Introduction
Nuchal Translucency (NT) is the sonographic form of subcutaneous gathering of liquid behind the foetal neck in the first trimester of pregnancy. There is association of increased NT with chromosomal and non-chromosomal abnormalities.
Aim
The purpose of this systemic review was to review the pregnancy outcome of abnormal nuchal translucency.
Materials and Methods
The present systematic review was conducted by searching English language articles from sources such as International Medical Sciences, Medline, Web of science, Scopus, Google Scholar, PubMed, Index Copernicus, DOAJ, EBSCO-CINAHL. Persian articles were searched from Iranmedex and SID sources. Related key words were “outcome”, “pregnancy”, “abnormal”, and “Nuchal Translucency” (NT). All, randomized, descriptive, analytic-descriptive, case control study conducted during 1997-2015 were included.
Results
Including duplicate articles, 95 related articles were found. After reviewing article titles, 30 unrelated article and abstracts were removed, and 65 articles were evaluated of which 30 articles were duplicate. Finally 22 articles were selected for final analysis. Exclusion criteria were, case studies and reports and quasi experimental designs. This evaluation has optioned negative relationship between nuchal translucency and pregnancy result. Rate of cardiac, chromosomal and other defects are correlated with increased NT≥2.5mm. Cardiac disease which were associated to the increased NT are heart murmur, systolic organic murmur, Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD), tricuspid valve insufficiency and pulmonary valve insufficiency, Inferior Vena Cava (IVC) and Patent Ductus Arteriosus (PDA). The most common problems that related with increased NT were allergic symptoms.
Conclusion
According to this systematic review, increased NT is associated with various foetal defects. To verify the presence of malformations, birth defect consultations with a perinatologist and additional tests are required.
Introduction
Ultrasonography is regularly used for prenatal care because it allows examination of foetal health in the early stages of pregnancy [1,2]. Nuchal Translucency (NT) is the sonographic appearance of subcutaneous accumulation of liquid in the back of the foetal neck in the first trimester of pregnancy (11-14 gestational weeks of pregnancy). NT measurement is an excellent and sensitive screening test for foetal chromosomal abnormalities. The aetiology for the phenomenon includes cardiac failure secondary to structural malformation, disorders in the extracellular matrix, and unusual or delayed development of the lymphatic system. NT is detected in about 5% of the foetuses during screening. NT size above the 95th centile is said to be an increased NT, the thickness of which is based on Crown Rump Length (CRL). CRL is undetected in 5% of the screened foetuses, increasing NT thickness is based on the CRL [1,2]. At minimum CRL (45 mm) and maximum CRL (84 mm) in gestational age 11 to 13 + 6 weeks, NT is between the 50th percentile and 95th percentile. There is an association between increased NT and chromosomal and non-chromosomal abnormalities [2–7]. Prevalence of abortion, foetal death and foetal anomalies increase exponentially with NT thickness [8]. Increasing NT is associated with the risk of a broad spectrum of congenital anomalies, varying from isolated structural deficiencies to genetic diseases and neurodevelopmental delay, which often become manifest in the first years of life [4–6]. Increasing NT is a reason to identify the number of developmental delay. Many of syndromes associated with an increased NT (such as chromosomal abnormality) can cause developmental defect in neonates [8]. Thus, determining the outcomes of foetuses with increased NT is necessary. As primary searches in the available databases show no systematic studies evaluating the pregnancy outcomes of abnormal NT, the main purpose of this study was to explore the outcomes of this abnormality.
Materials and Methods
Literature Search Criteria
English-language databases, including International Medical Sciences, Medline, Web of Science, Scopus, Google Scholar, PubMed, Index Copernicus, DOAJ, EBSCO-CINAHL, as well as Persian-language databases, including Magiran, were searched using keywords such as “NT,” “abnormal,” “outcome,” “pregnancy,” “increased,” “foetal,” and “Nuchal translucency.” The searches were performed using the Boolean operators OR and AND between main phrases and the keywords were obtained from particular matters of the topic under study. Furthermore, relevant keywords and Boolean operators were selected to modify the search strategy in each database. No language preference was specified during the database searches or applied during evaluation of the obtained studies’ reference lists.
Inclusion and Exclusion Criteria
This paper included all published articles from 1997 to 2016. All randomized, descriptive, analytic–descriptive and case control study conducted during 1997 to 2015 was included. Exclusion criteria were, case studies and reports and quasi experimental designs.
Data Collection
Independent searches were performed by two researchers from April 2016 to May 2016. If disagreement between authors was encountered, a third researcher was consulted to resolve this disagreement. The Strengthening the reporting of observational studies in epidemiology (STROBE) check list was used [9] to evaluate standard reporting quality in the obtained articles and studies with a quality assessment below 60% were excluded from this work.
Assessment of Study Quality
The Cochrane Risk of Bias Tool [10] was used for bias assessment.
Results
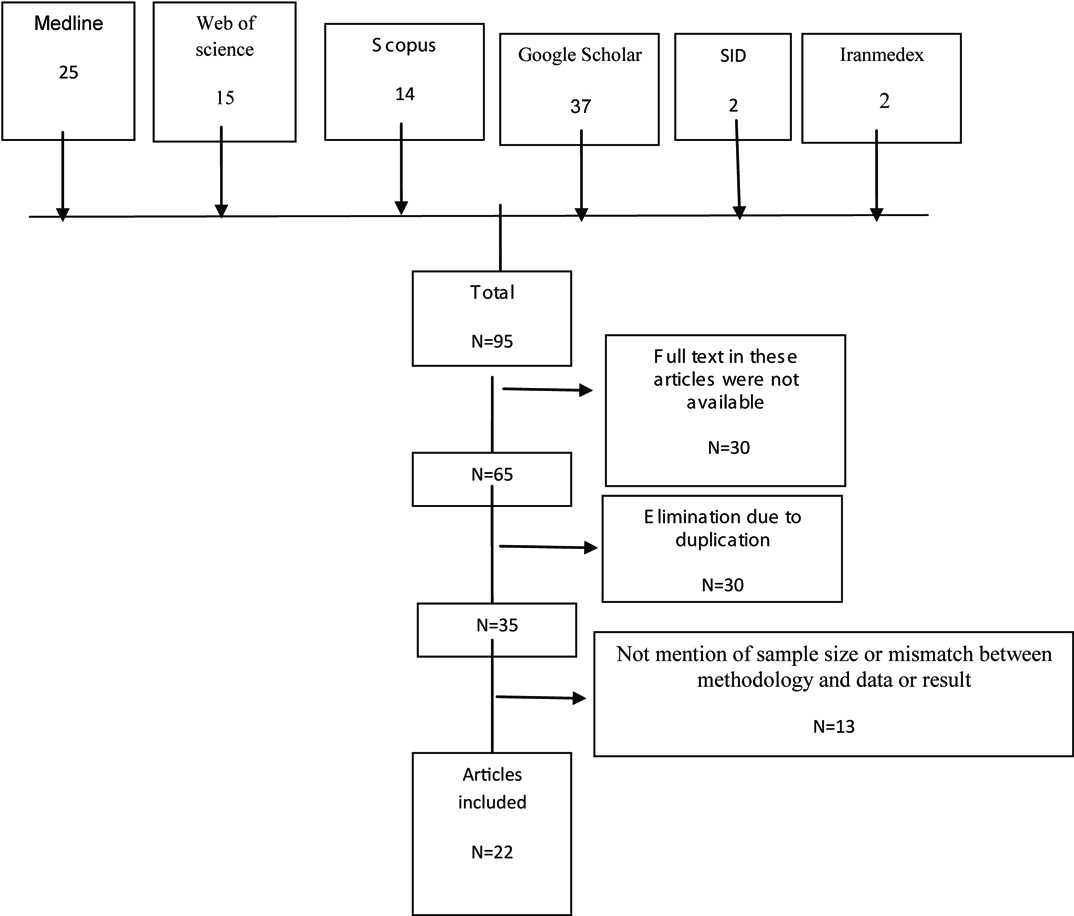
Including duplicate articles, 95 related articles were found. After reviewing article titles, 30 unrelated article and abstracts were removed and 65 articles were evaluated of which 30 articles were duplicate. Finally, 35 articles were analysed. Thirteen articles had no mention of sample size or there was mismatch between methodologies, data or results, finally twenty two articles were selected for final analysis [Table/Fig-1]. Results of study review are summarized in [Table/Fig-2] [11–32].
Flowchart of the search results.
Details of the studies used for analysis [11–32].
| Authors | Type of study | Method | Result | STROBE score |
|---|
| GHI T et al., [11] 2001 | Cross-sectional | Echocardiography was performed in 1319 chromosomally normal foetuses with increased NT. The incidence of major cardiac defects was examined. | Major cardiac defects were in 4.5% of foetuses with a nuchal translucency thickness in the range of 2.5-3.4 mm. | 18 |
| Zosmer N et al., [12] 1999 | Cross-sectional | Echocardiography was performed in 398 chromosomally normal foetuses with NT above the 2 mm, scan was carried out at 17-22 weeks and 20-22 weeks. Pregnancy outcome was obtained in all of the cases. | Major cardiac defects were present in 29 cases. Echocardiography was carried out at 13-17 weeks and an abnormality was suspected in 24 of the cases. | 18 |
| Hiippala A et al., [13] 2001 | Cohort | Clinical examination and detailed cardiac evaluation were carried out in 50 chromosomally normal children at the age of 2.4-7.1 years who had a nuchal translucency measurement of ≥ 3 mm at 13–15 weeks’ gestation. | Major cardiac defects were identified in 8% of the children. The growth of all children was within normal limits. One child had Noonan syndrome, one had a cleidocranial dysplasia and a third had a developmental delay together with an unrecognized syndrome. Webs in the neck region were noticed in two children, with no associated pathology. | 17 |
| Vieira LA et al., [14] 2013 | Cross-sectional | Foetuses with an NT above P95 and a normal karyotype were analyzed. Postnatal echocardiography (ECHO), weight, length and Apgar score at birth, and neuropsychomotor development by the ages and stages questionnaire evaluated. | Abortion, foetal death, several structural abnormalities and IVC was shown, postnatal echocardiography revealed the persistence of IVC in one case and one case of Atrial Septal Defect (ASD) and Patent Ductus Arteriosus (PDA). Of the 40 surviving children, only one showed delayed speech development and another presented autism. | 18 |
| Matias A et al., [15] 1998 | Cross-sectional | Ductusvenosus flow velocity waveforms were obtained immediately before foetal karyotyping in 486 consecutive singleton pregnancies at 10–14 weeks of gestation. All cases were screened for chromosomal defects by a combination of maternal age and foetal nuchal translucency thickness. | There were 63 chromosomal defects trisomy 18, seven cases of trisomy 13, three cases of Turner’s syndrome and three cases of triploidy. In 57 cases there was reverse or absent flow during atrial contraction. Abnormal ductusvenosus flow was also observed in 13 (3.1%) of the 423 chromosomally normal foetuses. | 16 |
| Jauniaux E et al., [16] 1996 | Cross-sectional | Foetal heart rate, umbilical artery pulsatility index, end diastolic flow, nuchal translucency thickness and placenta! thickness were recorded in 250 women with a viable singleton pregnancy undergoing chorionic villous sampling for foetal karyotyping at 11-14 weeks of gestation | The foetal karyotype was normal in 210 cases and abnormal in 40, including 21 with trisomy 21, 13 with trisomy 18, three with triploidy, two with monosomy X and one with trisomy 13. | 17 |
| Maymon R et al., [17] 2000 | cohort | Long-term pregnancy outcome and infancy prognosis of 78 fetuses with NT > 95th centile of the normal range for Crown–Rump Length (CRL) assess. | In 40% of the cases increased NT related to chromosomal abnormality. The chance of a normal outcome dropped to 50% in four cases with maternal age ≥30 years and NT ≥5 mm. | 17 |
| Schwarzler et al., [18] 1999 | Prospective. | Measurements of crown–rump length and NT. Pregnancy outcome was obtained through karyotyping, outcome questionnaires and examination of the newborn infants. | Screening was positive in 5.1% foetuses. Foetal karyotype was abnormal in 23 cases, including twelve with trisomy 21, five trisomy 18, one trisomy 13, one trisomy 10, one monosomy X and two triploidies. Only one out of nine major congenital heart defects in this population was found. | 16 |
| Westin M et al., [19] 2006 | Cross-sectional study | An NT measurement was made in 16, 383 consecutive euploid foetuses derived from an unselected pregnant population. | A total of 127 cases with a diagnosis of heart defect confirmed by cardiac investigations after birth or at autopsy. Of these, 55 defects were defined as major, of which 52 were isolated, corresponding to a prevalence of major heart defects in chromosomally. NT >or= 95th centile with regard to an isolated major heart defect. | 21 |
| Zoppi MA et al., [20] 2001 | Cohort | Foetal NT thickness and crown rump length were measured at 10–14 weeks of gestation in 12, 495 pregnancies. | There were 64 foetuses with trisomy 21 and 46 with other chromosomal defects. In 184 multiple pregnancies, there were four foetuses with chromosomal abnormalities. | 19 |
| Nicolides KH et al., [21] 2005 | Cross-sectional study | First-trimester combined screening for trisomy 21 was carried out in 75, 821 singleton pregnancies with live foetuses at 11+0 to 13+6 gestational weeks. | Chromosomal abnormalities were identified in 544 pregnancies, including 325 cases of trisomy 21. Increased NT associated to trisomy, trisomy 18, 13 and other chromosomal defects. | 21 |
| Taipale P et al., [22] 1997 | Cohort | Trans vaginal ultrasonography performed in 10,010 women less than 40 years of age with live singleton foetuses at 10 to 15.9 weeks of gestation. Increased foetal nuchal translucency was defined as an area of translucency at least 3 mm. | Abnormal karyotype was seen in abnormal NT in 76 foetuses. | 18 |
| Bijok J et al., [23] 2013 | A retrospective study | Children development in 87 women with increased foetal nuchal translucency and normal karyotype that underwent chorionic villus sampling at our department. Mean observation period was 12 months after birth. | NT was significantly higher in newborns with adverse pregnancy outcome than in after a normal anomaly scan at 20 weeks gestation the risk of adverse outcome was 14.5%. The rate of neurodevelopmental delay was 3.4 % and was not higher than in the general population. | 20 |
| Ayräs O et al., [24] 2013 | Cross-sectional | 1063 singleton pregnancies with increased NT at the first screening ultrasound examination were included. Pregnancy outcomes and short-term outcomes of the newborns were recorded and analyzed. | Structural defects or genetic disorders were observed in 9% of cases, of which 58% resulted in live birth, 34% in termination of pregnancy, and 8% in miscarriage or perinatal death. | 17 |
| Dane B, et al., [25] 2008 | Nested case-series | CRL, NT was recorded. A total of 1930 pregnant women were screened between 11-14 weeks. Follow up information was obtained by a review of medical records and self-reports from patients. | The prevalence of increased foetal NT was 1.4%. Among these, 12 showed increased foetal NT as an isolated finding. In the group with additional abnormalities were found to have chromosomal abnormalities. For all cases with increased foetal NT, total incidence of adverse outcome was 62%. | 18 |
| Lithner CU, et al., [26] 2015 | Cohort | Foetal NT was measured in 55, 123 singleton pregnancies. | Of the 139 high NT pregnancies with normal karyotype, 110 resulted in live births, one IUFD, 23 TOP and five MC. Structural foetal defects were found in 28, of which seven resulted in live births and 21 were terminated. The most common structural defect was cardiac defects. | 16 |
| Brady AF et al., [27] 1998 | Cross-sectional study | Clinical follow up of 89 chromosomally normal live births that in foetal life had a minimum NT thickness of 3.5 mm and a comparison group of 302 infants whose foetal nuchal translucency thickness at 10-14 weeks of gestation was less than 3.5 mm was performed. | Major abnormalities, mainly structural defects of the cardiovascular or skeletal systems. Delay in achievement of developmental milestones was observed in one of the infants with increased translucency and in one of the comparison group. | 19 |
| Souka AP et al., [28] 2001 | Retrospective study | 1320 chromosomally normal singleton pregnancies with nuchal translucency of ≥ 3.5 mm evaluated. In addition to foetal karyotyping these patients were managed with follow up scans at 14 to 16 and 20 to 22 Weeks. | In the 1,320 pregnancies there were 68 spontaneous abortions or intrauterine deaths, 18 neonatal and infant deaths and 154 terminations of pregnancy. In the 1,080 survivors, 60 had abnormalities requiring medical or surgical treatment or leading to mental handicap. | 16 |
| Tahmasebpur A et al., [29] 2012 | Cross-sectional study | A total of 186 cases with NT≥ 95th centile who attended for the first trimester screening were studied. All cases with increased NT including those with normal karyotype were followed up with anomaly scan at 18-22 weeks and foetal echocardiography at 22 to 24 weeks. Pregnancy outcome was extracted from delivery records and paediatrics notes and telephone interviews. | Almost 19.8% were abnormal karyotype, including 29 cases of trisomy 21, three of trisomy 18, two of trisomy 13, three of Turner syndrome. 4.6% of cases were found to have malformation antenatally and 4% cases postnatally. 11.4% women elected termination of pregnancy without further follow up. There were 4.6% foetal loss and 1.3% hydrops foetalis. | 17 |
| Mula R et al., [30] 2012 | Cohort | Singleton foetuses with NT above the 99(th) percentile and normal karyotype scanned. Work-up included first- and second-trimester anomaly scan, first- and second-trimester foetal echocardiography, and in selected cases infection screening and genetic testing. | There were seven spontaneous foetal losses, 38 terminations of pregnancy and two postnatal deaths. Among the 124 survivors, 12 were born with structural abnormalities. Neurodevelopmental follow up was completed in 108 of the 124 survivors and four showed moderate to severe impairment. Overall, a structural abnormality or genetic syndrome was diagnosed in 50 foetuses/newborns. Interestingly, a single umbilical artery was found in six foetuses with no structural defects at birth. | 19 |
| Scholl J et al., [31] 2012 | A retrospective cohort study | First-trimester foetuses with ultrasound-diagnosed nuchal cystic hygroma collected over a 10-year period. | A major congenital anomaly occurred in 28.8%. Perinatal loss occurred in 39% Overall, an abnormal outcome occurred in 86.6% of foetuses. | 19 |
| Muru K et al., [32] 2013 | Cohort | Screening tests of 5,257 pregnant women were analyzed during one-year period. | Among the 74 pregnant women, a structural or genetic abnormality was diagnosed in 16 cases, foetal death occurred in 12 cases and child was healthy at the age of two years in 31 cases. Four children had with congenital anomalies and/or syndromes: two had congenital heart disease – atrial septal defect and ventricular septal defect with patent ductus arteriosus, one Silver-Russell syndrome and one congenital adrenal hyperplasia. | 18 |
Discussion
Results have demonstrated that there is relationship between an increase foetal NT in pregnancy and adverse outcomes. An NT of above 2.5 mm was commonly found among different studies. Analysis of the articles revealed that major cardiac problems were more highly associated with increased NT in foetuses than other abnormalities. Cardiac defects related to the increased NT included heart murmur, systolic organic murmur, ASD, VSD, murmur, tricuspid valve insufficiency and pulmonary valve insufficiency, Intraventricular Communication (IVC) and Patent Ductus Arteriosus (PDA) [11–14]. Allergic symptoms were also common in increased NT such as allergies to antibiotics, food, pollen or animals [13]. Examination of the relationship between increased NT and chromosomal defects revealed that the incidence of chromosomal defects increases with foetal NT thickness. Increased NT was correlated with trisomy 21, trisomy 18, triploidy, monosomy X and trisomy 13. There was a stable and major increase in the mean foetal heart rate in trisomy 21 pregnancies [15–19]. Studies confirmed the association between Klinefelter syndrome and increased NT [20,21]. NTs of 4 mm to 22 mm have been correlated with aneuploidy, Turner’s syndrome, cystic hygroma, hydrops foetalis, and aneuploidy [22]. In 2013, Bijok J et al., found that Intra Uterine Foetal Death (IUFD), structural abnormalities, neonatal death, genetic disorders, and other major anomalies were among the adverse pregnancy results of increased NT [23]. The association between increased NT and a wide range of structural abnormalities and genetic syndromes suggests the increased need for follow-up scans, including foetal echocardiography and genetic testing [24–27]. Researchers believe that actual associations among one or more of several mechanisms, including venous congestion in the head and neck in relation to the contraction of the foetus in amniotic rupture sequence, cardiac dysfunction related to disorders of the heart and great vessels, lymphatic drainage failure due to abnormal development of the lymphatic system and neuromuscular disorders, may exist; vitamin B9 deficiency, anaemia and hypoproteinemia have also been associated with increased NT and should be evaluated in this case [28,29]. A broad series of disorders have been reported in foetuses with increased NT [30–32]. Other defects in increased NT were strawberry capillary naevi, haemangiomas, umbilical hernias, inguinal hernias, hypospadias, testis, mild undescended hydrocele, positional talipes equinovarus, clinodactyly, finger [33]. Echocardiography and foetal anomaly scan can detect many abnormalities from the 12th week of pregnancy. Chorionic villus sampling is used as follow-up scan at 14-16 weeks, evolution and diagnosis NT or delete of many birth defects. The true prevalence of developmental neuronal delay is likely to be underestimated because abnormalities may not appear until several years after birth in many cases. This study offers prenatal research that can help determine adverse pregnancy outcomes.
Limitation
The weaknesses of this review include a lack of access to all related journals and a lack of case-control studies. Given the importance of determining whether a fetus presents congenital abnormalities during pregnancy, further studies in different countries are necessary for determination of NT cut-off. Systematic reviews for evaluating the neurodevelopmental outcome of foetuses with increased nuchal translucency are also recommended.
Conclusion
Systematic reviews of pregnancy outcomes with increased NT provide useful information for physicians and health care practitioners and support decision-making and the selection of interventions to apply during pregnancy. Increased NT is associated with various foetal defects. To verify the presence of malformations, birth defect consultations with a perinatologist and additional tests are required.
Author’s Contribution: Development of the main idea and writing the article: Nasibeh Roozbeh, leili Darvish Revision of the study: Nasibeh Roozbeh, leili Darvish and Maryam Azizi.
Funding/Support: We received no funding from any organization for this research.
[1]. Nicolaides KH, Nuchal translucency and other first-trimester sonographic markers of chromosomal abnormalitiesAm J Obstet Gynecol 2004 191(1):45-67. [Google Scholar]
[2]. Snijders R, Noble P, Sebire N, Souka A, Nicolaides K, UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10–14 weeks of gestationThe Lancet 1998 352(9125):343-46. [Google Scholar]
[3]. Grandjean H, Sarramon MF, Sonographic measurement of nuchal skinfold thickness for detection of Down syndrome in the second-trimester fetus: a multicenter prospective studyJ Obstetet Gynecol 1995 85(1):103-06. [Google Scholar]
[4]. Watson WJ, Miller RC, Menard MK, Chescheir NC, Katz VL, Hansen WF, Ultrasonographic measurement of fetal nuchal skin to screen for chromosomal abnormalitiesAm J Obstet Gynecol 1994 170(2):583 [Google Scholar]
[5]. Michailidis GD, Economides DL, Nuchal translucency measurement and pregnancy outcome in karyotypically normal fetusesUltrasound Obstet Gynecol 2001 17(2):102-05. [Google Scholar]
[6]. Sepulveda W, Wong AE, Casasbuenas A, Solari A, Alcalde JL, Congenital diaphragmatic hernia in a first-trimester ultrasound aneuploidy screening programPrenat Diagn 2008 28(6):531-34. [Google Scholar]
[7]. Sotiriadis A, Papatheodorou S, Makrydimas G, Neurodevelopmental outcome of fetuses with increased nuchal translucency and apparently normal prenatal and/or postnatal assessment: a systematic reviewUltrasound in Obstetrics & Gynecology 2012 39(1):10-09. [Google Scholar]
[8]. Bilardo C, Timmerman E, Pajkrt E, van Maarle M, Increased nuchal translucency in euploid fetuses what should we be telling the parents?Prenat Diagn 2010 30(2):93-102. [Google Scholar]
[9]. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studiesJ Clin Epidemiol 2008 61(4):344-49.PMID: 18313558 [Google Scholar]
[10]. Abdi F, Kazemi F, Ramezani Tehrani F, Roozbeh N, Protocol for systematic review and meta-analysis: hop (Humuluslupulus L.) for menopausal vasomotor symptomsBMJ Open 2016 6(4):e010734 [Google Scholar]
[11]. Ghi T, Huggon IC, Zosmer N, Nicolides KH, Incidence of major structural cardiac defects associated with increased nuchal translucency but normal karyotypeUltrasound Obstet Gynecol 2001 18:610-14. [Google Scholar]
[12]. Zosmer N, Souter VL, han CSYC, Huggon IC, Nicolaides KH, Early diagnosis of major cardiac defects in chromosomally normal fetuses with increased nuchal translucencyBr J Obstetet Gynaecol 1999 06:829-33. [Google Scholar]
[13]. Hiippala A, Eronen M, Taipale P, Salonen R, Hiilesmaa V, Fetal nuchal translucency and normal chromosomes: a long-term follow-up studyUltrasound Obstet Gynecol 2001 18:18-22. [Google Scholar]
[14]. Vieira LA, Silva SV, de Faria RB, Lippi UG, Lopes RG, Perinatal and pediatric follow up of children with increased nuchal translucency and normal karyotypeRev Bras Ginecol Obstet 2013 35(6):274-80. [Google Scholar]
[15]. Matias A, Gomes C, Flack N, Montenegro N, Nicolaides KH, Screening for chromosomal abnormalities at 10–14 weeks: the role of ductusvenosus blood flowUltrasound Obstet Gynecol 1998 12:380-84. [Google Scholar]
[16]. Jauniaux E, Gavrill P, Khun P, Kurdi W, Hyett J, Nicolaides KH, Fetal heart rate and umbilico-placental Doppler flow velocity waveforms in early pregnancies with a chromosomal abnormality and/or an increased nuchal translucency thicknessHuman Repro 1996 11(2):435-39. [Google Scholar]
[17]. Maymon R, Jauniaux E, Cohen O, Dreazen E, Weinraub Z, Herman A, Pregnancy outcome and infant follow-up of fetuses with abnormally increased first trimester nuchal translucencyHuman Reproduction 2000 15(9):2023-27. [Google Scholar]
[18]. Schwarzler P, Carvalho tJS, Senat MV, Masroor T, Campbell Professor S, Screening for fetal aneuploidies and fetal cardiac abnormalities by nuchal translucency thickness measurement at 10-14 weeks of gestation as part of routine antenatal care in an unselected populationBr J Obstetet Gynaecol 1999 106:1029-34. [Google Scholar]
[19]. Westin M, Saltvedt S, Bergman G, Almström H, Grunewald C, Valentin L, Is measurement of nuchal translucency thickness a useful screening tool for heart defects? A study of 16,383 fetusesUltrasound Obstet Gynecol 2006 27:632-39. [Google Scholar]
[20]. Zoppi MA, Ibba RM, Floris M, Monni G, Fetal nuchal translucency screening in 12 495 pregnancies in SardiniaUltrasound Obstet Gynecol 2001 18:649-51. [Google Scholar]
[21]. Nicolides KH, Spencer K, Avgidou K, Faiola S, Falcon O, Multicenter study of first trimester screening for trisomy 21 in 75, 821 pregnancies: results and estimation of the potential impact of individual risk-orientated two-stage first-trimester screeningUltrasound Obstet Gynecol 2005 25:221-26. [Google Scholar]
[22]. Taipale P, Hiilesmaa V, Salonen R, Ylöstalo P, Increased Nuchal Translucency as a Marker for Fetal Chromosomal DefectsN Engl J Med 1997 337:1654-58. [Google Scholar]
[23]. Bijok J, Ziora-Jakutowicz K, Ilnicka A, Pawłowska B, Jóźwiak A, Dangel J, Increased nuchal translucency in chromosomally normal fetuses and pregnancy outcomes-a retrospective studyGinekol Pol 2013 84(3):172-79. [Google Scholar]
[24]. Äyräs O, Tikkanen M, Eronen M, Paavonen J, Stefanovic V, Increased nuchal translucency and pregnancy outcome: a retrospective study of 1063 consecutive singleton pregnancies in a single referral institutionPrenatal Diagnosis 2013 33(9):856-62. [Google Scholar]
[25]. Dane B, Dane C, Cetin A, Kiray M, Sivri D, Yayla M, Pregnancy outcome in fetuses with increased nuchal translucencyJ Perinatol 2008 28:400-04. [Google Scholar]
[26]. Lithner CU, Kublickas M, Sverker Ek, Pregnancy outcome for fetuses with increased nuchal translucency but normal karyotypeJ Med Screen 2016 23(1):01-06. [Google Scholar]
[27]. Brady AF, Pandya PP, Yuksel B, Greenough A, Patton MA, Nicolaides KH, Outcome of normal with chromosomally livebirths increased fetal nuchal translucency at 10-14 weeks’ gestationJ Med Genet 1998 35:222-24. [Google Scholar]
[28]. Souka AP, Krampl E, Bakalis S, Heath V, Nicolides KH, Outcome of pregnancy in chromosomally normal fetuses with increased nuchal translucency in the first trimesterUltrasound Obstet Gynecol 2001 18:9-17. [Google Scholar]
[29]. Tahmasebpour A, BaradaranRafiee N, Ghaffari S, Jamal A, Increased Nuchal Translucency and Pregnancy OutcomeIJPH 2012 41(11):92-7. [Google Scholar]
[30]. Mula R, Goncé A, Bennásar M, Arigita M, Meler E, Nadal A, Increased nuchal translucency and normal karyotype: perinatal and pediatric outcomes at 2 years of ageUltrasound Obstet Gynecol 2012 39(1):34-41. [Google Scholar]
[31]. Scholl J, Durfee SM, Russell MA, Heard AJ, Iyer C, Alammari R, First-Trimester Cystic Hygroma: Relationship of Nuchal Translucency Thickness and OutcomesObstet Gynecol 2012 120(3):551-59. [Google Scholar]
[32]. Muru K, Vals M-A, Sitska M, Asser K, Tammur P, Zilina O, Outcome of Children with Marked Changes in Maternal Screening Tests and Normal KaryotypeGenetics 2013 3:1 [Google Scholar]
[33]. Czuba B, Borowski D, Cnota W, Sieroszewski P, Grettka K, Pietryga M, Ultrasonographic assessment of fetal nuchal translucency (NT) at 11th and 14th week of gestation–Polish multicentre studyNeuro Endocrinol Lett 2007 28(2):175-81. [Google Scholar]