Case Report
A 54-year-old female with no significant past history and co-morbidities presented with a gradually progressive, non-tender swelling in the upper outer aspect of left eye since two years. She also noticed proptosis and diplopia on lateral gaze for the past one year. She denied any vision problems or dryness of eyes.
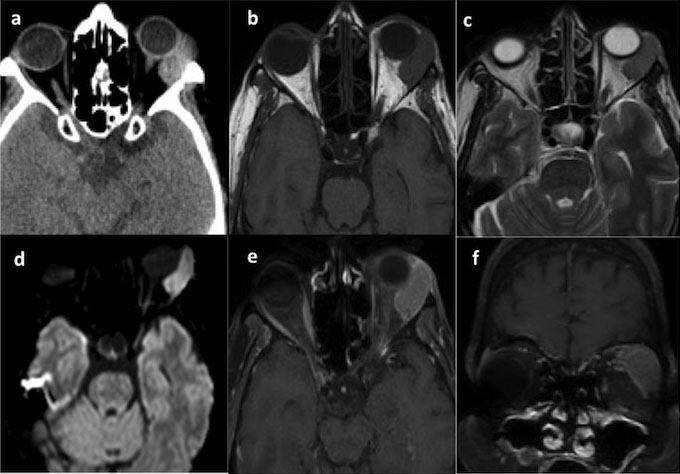
On examination, except for a restriction of extraocular movements in the left eye on lateral gaze, rest of the neurological examination was unremarkable. A thorough systemic examination revealed no abnormality. Computed Tomography (CT) showed a well-defined extraconal lesion which appeared iso-hyperdense located in the supero-lateral quadrant of left orbit in the region of lacrimal gland with no evidence of calcification or bony changes [Table/Fig-1a]. On Magnetic Resonance Imaging (MRI), the lesion measured 2.7 cm x 1.1 cm x 2.5 cm, appeared isointense on T1 and mildly iso to hypointense on T2 images, with prominent diffusion restriction and homogeneous contrast enhancement [Table/Fig-1b-f]. The optic apparatus was essentially normal.
a) Axial CT brain showing an iso-hyperdense extraconal lesion located in the supero-lateral quadrant of left orbit with no evidence of calcification or bony changes; 1b) MRI brain showing the lesion to be isointense on T1; 1c) Iso to hypointense on T2 images; 1d) with diffusion restriction; 1e,f) and homogeneous contrast enhancement.
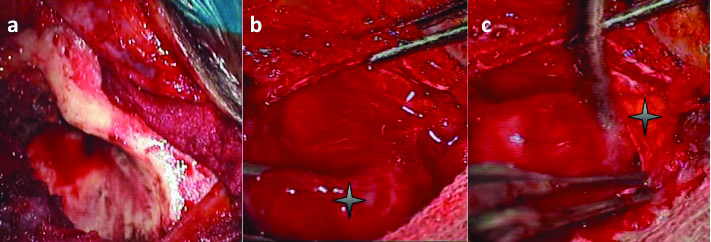
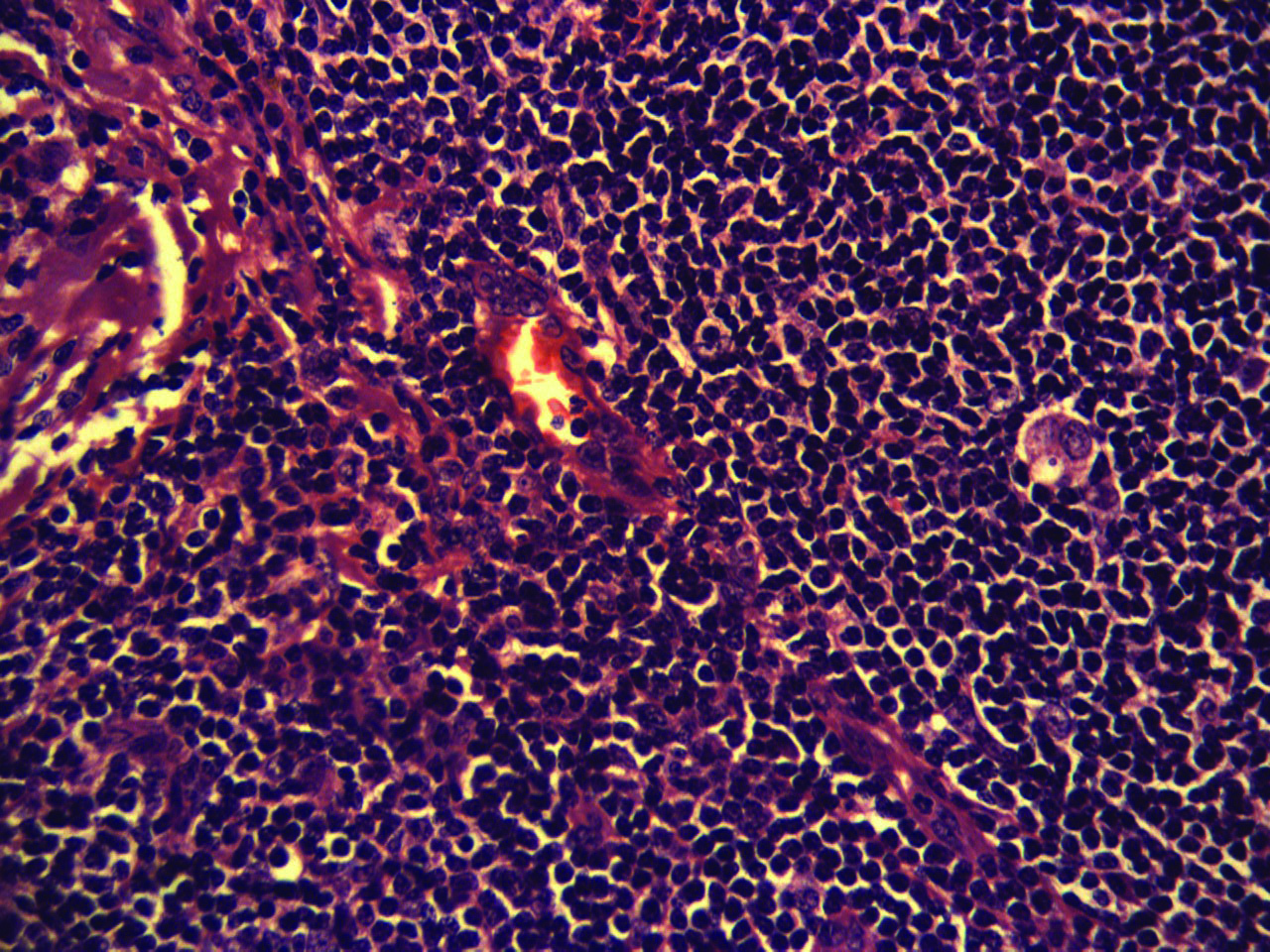
The differential diagnoses considered were lymphoma of the orbit or a primary lacrimal gland tumour such as pleomorphic adenoma. After discussing the pros and cons of biopsy versus resection, the latter one was consented by the patient. A lateral orbitotomy (Kronlein’s approach) [Table/Fig-2a] and complete enbloc removal of the lesion was performed. The lesion was attached to the supero-lateral orbital wall, was firm in consistency, well circumscribed and encapsulated [Table/Fig-2b]. The lacrimal gland was seen separately, but was abutting the lesion [Table/Fig-2c]. Histopathological examination showed a tumour composed of nodules of abnormal small lymphoid cells in a follicular pattern with endothelial venules and hyalinixed blood vessels. The lymphoid cells were positive for CD10, CD20, Bcl2 while negative for CD3, CD5, cyclin D and Bcl6. Overall features were suggestive of Non-Hodgkin’s Lymphoma (NHL)- follicular subtype [Table/Fig-3]. Bone marrow examination was negative for lymphoma. A whole body Positron Emission Tomography (PET) scan ruled out any systemic involvement.
a) Exposure for a lateral orbitotomy (Kronlein’s approach); b) The supero-lateral orbital rim, zygomatic and adjacent sphenoid bones have been exposed. A well circumscribed and encapsulated lesion is seen attached to the supero-lateral orbital wall (asterisk); c) Complete enbloc removal was performed. The lacrimal gland can be seen separately abutting the lesion (asterisk).
Histopathological photomicrograph (H&E x40) showing a tumour composed of nodules of abnormal small lymphoid cells in a follicular pattern with endothelial venules and hyalinized blood vessels, features suggestive of non-Hodgkin’s lymphoma- follicular subtype.
Thus, a diagnosis of primary localized extranodal lymphoma (Stage 1E) was made. Patient was referred to radiation oncology where she received a radiation dose of 30.6 Gy in 17 fractions delivered locally to the orbit. At the latest follow up of 14.5 months, she was doing well with modest improvement in diplopia and no signs of disease recurrence.
Discussion
Lymphomas are rare tumours of the orbit representing the malignant end of the spectrum of lymphoproliferative orbital lesions, and comprise lymphomas of the conjunctiva, lacrimal gland, eyelids and ocular musculature. These OL or otherwise Ocular Adnexal Lymphomas (OAL) account for 10% of malignant orbital tumours, 1% of NHL and 8% of all extranodal lymphomas [1–4]. Individuals in the fifth to seventh decade are mostly affected and a slight female preponderance is usually seen [4]. Painless proptosis, diplopia and palpable mass are the common presenting features while vision is rarely affected [5,6].
Due to its relatively benign course and nonspecific signs and symptoms, diagnosis and treatment is often delayed [7]. Majority of tumours are located in the supero-lateral quadrant of the orbit, are commonly extra conal and are almost always unilateral [5]. They form a heterogeneous group and the most common subtype is the extranodal marginal B-cell MALT-type lymphomas, seen in >70%-80% of cases. Other subtypes include follicular (5-10%), diffuse large B-cell and mantle cell lymphomas (9%) [7–11].
In a recent study of ocular adnexal follicular lymphoma in the Danish population over a 30-year period, 24 patients were identified of whom only 11 had primary OAL [12]. Of the 11 cases of OL analyzed by Eckardt AM et al., over an eight year period, none were of follicular subtype primary ones [7]. MRI is the investigation of choice providing excellent details of the adjacent orbital structures and the status of optic apparatus. These lesions appear well-circumscribed, shows diffusion restriction and homogeneous enhancement. Differential diagnoses include cavernous haemangiomas, other lymphoid lesions of the orbit, nerve sheath tumours, metastasis, haemangiopericytoma and others [1].
Staging of lymphomas is extremely important for therapeutic and prognostic reasons, for which the ANN ARBOR classification is the most widely followed [1,5]. According to this, any single extranodal site such as the orbit is categorized as stage IE disease. Other recent staging systems include International Prognostic Index (IPI), Lugano classification and Follicular Lymphoma International Prognostic Index (FLIPI) [12–14].
Treatment options include surgery, radiotherapy and chemotherapy. Role of surgery is limited to biopsy in majority of cases. Surgery alone is associated with a high relapse rate, however, Esik O et al., reported 0% local relapse-free survival at 10 years in patients treated with surgery alone [15]. Surgical approach depends upon the location of the lesion- lateral orbitotomy for laterally located tumours, transconjunctival approach for medial, basal extra-intraconal lesions and pterional intra-extradural procedures for orbital apex lesions or those with intracranial extensions [16]. Primary radiotherapy (usually 25-35 Gy) is the standard treatment for stage 1E OL [1,6,7,11,12,17].
In the series of Rasmussen PK et al., of the 11 patients with primary localized ocular adnexal follicular lymphoma, 10 underwent radiotherapy (after open biopsy confirmation) and one was treated with surgery [12]. In the study by Eckardt AN et al., all of the seven stage 1E patients were treated with radiotherapy after diagnostic confirmation through an open biopsy [7]. Chemotherapy is preferred for systemic and disseminated disease [1,6,7,11,17]. The most common combination chemotherapy regimens include cyclophosphamide, adriamycin, vincristine and prednisone (CHOP) or CHOP with rituximab (R-CHOP) [7,18]. Since local therapy as a first-line treatment for limited stages OAL (MALT-type) has given excellent results in various studies, it might not mean that this is the ideal treatment, because of the simple reason that no direct comparison studies (to systemic treatment approaches) have been performed yet (PLOS). Also, there are possible long-term risks of radiotherapy.
Hashimoto N et al., analyzed long-term outcomes of OL treated with radiotherapy alone and found that a total of 23/78 (30%) subsequently developed Grade III cataract and seven patients had retinal disorders [19]. Furthermore, in a recent study, Paik JS et al., compared the ophthalmologic outcomes of radiotherapy versus chemotherapy or combined chemo-radiotherapy and demonstrated significantly lower rates of ophthalmological symptoms in patients with non-conjunctival OAL (MALT-type) receiving no radiotherapy without compromising on the therapeutic outcome [20]. For these reasons, a randomized trial of radiotherapy versus systemic therapy is warranted [11]. A wait and watch policy may be a reasonable option in few selected cases, if optic nerve involvement has been ruled out by necessary tests. Tanimoto K et al., managed 36 localized OAL with observation alone and noted that 70% still did not require treatment after a median follow-up of seven years [21]. Other novel treatments under research include radioimmunotherapy with Y-90, lenalidomide, ibritumomab tiuxetan and antibiotics against Chlamydiae psittaci (doxycycline/clarithromycin) [2,11].
Prognosis is usually good and favourable for low-grade tumours with radiotherapy alone achieving local control rates of >90%. Prognostic criteria have been defined as per the Revised European American Lymphoma (REAL) classification; of these, younger age, low-grade histology, favourable response and a conjunctival location were statistically significant on multivariate analysis [22]. Poor prognostic factors include nonconjunctival primary site, advanced disease stage, nodal involvement, age >60 years, presence of B symptoms, and elevated serum Lactat edehydrogenase (LDH) levels [2]. Other biomarkers that could possibly indicate unfavourable prognosis include expression of CD5, CD43, p53, Bcl-6 and Bcl-10 [2]. Recurrences and relapses are known and hence, regular and long-term follow-up (clinical and radiological) is recommended [1,5,11,23].
Conclusion
Primary OAL are uncommon, extranodal lymphoid neoplasms. Majority of them are low-grade tumours of the MALT-type and usually carry a good prognosis. Local radiotherapy is the standard treatment, however, randomized trials of radiotherapy with systemic therapy are necessary in future in view of proven delayed adverse effects of local radiotherapy. In very few selected cases, observation alone may be tried. Much of the research work pertaining to therapeutic approaches in OL has been performed in MALT-type, simply because it’s the most common type of OL. But, because of the rarity, it is yet unclear as to whether these results can be reciprocated to the follicular type.
[1]. Gveroviæ-Antunica A, Markoviæ I, Bohaè M, Coroviæ-Arneri E, Ivaniin-Baraè A, Karaman K, Primary orbital non-hodgkins lymohoma. case reportActa Clin Croat 2007 46:113-16. [Google Scholar]
[2]. Stefanovic A, Lossos IS, Extranodal marginal zone lymphoma of the ocular adnexaBlood 2009 114:501-10. [Google Scholar]
[3]. Freeman C, Berg JW, Cutler SJ, Occurrence and prognosis of extranodal lymphomasCancer 1972 29:252-60. [Google Scholar]
[4]. Essadi I, Tazi EM, Allam W, Sbitti Y, Ichou M, Errihani H, Primary non Hodgkin’s lymphoma of the orbit: A case reportMedical Case Studies 2011 2:19-21. [Google Scholar]
[5]. Priego G, Majos C, Climent F, Muntane A, Orbital lymphoma: imaging features and differential diagnosisInsights Imaging 2012 3:337-44. [Google Scholar]
[6]. Cicco LD, Cella L, Liuzzi R, Solla R, Farella A, Punzo G, Radiation therapy in primary orbital lymphoma: a single institution retrospective analysisRadiat Oncol 2009 4:60 [Google Scholar]
[7]. Eckardt AM, Lemound J, Rana M, Gellrich NC, Orbital lymphoma: diagnostic approach and treatment outcomeWorld J Surg Onc 2013 11:73 [Google Scholar]
[8]. Coupland SE, Hummel M, Stein HM, Ocular adnexal lymphomasSurv Ophthalmol 2002 47:470-90. [Google Scholar]
[9]. Fung CY, Tarbell NJ, Lucarelli MJ, Goldberg SI, Linggood RM, Harris NL, Ocular adnexal lymphoma: Clinical behavior of distinct World Health Organization classification subtypesInt J Rad Oncol Biol Phys 2003 57:1382-91. [Google Scholar]
[10]. Coupland SE, Hellmich M, Auw-Haedrich C, Lee WR, Stein H, Prognostic value of cell- cycle markers in ocular adnexal lymphoma: an assessment of 230 casesGraefes Arch Clin Exp Ophthalmol 2004 242:130-45. [Google Scholar]
[11]. Kiesewetter B, Lukas J, Kuchar A, Mayerhoefer ME, Streubel B, Lagler H, Clinical features, treatment and outcome of mucosa-associated lymphoid tissue (MALT) lymphoma of the ocular adnexa: single center experience of 60 patientsPLoS One 2014 9:e104004 [Google Scholar]
[12]. Rasmussen PK, Ralfkiaer E, Prause JU, Sjö LD, Specht L, Rossing HH, Follicular lymphoma of the ocular adnexal region: a nation-based studyActa Ophthalmol 2015 93:184-91. [Google Scholar]
[13]. Cheson B, Pfistner B, Juweid M, Gascoyne RD, Specht L, Horning SJ, Revised response criteria for malignant lymphomaJ Clin Oncol 2007 25:579-86. [Google Scholar]
[14]. Armitage JO, Staging Non-Hodgkin lymphomaCA Cancer J Clin 2005 55:368-76. [Google Scholar]
[15]. Esik O, Ikeda H, Mukai K, Kaneko A, A retrospective analysis of different modalities for treatment of primary orbital non-Hodgkins lymphomaRadiother Oncol 1996 38:13-18. [Google Scholar]
[16]. Schick U, Lermen O, Unsold R, Hassler W, Treatment of primary orbital lymphomasEur J Haematol 2004 72:186-92. [Google Scholar]
[17]. Cohen V, Treatment options for ocular adnexal lymphomaClin Ophthalmol 2009 3:689-92. [Google Scholar]
[18]. Coiffier B, Lepage E, Brière J, Herbrecht R, Tilly H, Bouabdallah R, CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-b-cell lymphomaN Engl J Med 2002 346:235-42. [Google Scholar]
[19]. Hashimoto N, Sasaki R, Nishimura H, Yoshida K, Miyawaki D, Nakayama M, Long-term outcome and patterns of failure in primary ocular adnexal mucosa- associated lymphoid tissue lymphoma treated with radiotherapyInt J Radiat Oncol Biol Phys 2012 82:1509-14. [Google Scholar]
[20]. Paik JS, Cho WK, Lee SE, Choi BO, Jung SE, Park GS, Ophthalmologic outcomes after chemotherapy and/or radiotherapy in non-conjunctival ocular adnexal MALT lymphomaAnn Hematol 2012 91:1393-401. [Google Scholar]
[21]. Tanimoto K, Kaneko A, Suzuki S, Sekiguchi N, Maruyama D, Kim SW, Long-term follow up results of no initial therapy for ocular adnxeal MALT lymphomaAnn Oncol 2006 17:135-40. [Google Scholar]
[22]. Martinet S, Ozsahin M, Belkacémi Y, Landmann C, Poortmans P, Oehler C, Orbital lymphoma: Outcome and prognostic factors in eighty-eight consecutive patients treated with radiationtherapy. A rare cancer network studyInt J Rad Oncol Biol Phys 2000 48:216-17. [Google Scholar]
[23]. Raderer M, Vorbeck F, Formanek M, Osterreicher C, Valencak J, Penz M, Importance of extensive staging in patients with mucosa-associated lymphoid tissue (MALT)-type lymphomaBr J Cancer 2000 83:454-57. [Google Scholar]