A Rare Collision Tumour of Uterus- Squamous Cell Carcinoma and Endometrial Stromal Sarcoma
Nadeem Tanveer1, Bindiya Gupta2, Abhishek Pathre3, Shalini Rajaram4, Neerja Goyal5
1 Associate Professor, Department of Pathology, University College of Medical Sciences, Delhi, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, University College of Medical Sciences, Delhi, India.
3 Post Graduate Student, Department of Pathology, University College of Medical Sciences, Delhi, India.
4 Director and Professor, Department of Obstetrics and Gynaecology, University College of Medical Sciences, Delhi, India.
5 Director and Professor, Department of Obstetrics and Gynaecology, University College of Medical Sciences, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nadeem Tanveer, Associate Professor, Department of Pathology, University College of Medical Sciences, Dilshad Garden, Delhi-110095, India.
E-mail: ntobh104@yahoo.co.in
Collision tumours are defined by co-existence of two tumours in the same or adjacent organs which are topographically and histologically distinct with minimal or no histological admixture. Collision tumours have been described in many organs notably thyroid, brain, adrenal gland, stomach and rarely uterus. Most of the collision tumours reported in uterus have two components; an adenocarcinoma and a sarcoma. We report a case of a 60-year-old lady who presented with complaints of post-menopausal bleeding. A cervical biopsy was performed which showed a non-keratinizing squamous cell carcinoma of cervix. Intra-operatively the uterus was bulky with a 6 cm x 5 cm polypoidal mass in the endometrial canal along with a 2 cm friable cervical growth. The fleshy uterine cavity mass was a spindle cell tumour with moderate pleomorphism and frequent mitosis. It was immunopositive for CD10 and negative for smooth muscle actin and cytokeratin 5/6. The other growth showed non-keratinizing squamous cell carcinoma which was positive for cytokeratin 5/6. Based on the distinct topographical location and limited areas of tumour admixture of the two tumours, a diagnosis of collision tumour of uterus comprising of endometrial stromal sarcoma (high grade) uterus and squamous cell carcinoma cervix was made.
Adenocarcinoma, Endometrial neoplasms, Post-menopausal bleeding
Case Report
A 60-year-old lady P8L8 presented with complaints of foul smelling blood stained discharge per vaginum for 6 months. She had one episode of post-menopausal bleeding one month back. There was no history of post-coital bleeding, dyspareunia or abdominal pain. She attained menarche at 12 years of age and menopause 12 years back with normal perimenopausal transition. Previous cycles were 4-5 days/28 days with normal flow. She was a tobacco chewer for 15 years. There was no significant past or family history.
On examination there was pallor without organomegaly. On per speculum examination 1.5 cm x 1.0 cm growth was found on anterior lip of cervix. On per vaginal examination uterus was anteverted bilateral fornices were free and a friable growth was felt on anterior lip of cervix which bled on touch. On per rectal examination bilateral parametria and rectal mucosa were free. The clinical diagnosis was carcinoma cervix stage 1b1. Her haemogram, liver function tests and renal function tests were within normal limits.
A cervical biopsy was performed which was reported as non-keratinizing squamous cell carcinoma. A Transvaginal Ultrasound (TVS) was performed which showed myohyperplasia, bilateral ovaries and endometrial thickness were normal. Contrast Enhanced Computed Tomography (CECT) chest was normal. Radical hysterectomy (Type III) with bilateral pelvic lymphadenectomy was performed.
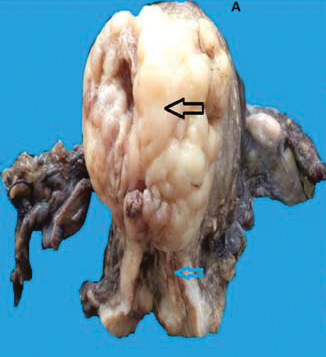
Intra-operatively the uterus was bulky with a 6 cm x 5 cm polypoidal mass in the endometrial canal along with a 2 cm friable cervical growth. Bilateral external iliac nodes were mildly enlarged. The rest of the lymph nodes were of normal size. The specimen of uterus with cervix with bilateral fallopian tubes and ovaries was received in 10% formalin in the histopathology department. The uterus with cervix measured 8 cm x 6.5 cm x 5 cm. An exophytic globular mass measuring 6 cm x 5 cm was identified arising from the posterior wall of uterus and almost completely obliterating the uterine cavity [Table/Fig-1]. On cut-section this mass was fleshy in consistency whereas, another adjacent 2 cm x1cm grey white growth identified in the cervix was hard and friable in consistency. Multiple sections were examined from both the tumours and also from the intervening area. Both the fallopian tubes and ovaries were unremarkable.
Gross photograph of resection specimen of uterus with cervix and bilateral fallopian tubes and ovaries. Black arrow shows the fleshy tumour arising from corpus with areas of haemorrhage (Endometrial stromal sarcoma) while the blue arrow shows the adjacent squamous cell carcinoma.
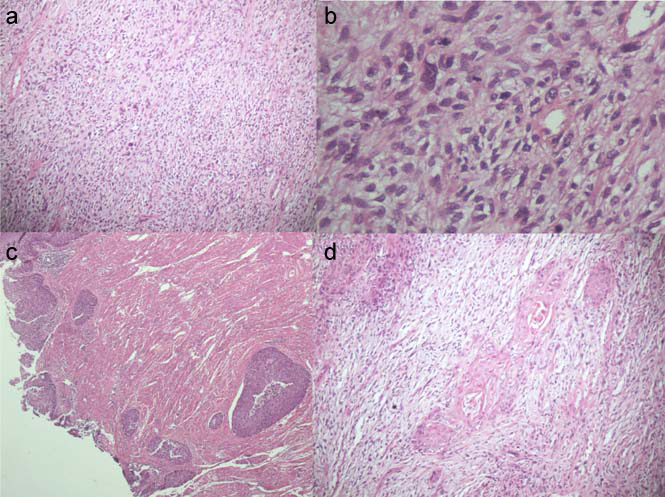
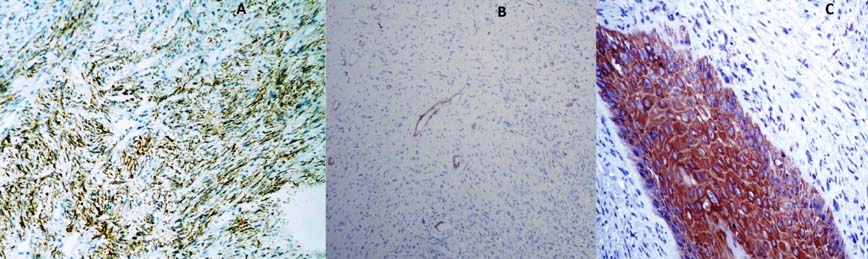
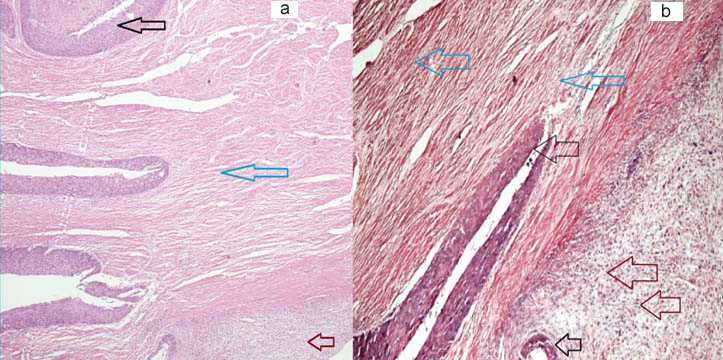
On microscopic examination the fleshy uterine cavity mass showed a high grade spindle cell tumour with marked pleomorphism, frequent mitosis (8 per 10 high power field) and foci of necrosis. The tumour cells were ovoid to spindle shaped with minimal cytoplasm intimately associated with prominent arterioles. The tumour infiltrated the myometrium in broad fronts. No whorling pattern was seen [Table/Fig-2]. On immunohistochemistry the tumour cells were immunopositive for CD10 and negative for Smooth muscle antigen and cytokeratin 5/6 [Table/Fig-3]. This tumour was diagnosed as high grade endometrial stromal sarcoma. Sections from the cervical growth showed non-keratinizing squamous cell carcinoma which was clearly separated from the sarcoma by the intervening cervical stroma [Table/Fig-4a,b]. Only an occasional focus of intermingling with the sarcoma was found in the sections taken from the endocervical canal in continuity with the endometrial canal [Table/Fig-2]. The rest of the sections taken from the cervix were free of sarcoma component. The carcinoma was immunopositive for cytokeratin 5/6 while the sarcoma was immunonegative [Table/Fig-3].
a,b) Endometrial stromal sarcoma with moderate pleomorphism and frequent mitoses (H&E; 10X, 40X respectively); c) Area showing squamous cell carcinoma (H&E; 10X); d) Rare area of histological admixture of the two tumours (H&E; 20X)
a) Endometrial stromal sarcoma immunopositive for CD10 (IHC; 10X); b) Immunonegative for Smooth Muscle Actin (SMA) (IHC; 10X); c) Squamous cell carcinoma component is immunopositive for cytokeratin 5/6 while the surrounding endometrial stromal sarcoma is negative (IHC; 40X).
Black arrow shows squamous cell carcinoma while brown arrow shows endometrial stromal sarcoma. The blue arrow marks the intervening uninvolved stroma separating the two tumours and highlighting the topographically distinct location (H&E; 10X).
All the lymph nodes were negative for metastasis. The bilateral parametria and resected margins of cuff-of vagina were free of tumour. Both the fallopian tubes and ovaries were unremarkable.
Final diagnosis of collision tumour comprising of high grade endometrial stromal sarcoma and squamous cell carcinoma was given keeping in mind the topographically distinct location of the two tumours. The patient is disease free after six month follow-up and is receiving chemotherapy.
Discussion
Collision tumour should be viewed as occurrence of multiple synchronous tumours in the same organ or two adjacent organs. The components are separated from each other by normal stroma with little or no histological admixture. Collision tumours are of special interest to the pathologist since, they have to be differentiated from composite tumours [1,2]. The individual components of a composite tumour are intimately admixed with each other and it is not possible to separate them topographically. Composite tumours are characterized by two divergent lineages originating from the same neoplastic clonal proliferation. Malignant mixed mullerian tumours of uterus are composite tumours and are believed by many, to behave like metaplastic carcinomas. In contrast the prognosis and management of collision tumours is dictated by the histology of its individual components [2].
Collision tumours of uterus are rare with only few such cases reported till date [3]. Most of these are composed of adenocarcinoma (endometrioid or papillary serous) colliding with a sarcoma (leiomyosarcoma or endometrial stromal sarcoma) [4]. The unusual components of collision tumours reported include hepatoid carcinoma and malignant rhabdoid tumour [5,6]. All the collision tumours of uterus reported till date except one had two components. This extremely rare case had three components –endometrioid adenocarcinoma, papillary serous carcinoma, and malignant mixed mullerian tumour [3].
In our case, both the components were topographically distinct with uninvolved stroma separating the two components and only minimal admixture. Immunohistochemistry was performed to confirm the divergent histogenesis of the two components. The sarcoma component was immune-negative for smooth muscle antigen and immune-positive for CD10 confirming the endometrial stromal origin. Immunohistochemistry for cytokeratin 5/6 was performed on the sections showing the rare areas of histological admixture. Cytokeratin 5/6 was preferred over pan cytokeratin since, pan cytokeratin is frequently positive in endometrial stromal sarcomas whereas, cytokeratin 5/6 is almost always negative [7]. Cytokeratin 5/6 stains most of the squamous cell carcinomas [8]. The demonstration of uninvolved stroma separating the two components [Table/Fig-3] is important for proving histologically that, the tumours are topographically distinct. A carefully chosen section taken from the area of collision serves this purpose.
The terminology of collision, composite and synchronous tumours needs to be re-visited. The occurence of two synchronous tumours in the same organ with no admixture should ideally not be called collision. Similarly, presence of a neuroendocrine component in a mixed tumour creates problems–whether these should be called collision or composite tumours is a matter of debate [9].
This case has been reported in view of its rarity and unique gross and microscopic features of tumour admixture. The details of other similar cases in literature have been presented in [Table/Fig-5] [1,3–6,10–13].
List of collision tumours of uterus and their components reported in literature till date [1,3–6,10–13].
| S.No | Components | Age | Ref |
|---|
| Adenocarcinoma | Sarcoma | Other | | |
| 1 | Endometrioid | Endometrial stromal sarcoma | | 73 | 1 |
| 2 | Papillary Serous | Leiomyosarcoma | | 55 | 12 |
| 3 | Endometrioid | Endometrial Stromal Sarcoma | | 36 | 13 |
| 4 | Endometrioid | Endometrial Stromal Sarcoma | | 55 | 13 |
| 5 | Endometrioid | Endometrial Stromal Sarcoma | | 59 | 13 |
| 6 | Papillary SerousEndometrioid | | Malignant Mixed Mullerian tumour | 70 | 3 |
| 7 | Hepatoid carcinoma | | Carcinosarcoma | 68 | 5 |
| 8 | Endometrioid adenocarcinoma | Endometrial stromal sarcoma high grade | | 47 | 4 |
| 9 | Endometrioid adenocarcinoma | Endometrial stromal sarcoma high grade | | 85 | 4 |
| 10 | Endometrioid Adenocarcinoma | | Malignant Rhabdoidtumour | 49 | 6 |
| 11 | Serous carcinoma | Heterologous sarcoma | | 72 | 11 |
| 12 | Endometrioid adenocarcinoma | Homologous sarcoma | | 67 | 11 |
| 13 | Adenocarcinoma | Leiomyosarcoma | | 55 | 10 |
| 14 | - | Endometrial stromal sarcoma | Squamous cell carcinoma | 60 | Our case |
Conclusion
Rarely, we may encounter two tumours with different morphologies intermingling with each other which may create confusion in diagnosis or may even lead to an erroneous diagnosis. Thus, it is important to differentiate between collision tumours, composite tumours and carcinosarcomas in such situations.
[1]. Liu G, Zhang C, Ma Z, Zhang Q, Liu B, Endometrial stromal sarcoma with endometrioid adenocarcinoma of the uterus: a case reportInternational Journal of Clinical and Experimental Pathology 2015 8(5):5242-46. [Google Scholar]
[2]. McCluggage WG, Malignant biphasic uterine tumours: carcinosarcomas or metaplastic carcinomas?J ClinPathol 2002 55(5):321-25. [Google Scholar]
[3]. Jang K-S, Lee W-M, Kim Y-J, Cho S-H, Collision of three histologically distinct endometrial cancers of the uterusJ Korean Med Sci 2012 27:89-92. [Google Scholar]
[4]. Lam KY, Khoo US, Cheung A, Collision of endometrioid carcinoma and stromal sarcoma of the uterus: a report of two casesInt J Gynecol Pathol 1999 18:77-81. [Google Scholar]
[5]. Takahashi Y, Inoue T, Hepatoid carcinoma of the uterus that collided with carcinosarcomaPathol Int 2003 53:323-26. [Google Scholar]
[6]. Gaertner EM, Farley JH, Taylor RR, Silver SA, Collision of uterine rhabdoidtumour and endometrioid adenocarcinoma: a case report and review of the literatureInt J Gynecol Pathol 1999 18:396-401. [Google Scholar]
[7]. Adegboyega PA, Qiu S, Immunohistochemical profiling of cytokeratin expression by endometrial stromal sarcomaHum Pathol 2008 39(10):1459-64. [Google Scholar]
[8]. Chu PG, Weiss LM, Expression of cytokeratin 5/6 in epithelial neoplasms: An immunohistochemical study of 509 casesMod Pathol 2002 15(1):6-10. [Google Scholar]
[9]. Yazici O, Aksoy S, Özhamam EU, Zengin N, Squamous cell and neuroendocrine carcinoma of esophagus: Collision versus composite tumour: A case report and review of literatureIndian J Cancer 2015 52(4):603-04. [Google Scholar]
[10]. Patwardhan JR, Gadgil RK, Collision tumour of the uterusIndian J Cancer 1969 6:194-97. [Google Scholar]
[11]. Sreenan JJ, Hart WR, Carcinosarcomas of the female genital tract. A pathologic study of 29 metastatic tumours: further evidence for the dominant role of the epithelial component and the conversion theory of histogenesisAm J Surg Pathol 1995 19:666-74. [Google Scholar]
[12]. Nagamuthu EA, Fatima SS, Collision tumour-An unusual case reportAdvApplSci Res 2014 5(3):172-178. [Google Scholar]
[13]. Kim G, Pham HQ, Ramzan A, Elishaev E, Mhawech-Fauceglia P, Endometrioid adenocarcinoma associated with endometrial stromal sarcoma: A rare, often unrecognized collision tumourGynecol Oncol Rep 2015 13:8-12. [Google Scholar]