Case Report
An adult 25-year-old male truck driver presented to Outpatient Department of ENT of All India Institute of Medical Sciences (AIIMS), Raipur, Chhattisgarh with fluctuant swelling over left medial canthal region of one week duration. He also complained of left side nasal obstruction. On examination pinkish fleshy masses were seen filling the left nasal cavity along with 3 by 2 cm fluctuant abscess over the medial canthal region [Table/Fig-1,2]. The provisional diagnosis of lacrimal abscess secondary to nasal pathology was made and patient consent was obtained. He had history of chronic dacryocystitis and surgery done for some swelling in the infra-orbital region nine months back, the details of which were not available with the patient. The patient was afebrile and there were no clinical signs of systemic involvement. Various serological and radiological investigations were advised viz., complete blood examination including Complete Blood Count (CBC), Erythrocyte Sedimentation Rate (ESR), HIV, Hepatitis B, C and Venereal Disease Research Laboratory (VDRL)/ Rapid Plasma Reagin (RPR) serology, Contrast Enhanced Computed Tomography (CECT) of nose Para Nasal Sinus (PNS). Approximately, 7cc pus from the medial canthal swelling was aspirated in a sterile tube and immediately sent to the Department of Microbiology for Gram’s staining, bacterial culture and anti-microbial sensitivity, Acid Fast Bacilli (AFB) staining and mycobacterial culture using Lowenstein Jensen (LJ) medium and fungal potassium hydroxide (KOH) examination and fungal culture on Sabouraud Dextrose Agar (SDA). Blood culture was not considered because patient was not febrile. Nasal mass biopsy was planned for histopathological examination after CT and blood investigations reports. The patient was started on oral amoxicillin-clavulanate 625mg TDS and was asked to come again after one week along with reports of all investigation for review. On his subsequent visit, the patient had reported that, swelling at medial canthal region was considerably reduced after aspiration. Patient had not got CECT nose paranasal sinus done due to his poor financial condition and drinking habits. CBC was found with in normal limits with RBC 5.35x106/μl, HGB 15.3 g/dL, Hematocrit (HCT) 46.8 %, Mean Corpuscular Volume (MCV) 87 fL, Mean Corpuscular Hemoglobin (MCH) 28.7 pg, MCHC 32.8 g/dL, Red Cell Distribution Width (RDW) 14.2% except for lower WBC count of 5000/μl and raised ESR of 58 mm/hr. Serological test confirmed HIV positive status of the patients and found negative for HBsAg, anti-HCV antibody and VDRL/RPR. Grams’ staining revealed abundant number of polymorphonuclear leucocyte with gram negative coccobacilli. Fungal KOH, AFB smear examination and their culture were found negative. He was sent for registration at the government designated Integrated Counselling and Testing Centre (ICTC) for anti-retroviral therapy and asked to follow-up with CT scan for nasal mass biopsy and incision and drainage of the medial canthal region with continuing the amoxicillin-clauvlanate for one more week. Unfortunately the patient did not return for follow-up.
Fluctuant swelling seen over left medial canthal region of one week duration and partially seen left side nasal fleshy mass.

Pinkish fleshy mass filling the left nasal cavity.

The pus was inoculated on both Blood agar and Mac-Conkey agar (BA and MA) and incubated at 370C for 24 hours. Next day cultural examination revealed a moderate growth of non-haemolytic, large, grayish white, smooth colonies on BA, whereas on MA agar, non-lactose fermenting, moist colonies were obtained [Table/Fig-3,4]. Smear examination from both MA and BA showed gram-negative Coccobacilli. The isolate was catalase and oxidase test positive. Considering it as presumptive non-fermenter, following battery of test was put up for identification [Table/Fig-5]. The biochemical identification confirmed this isolate as P.canis biovar 2 on the basis of Indole test which comes positive for biovar 1 and negative for biovar 2. Since, it’s a rare pathogen of abscess isolated from left medial canthal region, we referred the isolate for automated identification by Vitek 2 microbial identification system, Biomerieux, USA using GN card which also confirmed P.canis with excellent identification confidence level of 98% after eight hours of incubation. Fungal and tuberculosis investigation were found negative. Antibiotic susceptibility testing was done by Kirby-Bauer disk diffusion test following the CLSI guidelines, 2014 [1]. The organism was found sensitive to ampicillin, gentamycin, cefuroxime, cefotaxime, ciprofloxacin, amoxycillin-clavulanic acid, piperacillin and tetracycline.
Non haemolytic, smooth, grayish white colonies with pungent odour of P.canis on blood agar.
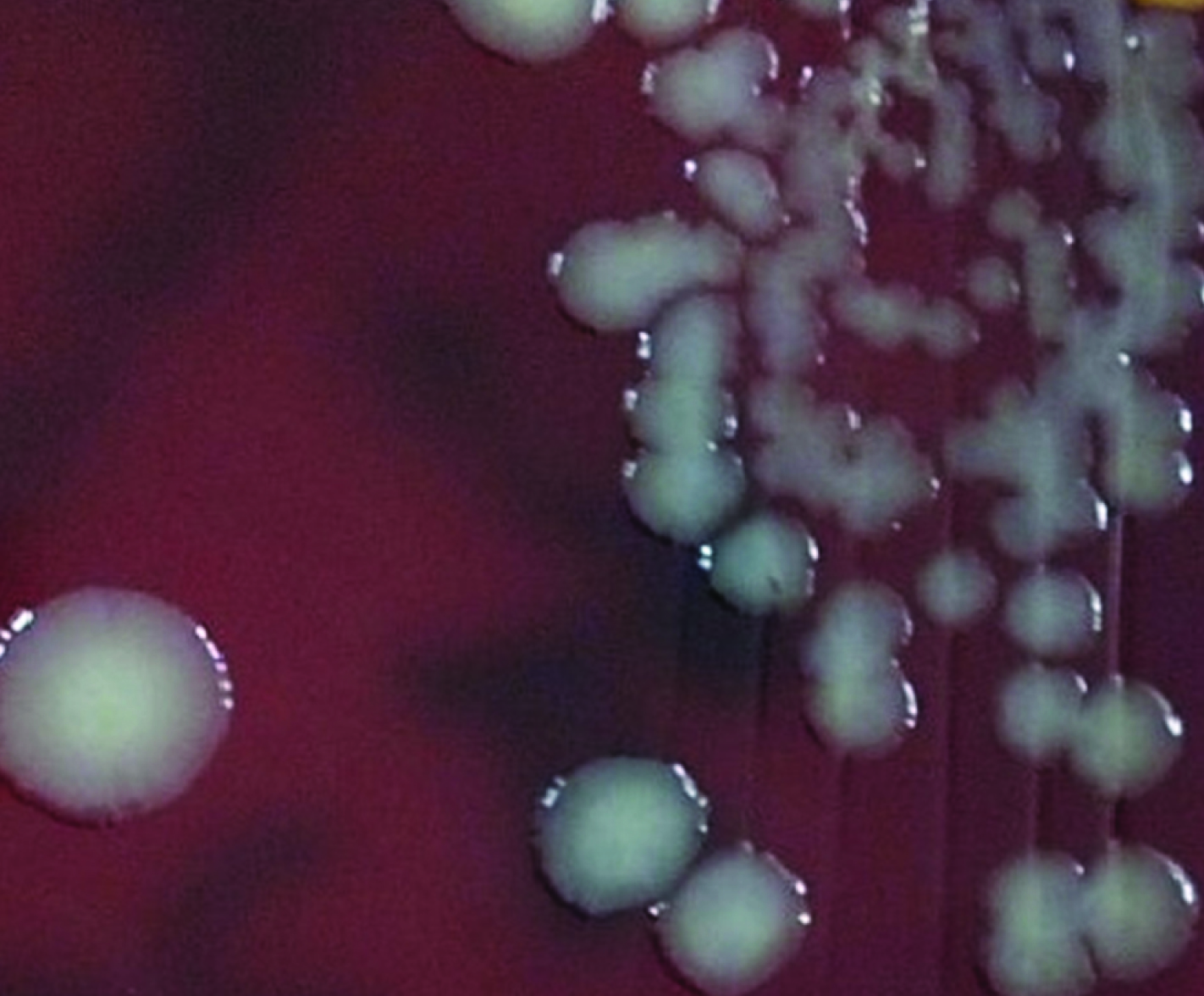
Nonlactose fermenting colonies of P.canis on mac-conkey agar.

List of biochemical tests put up for identification of the culture isolate and their results.
| S. No. | Test Name | Result |
|---|
| 1. | Oxidase | Positive |
| 2. | Catalase | Positive |
| 3. | Motility | Non-motile |
| 4. | Indole | Negative |
| 5. | Methyl Red | Negative |
| 6. | Voges-Prauskauer | Negative |
| 7. | Citrate | Negative |
| 8. | Urease | Negative |
| 9. | Bile esculin | Negative |
| 10. | Lysine, Arginine, Ornithine | Negative, Negative, Positive |
| 11. | Phosphatase | Positive |
| 12. | Nitrate reduction test | Positive |
| 13. | ONPG | Negative |
| 14. | Glucose | Fermented |
| 15. | Sucrose | Fermented |
| 16 | Maltose | Not fermented |
| 17 | Lactose | Not fermented |
| 17 | Mannitol | Not fermented |
| 18 | Fructose | Fermented |
| 19 | Mannose | Fermented |
Since, P.canis has been reported mostly following animal bite history, patient was enquired for any animal contact history on which he stated being involved in caring of cattle at his village farm. Literature search of P.canis in PUBMED retrieved 72 reports. Fifty three (53) studies restricted to animals and six (06) with characterisation of P.canis were excluded. Only 13 case studies were found relevant for review [2–14].
Discussion
More than 80% of HIV infected patients present with otorhinolaryngological and ocular manifestations at some point during the course of their disease [15,16]. ENT and ocular manifestations in HIV patients are however varied. People infected with HIV are prone to develop various infections by typical as well as atypical organisms.
P.canis, a gram negative non-motile coccobacillus or short rods belonging to Pasteurellaceae family is found as a part of normal oropharyngeal flora of many animals including healthy dogs and cats. P. canis although rarely affects humans and cause systemic zoonotic infection albeit its infection can be broadly classified into three categories on the basis of its mode of transmission [4,17]. The first category includes infection occurring after animal bite pre-dominantly of dog and cat with dog bite reported more commonly and infrequently by licking and scratches. The second category describes infection occurring after other animal exposure while third category included infection with no known animal contact history [4,17]. P.canis have been infrequently implicated in wound infection, cellulitis, bacteraemia, peritonitis, conjunctivitis, empyema, osteoarticular and lower respiratory tract infection mainly during two extremities of age but never been reported in HIV patients [2–9]. In fact, P.bettaye has exclusively been reported in HIV patients [18]. No literature was found for P.canis infection in HIV patients supporting our claim of this case report as one of the rarest finding.
To the best of our knowledge, this is probably the first report of isolation of P.canis from abscess in the left nasolacrimal sac region from a HIV positive patient of chronic dacryocystitis without any dog or cat bite history. How this P.canis has colonized canthal region and caused abscess was really interesting to explore. The most probable reason could be initial nasopharyngeal colonization via inhalation after close contact with cattle. Bhat S et al., have also reported the inhalation route of transmission of P.canis [5]. Once colonized, probably the leukotoxin production had stimulated cytokine release in exaggerated manner leading to inflammation and abscess formation amid impaired cellular response due to HIV infection. Since, the patient did not return for follow-up, we could not get the histopathological examination of the pink fleshy nasal masses done leaving the speculation wide open whether P.canis isolated of abscess from left medial canthal region could also be the reason of pinkish fleshy mass in the left nasal cavity or vice-versa. Although lack of histopathological examination is a major limitation of this study, the mainstay of this case report of novel finding of P.canis from left medial canthal region prompted us to share this unusual extended spectrum of infective capacity of P.canis.
Literature search of various human infection by P.canis in PUBMED retrieved 13 case reports [Table/Fig-6] [2–14]. On comparison, we found that infrequent reports of P.canis infection due to animal exposure other than dog and cat bite have been reported to support our hypothesis of transmission of P.canis after close contact with other animals. Yefet E et al., reported P.canis associated bacteraemia in a child after exposure to rabbit secretions [6]. Castellano et al., reported, P.canis associated peritonitis in a peritoneal dialysis patient without animal bite history [8]. Hazelton BJ et al., reported P.canis associated osteomyelitis and septic arthritis in 14 and 19 month old girl respectively without any history of penetrating dog bite [2]. Casallas-Rivera N et al., reported haemorrhagic sepsis and empyema in a 56-year-old female patient without epidemiological background [7]. All the reported cases led to the important finding that P. canis is an opportunistic pathogen which cause multi-varied infection in humans after exposure to animal bite, scratches, licking or close contact and even in cases without animal contacts. Majority of these cases were from extreme of the ages either children or old age people and predominantly suffering with some underlying disease, although not always true. All the cases showed sufficient sensitivity of P.canis to various anti-microbial with complete recovery of their patients and amoxicillin-clavulanate was the drug of choice in majority of the reported cases [2–14].
Comparative study of the various case reports of P.canis infection in indexed Journal of Pubmed.
| Study [Reference No.] | Case detail | Diagnosis | Transmission route | Underlying disease | Treatment | Outcome |
|---|
| Casallas-Rivera M et al., [7] | 56 Yr, Female | Hemorrhagic septicaemia with secondary pleural empyema | Unknown (No animal contact) | Hypertension and hypothyroidism | Piperacillin-Tazobactam | Recovered |
| Bhat S et al., [5] | 70 Yr, Male | Lower respiratory tract infection | Exposure to domestic cats | COPD and ischaemic heart disease | Doxycycline | Recovered |
| Gundluru R et al., [11] | 16 Yr, Female | Peritonitis | Patting of peritoneal catheter by cat | Peritoneal dialysis for end stage renal disease | Cefepime | Recovered |
| Castellano I et al., [8] | 65 Yr, Male | Peritonitis | Dog contact | Continuous cycling peritoneal dialysis | Vancomycin and Gentamycin | Recovered |
| Hazelton BJ et al., [2] | 14 Month, female | Osteomyelitis and synovitis of Left ankle joint | Dog licking on face | None | Amoxicillin- Clavulanate | Recovered |
| 19 Month, Female | Septic arthritis of right elbow | Dog licking on face | None | Amoxicillin- Clavulanate | Recovered |
| Kaftandzieva A et al., [9] | 55 Yr, Female | Right leg wound | Dog bite | None | Amoxicillin- Clavulanate | Recovered |
| Yimaz MB et al., [13]a | 14 children with median age 3 month | Conjunctivitis | NA | NA | Vancomycin and Gentamycin | Recovered |
| Rashid NK et al., [4] | 3 Yr, Male | Superonasal conjunctival laceration and scleral perforation | Left eye trauma with coconut skewer broom stick contaminated by cat | None | Ciprofloxacin | Recovered |
| Akhane T et al., [3] | 25 Yr, Female | Dog bite wound | Dog bite | None | Cefazolin/Cefcapene pivoxil | Recovered |
| Yefet E et al., [6]a | 21 Month, | Bacteraemia | Rabbit secretion | None | NA (in Hebrew) | Recovered |
| Albert TJ and Steven DL [10] | 74Yr, male | Bacteraemia | Dog lick to open leg wound | Alcholic cirrhosis | Amoxicillin- Clavulanate | Recovered |
| Hara H et al., [12]a | NA | Osteomyelitis and cutaneous abscess | Dog bite | None | NA | Recovered |
| Mondon D et al., [14]a | NA | Total knee arthroplasty infection | NA | NA | NA | NA |
a and NA = Not fully accessed due as not available freely online except abstract.
P.canis is divided into two biotypes: biotype 1 is found in the oral cavity of dogs, whereas, biotype 2 has been received from calves [5]. As our isolate was negative for indole test which is the criteria of distinguishing biotype 2 (indole negative) from Biotype 1 (Indole positive), we designated it as P.canis biotype 2 correlating well with the clinical history of the patient involvement in care of cattles.
We found the susceptibility of the isolate to ampicillin, gentamycin, cefuroxime, cefotaxime, ciprofloxacin, amoxycillin- clavulanic acid, piperacillin and tetracycline supporting the notion that Pasteurella spp are not great resistance exhibiting organism [3–9]. Several decades of clinical experiences with Pasteurella and numerous in vitro studies including ours suggested, penicillin as the best anti-microbial agent for the treatment of virtually all forms of infection [17]. Aminopenicillin, oral (cefuroxime and cefixime) and parenteral cephalosporin (ceftriaxone and cefoperazone) have been reported as excellent invitro activity [17]. Among non-β-lactam antibiotics, trimethoprim-sulfamethoxazole, fluoroquinolones and tetracyline showed good invitro activity [17]. However, occasional clinical failures have been documented to P.multocida against various anti-microbials including oral macrolides (e.g., erythromycin), semi-synthetic penicillins (e.g., oxacillin, dicloxacillin), first generation cephalosporins (e.g., cephalothin, cephalexin, cefadroxil) and clindamycin [3–9].
Pasteurella infections although considered often amid history of dog or cat bite, our and some published studies strongly advocated that, it also should not be ignored even in absence of animal bite history. Timely and accurate identification proved pivotal in giving rarest insight spectrum of infective capacity of P.canis and evidence based anti-microbial treatment to prevent any further complications.
Conclusion
The potential spectrum of clinical manifestation caused by P.canis even without prior penetrating injury is more extensive than had been thought previously especially in immunocompromised patients where in early accurate identification and evidence based antimicrobial therapy may prevent any further complication.
a and NA = Not fully accessed due as not available freely online except abstract.
[1]. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. Twenty-Fourth Informational Supplement. CLSI document; 2014. M100-S24 [Google Scholar]
[2]. Hazelton BJ, Axt MW, Jones CA, Pasteurella canis osteoarticular infections in childhood: Review of bone and joint infections due to Pasteurella species over 10 years at a tertiary pediatric hospital and in the literatureJ Pediatr Orthop 2013 33:e33-8. [Google Scholar]
[3]. Akahane T, Nagata M, Matsumoto T, Murayama N, Isaka A, Kameda T, A case of wound dual infection with Pasteurella dagmatis and Pasteurella canis resulting from a dog bite- limitations of Vitek-2 system in exact identification of Pasteurella speciesEur J Med Res 2011 16:531-36. [Google Scholar]
[4]. Rashid NK, Zam Z, MdNoor SS, SitiRaihan I, Azhany Y, Pasteurella canis isolation following penetrating eye injury: A case reportOphthalmol Med 2012 2012:362-69. [Google Scholar]
[5]. Bhat S, Acharya PR, Biranthabail D, Rangnekar A, Shiragavi S, A case of lower respiratory tract infection with canine associated Pasteurella canis in a patient with chronic obstructive pulmonary diseaseJ Cli Diag Res 2015 9:DD03-4. [Google Scholar]
[6]. Yefet E, Abozaid S, Nasser W, Peretz A, Zarfin Y, Unusual infection-Pasteurella canis bacteraemia in a child after exposure to rabbit secretionHarefuah 2011 150:13-5. [Google Scholar]
[7]. Casallas-Rivera M, Faccini Martinez A, Perdomo-Beltran N, Botero-Garcia C, Bravo J, Perez-Diaz C, Pasteurella canis haemorrhagic sepsis and empyemaRev Chilena Infectol 2016 33:85-8. [Google Scholar]
[8]. Castellano I, Martin JP, Gallego S, Mora M, Rangel G, Suarez MA, Pasteurella canis peritonitis in a peritoneal dialysis patientPerit Dial Int 2011 31:503-04. [Google Scholar]
[9]. Kaftandzieva A, Peneva M, Petrovska B, Cekovska Z, Pasteurella canis as a cause of soft tissue infection after dog bite: A case reportMaced J Med Sci 2013 6:74-8. [Google Scholar]
[10]. Albert TJ, Steven DL, The first case of Pasteurella canis bacteraemia: A cirrhotic patient with an open leg woundInfection 2010 38:483-85. [Google Scholar]
[11]. Gundluru R, Bheemanathini P, Yaseen R, Pasteurella canis peritonitis in a child on peritoneal dialysisPediatr Infect Dis J 2015 34:332 [Google Scholar]
[12]. Hara H, Ochiai T, Morishima T, Arashima Y, Kumasaka K, Kawano KY, Pasteurella canis osteomyelitis and cutaneous abscess after a domestic dog biteJ Am Acad Dermatol 2002 46:S151-52. [Google Scholar]
[13]. Yimaz MB, Tolya Y, Esen AB, Engin KN, Taskapali M, Pasteurella canis and Granulicatella adiacens conjunctivitis outbreak resistant to empirical treatment in a child welfare agencyJ Pediatr Ophthalmol Strabismus 2012 49:314-19. [Google Scholar]
[14]. Mondon D, Bouillet B, Lesens O, Descamps S, First report of a total knee arthroplasty infected by Pasteurella canisMed Mal Infect 2010 40:600-01. [Google Scholar]
[15]. Prasad HK, Bhojwani KM, Shenoy V, Prasad SC, HIV manifestations in otolaryngologyAm J Otolaryngol 2006 27:179-85. [Google Scholar]
[16]. Moazzez AH, Alvi A, Head and neck manifestations of AIDS in adultsAm Fam Physician 1998 57:1813-1822. [Google Scholar]
[17]. Mandell GL, Doughlas RG, Bennet JE, “Pasteurella species” in principles and practice of infectious diseases 2005 6th edNew York, NY, USAChurchill Livingstone:2687-2691. [Google Scholar]
[18]. Holst E, Rollof J, Larsson L, Nielsen JP, Characterisation and distribution of Pasteurella species recovered from infected humansJ Clin Microbiol 1992 30:2984-87. [Google Scholar]