Utilization of Intraoperative Real-time Three-Dimensional Transoesophageal Echocardiography to Objectively Assess Improvement in Synchronization and Regional Wall Motion after Coronary Reperfusion
Abhishek Karnwal1, Clinton Z Kakazu2, Sonia Shah3, Bassim Omari4, Charu Dutt Arora5
1 Assistant Professor, Department of Anaesthesiology Critical Care Medicine, Children’s Hospital Los Angeles, California, USA.
2 Associate Professor, Department of Anaesthesiology, Harbor-UCLA Medical Center, Torrance, California, USA.
3 Assistant Professor, Department of Cardiology, Harbor-UCLA Medical Center, Torrance, California, USA.
4 Assistant Professor, Department of Cardiothoracic Surgery, Harbor-UCLA Medical Center, Torrance, California, USA.
5 Research Assistant, Department of Anesthesiology, Critical Care Medicine, Children’s Hospital, Los Angeles, California, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhishek Karnwal, 4650 Sunset Blvd, MS#12, Los Angeles, California-90027, USA.
E-mail: karnwal@gmail.com
It is well known that myocardial ischemia leads to Regional Wall Motion Abnormalities (RWMAs) and reversible depression of Left Ventricular (LV) systolic function. Transoesophageal Echocardiography (TEE) is an established tool for early diagnosis of new RWMAs. However, evaluation of RWMAs by echocardiography is largely qualitative and relies on visual assessment of wall segments. Evaluation of LV systolic function and Ejection Fraction (EF) is more reproducible and accurate with Real-Time 3D Echocardiography (RT3DE) as compared with two-dimensional and M-mode techniques. Primary advantages for RT3DE are fast and largely automated volumetric analysis of LV function and LV volumes, without geometric assumptions and risk of underestimating volumes in foreshortened views. This case illustrates the use of intraoperative RT3DE during coronary artery bypass surgery to objectively assess: LV systolic function with LV volumes and RWMAs and improvement in cardiac synchronization following coronary reperfusion.
Myocardial ischemia, Myocardial reperfusion angina, Unstable echocardiography, Three-Dimensional Co
Case Report
A 50-year-old female presented to Harbor-UCLA Medical Center, Los Angels, United States with unstable angina. Cardiac catheterization and left ventriculogram revealed occlusion of the proximal Left Anterior Descending (LAD) Artery with a right to left collateral filling of the distal LAD. Other coronary arteries did not show significant occlusion. Transthoracic Echocardiogram (TTE) showed mildly reduced left ventricular systolic function with an Left Ventricular Ejection Fraction (LVEF) of 40-45% and RWMAs involving basal to mid-anterior and anteroseptal walls. She subsequently underwent a single vessel off-pump Left Internal Mammary Artery (LIMA) to LAD bypass. Prior to induction of anaesthesia, standard American Society of Anaesthesiologists (ASA) monitors, left radial arterial and a pulmonary artery catheter were placed uneventfully. Anaesthesia was induced and maintained with titrated doses of fentanyl, midazolam, rocuronium and sevoflurane. The patient remained haemodynamically stable throughout the surgery and was transferred to the cardiothoracic Intesive Care Unit (ICU) for postoperative care without requiring any vasopressor drugs.
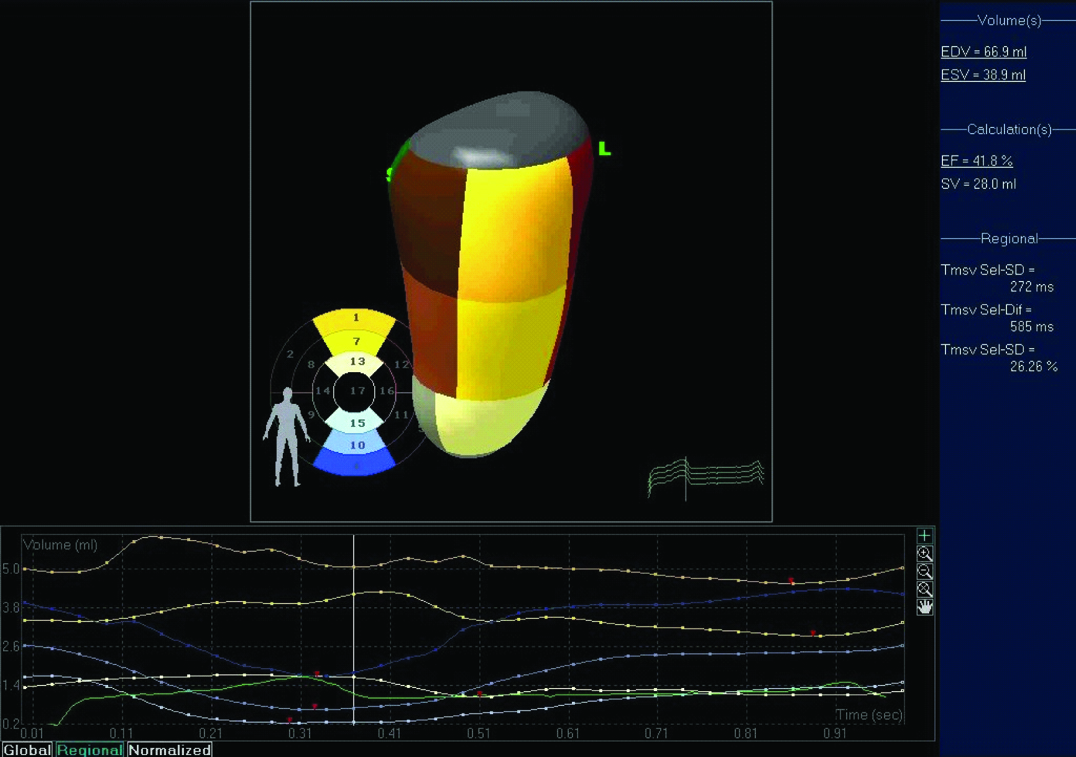
An intraoperative TEE was performed based on the guidelines from Society of Cardiovascular Anaesthesiologists/ American Society of Anaesthesiologists [1], initially after induction and subsequently 30 minutes after coronary reperfusion. A multiplane phased array TEE probe (X7-2t transducer) was used and images acquired on a Phillips iE33 xMatrix Ultrasound Imaging System (Phillips Medical Systems, Bothell, Washington). A wide-angle acquisition “full volume” mode, in which 4 wedge-shape sub-volumes were acquired over four consecutive cardiac cycles, during a single breath-hold to avoid “stitch artifact”. Special care was taken to include the entire LV cavity within the pyramidal 3D volume. Optimization of images for endocardial visualization, gain modification, compression and time-gain compression controlling was performed before the 3D volume acquisition. Digital RT3DE images were analyzed intraoperatively using prototype software (QLAB, 3DQ-Advance, Philips Medical Systems). First, 2-and 4-chamber views with the largest long axis dimension were selected from the RT3DE pyramidal data set in end-diastole. In these 2 planes, 5 points, including 4 on the mitral annulus (2 on each plane) and the apex on either plane, were manually initialized to define the endocardial border. The automated endocardial border detection traced the LV cavity in end diastole and the voxel count inside the LV cast derived the End-Diastolic Volume (EDV). The same process was repeated for the end-systolic frame, which was identified by the frame with the smallest LV cavity, deriving the End- Systolic Volume (ESV). After the automated processing of all the RT3DE frames throughout one cardiac cycle, the pre-bypass LV cast reconstruction model [Table/Fig-1] was obtained. Computer generated baseline ejection fraction was calculated at 41.8% based on measurements from EDV and ESV ([Table/Fig-1]- far-right margin). The accompanying end diastolic volume percent (% EDV) plotted against time (seconds) during one cardiac cycle confirmed the anterior wall motion abnormality seen preoperatively. [Table/Fig-1], corresponding to segments 1, 7 and 13 on the 17 segment model. The minimal change in EDV was noted in segments 1 and 7 corresponding to RWMA in the basal and mid anterior wall. Segments 4, 10, and 15 corresponding to the inferior wall were normal and are shown for comparison.
Pre coronary bypass intraoperative 3D TEE LV cast reconstruction image.
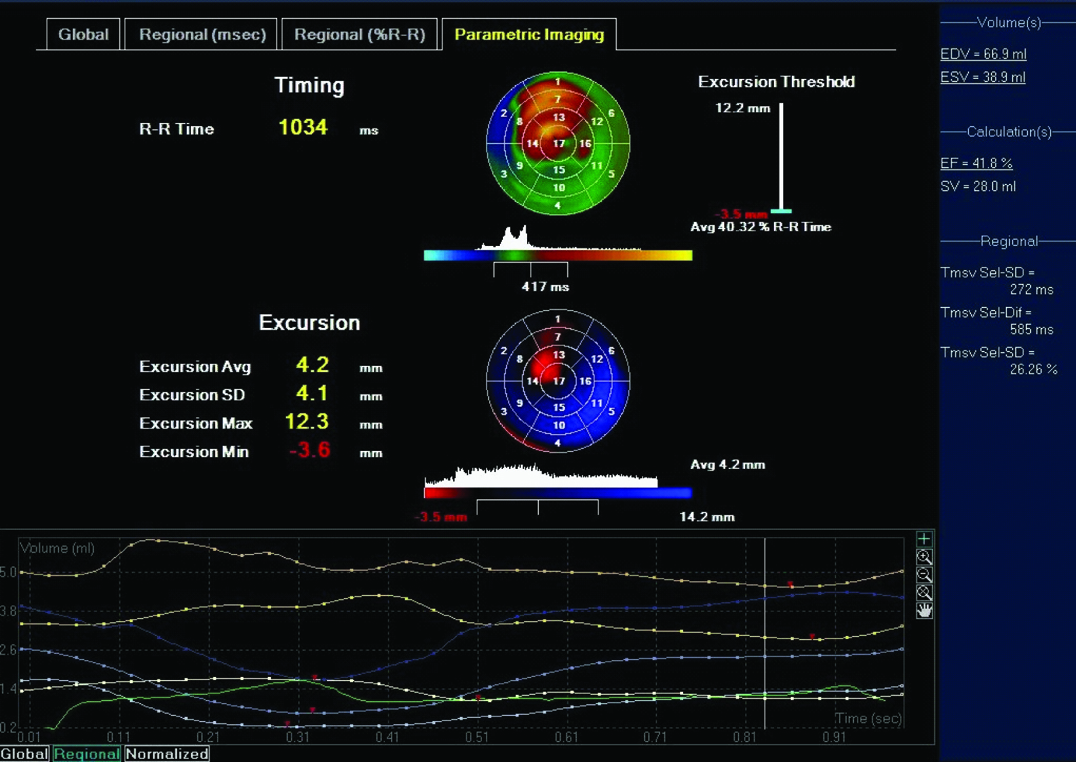
The pre-bypass parametric image [Table/Fig-2] shows dyssynchrony (in red) of the anterior wall segments in the LAD territory (timing: top bulls-eye). There are hypokinesis and dyskinesis (in red and black) consistent with ischemia in the corresponding segments (wall excursion: bottom bulls-eye.)
Pre coronary bypass parametric image (bottom).
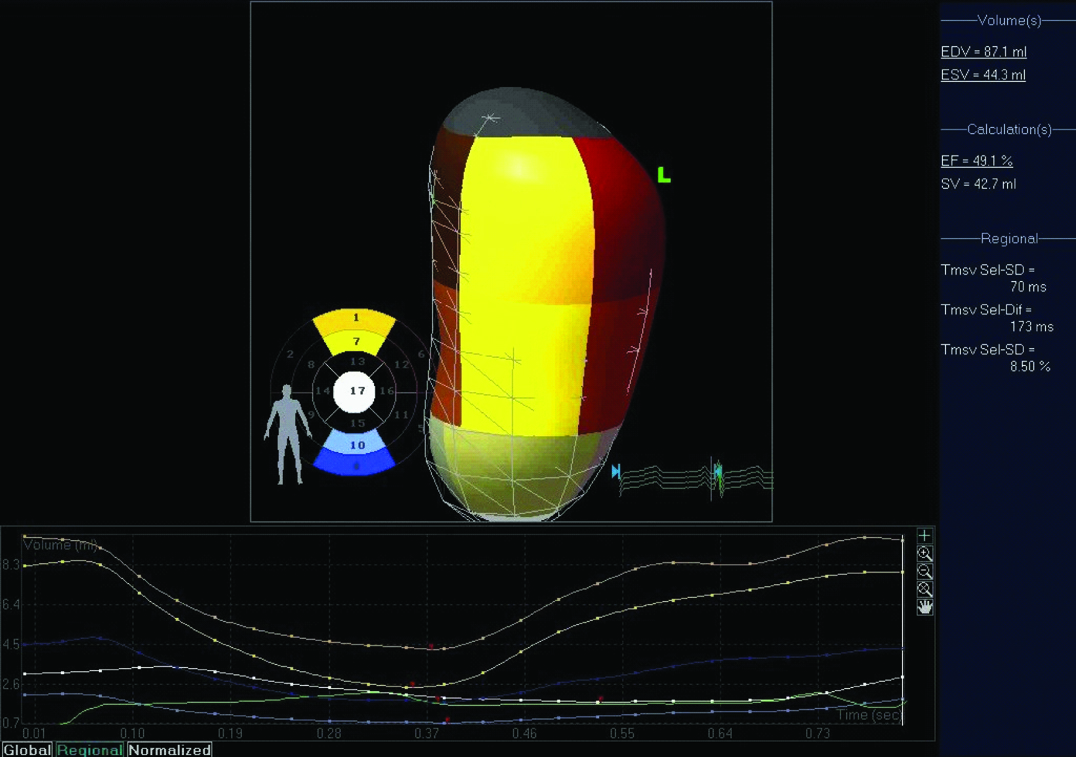
Following off-pump coronary bypass of LIMA to LAD, a “full volume” LV acquisition was performed and analysis was carried out in a similar fashion using QLAB and 3DQ-Advance software. Significant improvement in anterior wall motion and synchronization in myocardial segments were noted. The LV function also improved from 41% at baseline to 49% post-reperfusion. The segmental EDV loops directly showed improved segmental wall motion when compared to the baseline [Table/Fig-3].
Post-coronary bypass intraoperative 3D TEE LV cast reconstruction image.
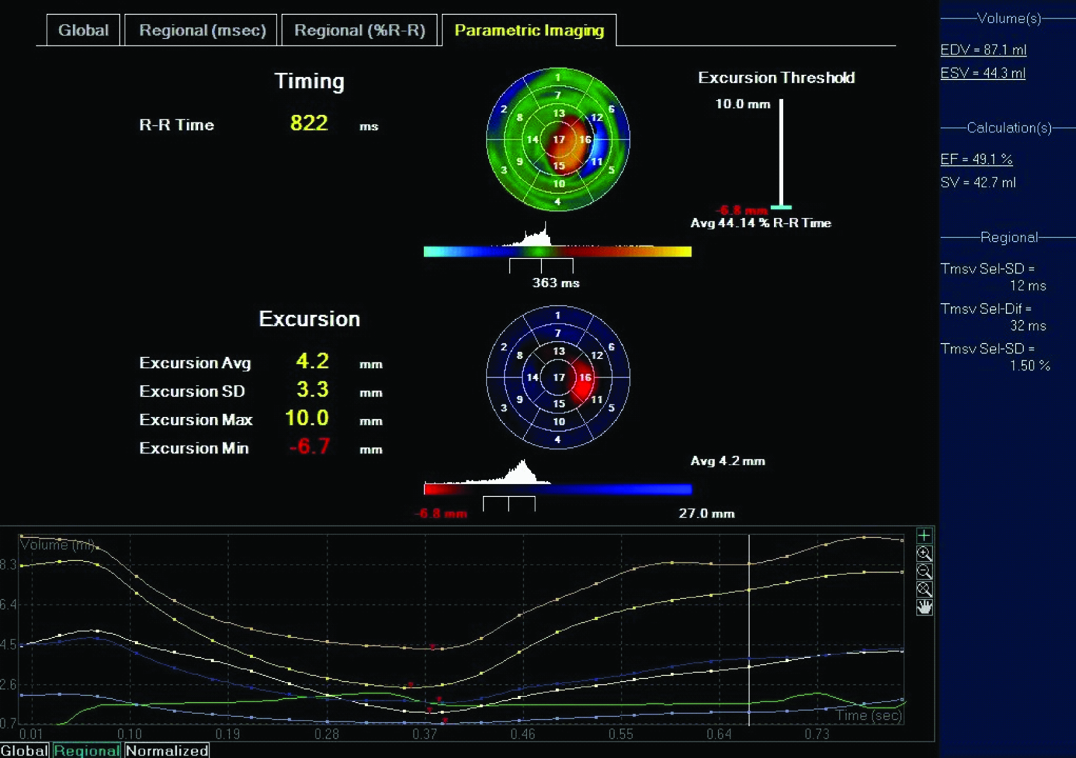
The post-bypass parametric image [Table/Fig-4] showed improved synchrony, in green, and wall motion, in blue, for the LAD territory. A new area of timing and excursion abnormality was noted in segment 16. This correlates with the anatomical site of placement of the apical suction cup used for elevation and stabilization of the heart during off-pump coronary bypass.
Post-coronary bypass parametric image.
Discussion
Since myocardial ischemia is well known to cause RWMAs and reversible depression of LV systolic function [2], and TEE is an established tool for early diagnosis of new RWMAs [3], thus, evaluation of LV systolic function and EF is more reproducible and accurate with RT3DE as compared with 2-dimensional and M-mode techniques [3,4]. RT3D TEE is a beneficial intraoperative tool for quantitative assessment of LV systolic function and regional wall motion after coronary reperfusion. Using RT3DE, we were able to perform an objective assessment of LVEF and wall motion and subsequently demonstrate improvement after re-vascularization. At full volume data set of the LV allowed for quantification of the LVEF and abnormal segmental wall motion, consistent with ischemia in the LAD territory. Parametric imaging supported this finding, revealing abnormal timing and extent of segmental contraction in the anterior wall.
As the patient did not require any vasoactive drugs after reperfusion, it can be concluded that, improved synchronization, segmental wall motion, and LVEF were a direct effect of coronary reperfusion. Further, studies are needed to validate the utility of intraoperative RT3D TEE to directly assess the effects of coronary reperfusion on segmental wall motion, synchronization as well as ejection fraction.
Conclusion
The case presented above illustrates the use of intraoperative RT3DE during coronary artery bypass surgery in assessing the LV systolic function with LV volumes and RWMAs and improvement in cardiac synchronization following coronary reperfusion. A larger case series is important to validate our finding. We are currently conducting a prospective case series to validate the same.
[1]. American Society of Anaesthesiologists and Society of Cardiovascular Anaesthesiologists, Practice guidelines for perioperative Transesophageal echocardiographyPractice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal EchocardiographyAnaesthesiology 2010 112:1084-96. [Google Scholar]
[2]. Awan M, Khan A, Siddiqi T, Hussain A, Rabbi F, Tasneem H, Early effects of coronary artery bypass grafting on left ventricular regional wall motion abnormalitiesJ Coll Physicians Surg Pak 2007 17(1):3-7. [Google Scholar]
[3]. Swaminathan M, Morris RW, De Meyts DD, Podgoreanu MV, Jollis JG, Grocott HP, Deterioration of regional wall motion immediately after coronary artery bypass graft surgery is associated with long-term major adverse cardiac eventsAnaesthesiology 2007 107(5):739-45. [Google Scholar]
[4]. Lang RM, Vignon P, Weinert L, Bednarz J, Korcarz C, Sandelski J, Echocardiographic quantification of regional left ventricular wall motion with color kinesisCirculation 1996 93:1877-85. [Google Scholar]