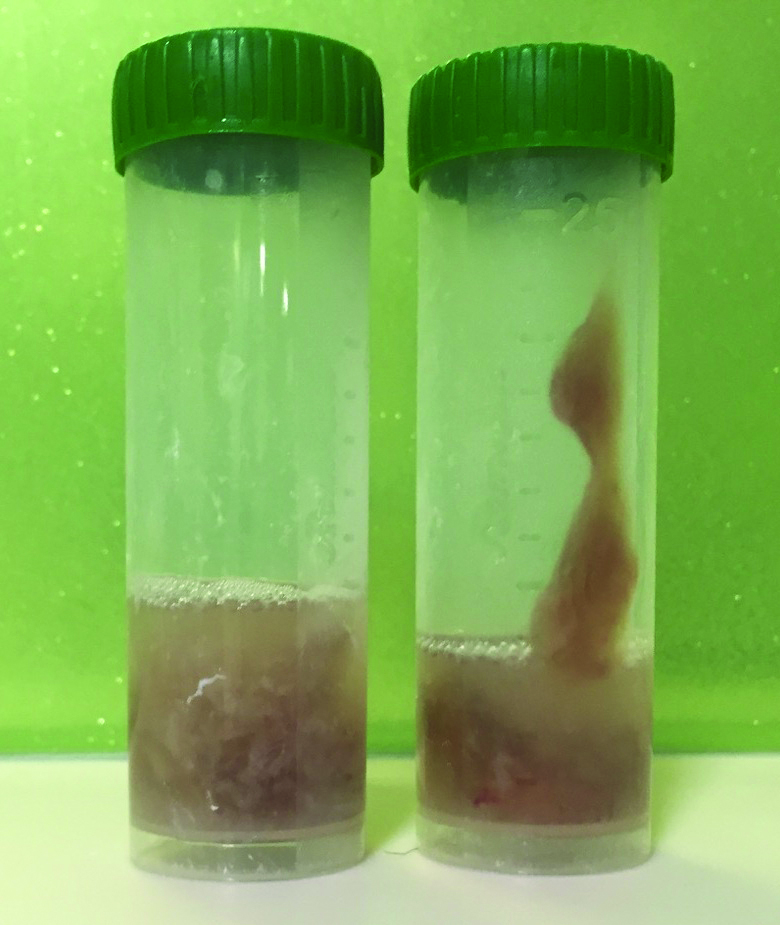
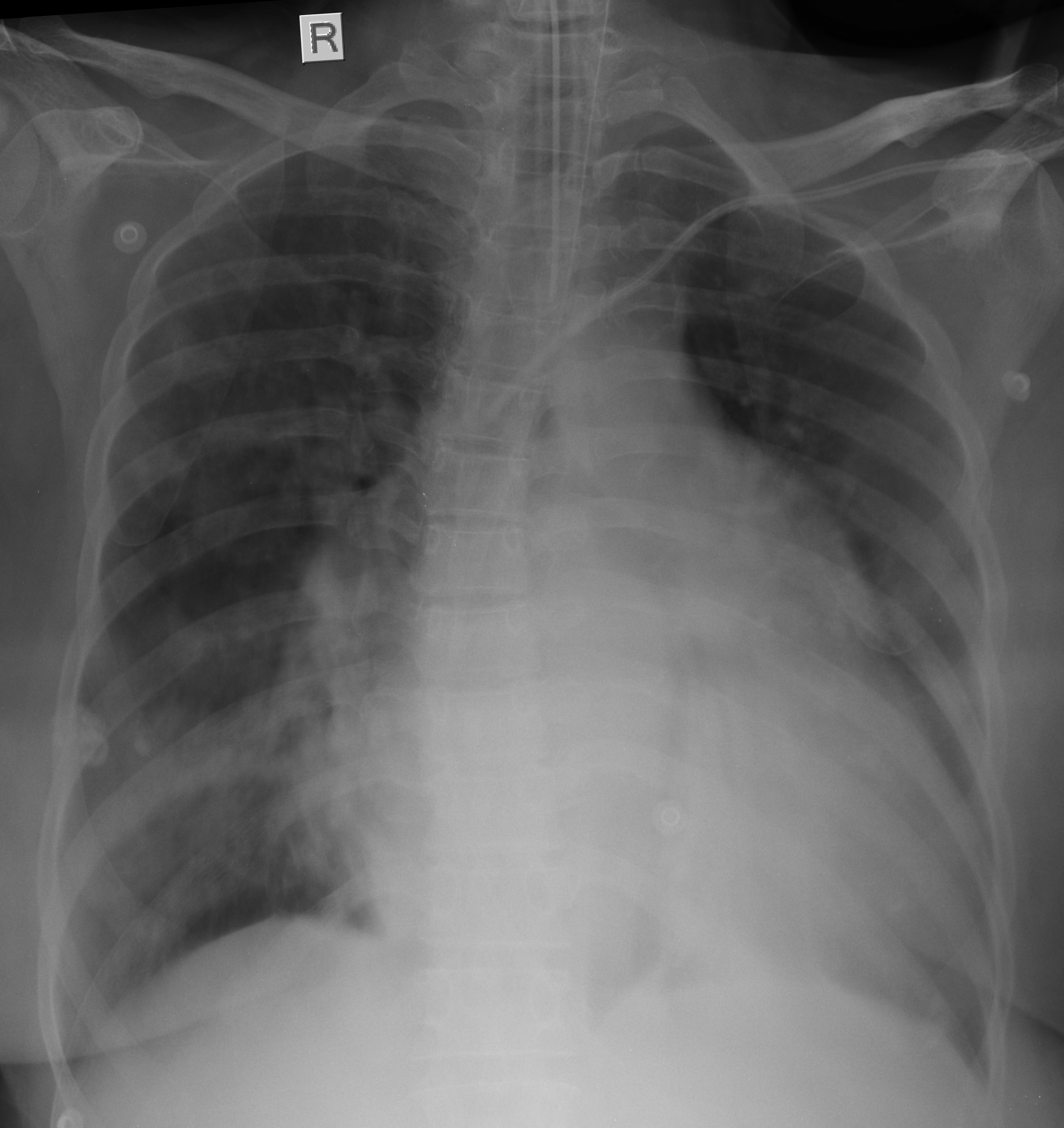
A 60-year-old-woman was referred for evaluation of total opacification of left hemithorax with ipsilateral shift of mediastinum in supine chest radiograph [Table/Fig-1]. Her latest Arterial Blood Gas (ABG) analysis showed a pH of 7.49, PaCO2 of 50.3 mmHg, PaO2 of 58.1 mmHg and HCO3– of 36 meq/L. She was on non-invasive ventilation with inspired Fraction of Oxygen (FiO2) of 0.6 and was on amiodarone infusion to control atrial fibrillation. Two days back, patient was admitted into Intensive Care Unit (ICU) for acute stroke with left hemiplegia and atrial fibrillation. Her initial ABG report showed pH of 7.28, PaCo2 of 67.4 mmHg, PaO2 of 51.8 mmHg and HCO3 of 26.2 mmol/L. Blood and urine reports were normal except for mild leucocytosis. Patient had pre-existing rheumatic heart disease with severe pulmonary arterial hypertension. A pre-admission supine chest radiograph taken in the emergency room showed cardiomegaly and left perihilar patchy opacities [Table/Fig-2]. A two dimensional transthoracic echocardiogram showed moderate mitral valve stenosis, severe tricuspid valve stenosis, severe pulmonary arterial hypertension and dilated right heart chambers. An ultrasound of chest suggested complete collapse of left lung with minimal effusion. Aggressive chest physiotherapy was avoided for fear of aggrevating atrial fibrillation. After obtaining high risk written consent, flexible bronchoscope (Pentax BF20) was introduced transnasally using 2% lidocaine jelly for lubrication while administering supplemental oxygen (FiO2 of 1.0) through the other nostril under midazolam sedation. Further, Flexible Bronchoscopy (FB) was done under local anaesthesia with 10% lidocaine spray for oropharynx and 2% lidocaine instilled through the bronchoscope from glottic level. At carinal level, thick mucous plug was seen completely occluding the left main bronchial orifice. A 5 ml of normal saline was instilled over the mucous plug and negative suction was applied. Part of the mucous plug was sucked into the bronchoscope and completely occluded the lumen of suction channel and further negative suction failed to clear it. The bronchoscope was withdrawn and the mucous was pushed out of bronchoscope with the bronchial brush into the collection trap. In the same way, all visible mucous was sucked out and collected in the collection trap [Table/Fig-3]. Electrocardiogram (ECG), oxygen saturation and blood pressure were monitored throughout the FB. FB was completed in about 8 minutes and was uneventful. A total of 20 ml of normal saline was instilled and bronchoscope was withdrawn twice to push the mucous out. At the end of procedure, breath sounds were well heard on auscultation over left lung. A post FB supine chest radiograph showed expansion of left lung [Table/Fig-4].
A supine chest radiograph showing complete opacification of left lung.
A pre-admission supine chest radiograph showing cardiomegaly and left perihilar opacities.
The airway mucous collected in trap.
Post bronchoscopy supine chest radiograph showing expanded left lung.
Mucus may accumulate in dependent portions of lung if the patient is bedridden for long duration without spontaneous movements. The other predisposing factors of mucous accumulation and plugging of airway include ineffective or inability to cough, inadequate inspiratory effort, obesity, pre-existing lung diseases with excessive mucus secretion like cystic fibrosis, bronchiectasis and endobronchial obstructive lesions like foreign body or tumour [1]. Our patient had immobility, inability to cough and muscle weakness as predisposing factors of airway mucous accumulation and plugging. Severe mucous plugging may cause airway obstruction resulting in worsening of gas exchange, increase in inspiratory pressure and may end up with infective complications if left untreated [2]. Chest physiotherapy may cause cardiac arrhythmias more often in critically ill aged and/or with acute cardiac disease; 11% had major arrhythmias and 25% had minor cardiac arrhythmias [3]. Our patient was 60-year-old with pre-existing cardiac disease and atrial fibrillation at presentation. FB is a safe procedure even in critically ill patients and cardiac arrhythmia like supraventricular tachycardia was documented only in 3.8% cases [4]. Critically ill patients with pre-existing coagulopathy, cardiac disease, hypoxaemia, pulmonary arterial hypertension and immunosuppression have additional risk of complications due to FB. Severe pulmonary hypertension is considered as a relative contraindication for bronchoscopy even though large scale studies are not available. Our case had severe pulmonary arterial hypertension with right heart failure. The most common indication for therapeutic bronchoscopy in a critically ill patient is retained mucus secretions and plugs in the airway and FB should not be avoided because of hypoxaemia as it can be life saving in some patients [5]. FB helps in identifying the aetiology of lung collapse quickly by direct inspection of the tracheobronchial tree and can detect blood clots occluding the bronchial lumen without any haemoptysis [6]. The other causes of complete lung collapse in ICU are retained foreign body and malpositioned endotracheal tube. Atelectasis is the most common cause of lung opacity in the ICU and radiologically, the signs of volume loss may be difficult to differentiate from consolidation [7]. Complete opacification of hemithorax may also be due to a large pleural effusion with underlying lung collapse. Bed side chest ultrasound can reliably rule out pleural effusion. Computed Tomography (CT) of chest may be more informative but mobilization of patient from ICU is usually difficult. Significant complications during FB in seriously ill patients can be prevented if aspiration is done intermittently and bronchoscope is withdrawn periodically atleast once in every five minutes [8]. We completed FB in about 8 minutes and the instrument was withdrawn twice to clear entangled thick strand of mucus into the collection trap. In our case, the negative suction was not strong enough to clear the thick mucous from the bronchoscope into the collection trap and brush biopsy forceps was used to push the mucous out of bronchoscope. Sometimes biopsy forceps or foreign body basket may have to be used to remove extremely tenacious mucous plugs. Bronchoscopic instillation of recombinant human DNase through bronchoscope was successful in improving atelectasis due to thick tenacious airway secretions unresponsive to medical treatment in selected cases of cystic fibrosis [9].
To conclude, short duration FB without biopsy procedures in a proper setting may be uncomplicated in patients with severe pulmonary arterial hypertension, right heart failure with cardiac arrhythmia like atrial fibrillation.
[1]. Jantz MA, Flexible bronchoscopy. In Gabrielli A, Layon AJ, Yu M editorsCivetta, Taylor and Kirby’s Manual of critical care 2009 4th edPhiladelphia PALippincott Williams & Wilkins:2171-88. [Google Scholar]
[2]. Mehrishi S, Is bronchoscopy indicated in the management of atelectasis?J Bronchol 2002 9:46-51. [Google Scholar]
[3]. Hamman WE, Connors AF, McCaffree DR, Cardiac arrhythmias during postural drainage and chest percussion of critically ill patientsChest 1992 102:1836-41. [Google Scholar]
[4]. Estella A, An analysis of 208 flexible bronchoscopies performed in our intensive care unitMed Intensiva 2012 36:396-401. [Google Scholar]
[5]. Prakash UBS, Emergency bronchoscopy in the critically ill patientsJ Bronchol 1998 5:275-79. [Google Scholar]
[6]. Arney KL, Judson MA, Sahn SA, Airway obstruction arising from blood clot. Three reports and a review of literatureChest 1999 115:293-300. [Google Scholar]
[7]. Mahajan VK, Catron PW, Huber GL, The value of fiberoptic bronchoscopy in the management of pulmonary collapseChest 1978 73:617-20. [Google Scholar]
[8]. Fishman JE, Primack SL, Thoracic imaging in the intensive care unitAppl Radiol 2005 34:8-17. [Google Scholar]
[9]. McLaughlin AM, McGrath E, Barry R, Egan JJ, Gallagher CG, Treatment of lobar atelectasis with bronchoscopically administered recombinant human deoxyribonuclease in cystic fibrosisThe Clinical Respiratory Journal 2008 2:123-26. [Google Scholar]