Effect of Trauma to Primary Tooth on Permanent Maxillary Incisors: A Clinical Case Report
Bhawana Gupta1, Sachin Gupta2, Jitesh Wadhwa3, Alpa Gupta4
1 Consultant, Conservative and Operative Dentistry, Private Practice, Gupta dental clinic, Rohtak, Haryana, India.
2 Reader, Department of Periodontics, Career Institute of Dental Sciences, Lucknow, U.P, India.
3 Reader, Department of Orthodontics, K.D Dental College, Mathura, U.P, India.
4 Senior Resident, Conservative and Operative Dentistry, Post Graduate Institute of Dental Sciences, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Alpa Gupta, H. No 640/30 Adarsh Nagar, Rohtak-124001, Haryana, India.
E-mail: alpagupta2008@gmail.com
Trauma to primary tooth leads to abnormal variations in crown and root canals of permanent teeth that presents a challenge in diagnosis and clinical management to the practitioner. This article presents a detailed case report of the endodontic treatment of a three canalled maxillary central incisor and maxillary lateral incisor having single canal with open apex linked with periodontal defect. Root canals were prepared with hand files and canals were irrigated with 2.5% sodium hypochlorite solution. Calcium hydroxide was placed as an intracanal medicament. As the expected healing did not occur even after one month of calcium hydroxide therapy, so periapical endodontic surgery was performed using Platelet Rich Plasma (PRP). Satisfactory clinical and radiographic results were obtained at 12 months. Detailed knowledge of the anatomical variations in the root canal and awareness of their configuration is essential for the success of such cases.
Anatomic variations, Open apex, Platelet rich plasma
Case Report
A 15-year-old boy with a non-contributory medical history was referred to Department of Conservative Dentistry and Endodontics of Post Graduate Institute of Dental Sciences, Rohtak, Haryana by a private practitioner. Patient reported history of trauma at the age of 5 years. He presented with a dilacerated crown in relation to the left maxillary central incisor (21), a sinus tract in the facial vestibule and tenderness to percussion with respect to left maxillary lateral incisor (22) [Table/Fig-1a]. Periodontal probing showed an intact epithelial attachment with 3-mm mesial and distal probing, 2-mm palatal probing and 3 mm buccal probing in 21, but it revealed 9-mm probing depth in relation to buccal aspect of 22. Radiographic evaluation indicated large periapical radiolucency, open apex and a tooth like structure associated with 22 [Table/Fig-1b]. Furthermore, there was evidence of additional canals radiographically in relation to 21. The differential diagnosis of pulpal necrosis with chronic periapical abscess and radicular cyst were considered based on the facts that teeth were nonvital, pus discharge from the sinus and large periapical radiolucency present in relation to both the teeth. The management part included the endodontic root canal treatment of both the teeth.
(a) Figure showing dilacerated crown of maxillary left central incisor and sinus in vestibule in relation to maxillary left lateral incisor; (b) Radiograph showing open apex of maxillary left lateral incisor, tooth like structure associated with large periapical radiolucency.

After local anaesthesia and rubber dam isolation, access openings of both the teeth were performed. At the first appointment 2 canals could be identified under the dental microscope in 21. The working length was determined by an electronic apex locator (Root ZX; Morita, Tokyo, Japan) and radiographically confirmed. The canals were cleaned and shaped with Gates Glidden burs (Dentsply, Maillefer, Ballaigues, Switzerland) and hand K files (Dentsply, Maillefer). While in 22, length was determined radiographically. Irrigation was carried out with copious amounts of 2.5% sodium hypochlorite. Calcium hydroxide (Ultradent, South Jordan, UT) was applied after the biomechanical instrumentation in both the teeth, and the access cavities were sealed with the temporary filling material (Cavit; 3 M, St Paul, MN).
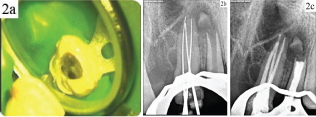
One week later, the sinus tract still persisted. At that time, on careful inspection of the pulp chamber floor, a third canal orifice was detected under high magnification in relation to 21 [Table/Fig-2a]. Subsequently, this canal was also thoroughly cleaned and shaped [Table/Fig-2a] after the working length had been determined [Table/Fig-2b]. Again calcium hydroxide dressing was given in both 21 and 22. After one month of calcium hydroxide therapy, it was decided to perform periapical endodontic surgery because the expected healing did not occur and symptoms did not resolve, still there was pus discharge from both the teeth.
(a) Clinical picture showing three canals in maxillary left central incisor; (b) Radiograph showing working length of three canals in maxillary left central incisor; c) Radiograph showing obturation of maxillary left central and lateral incisor;
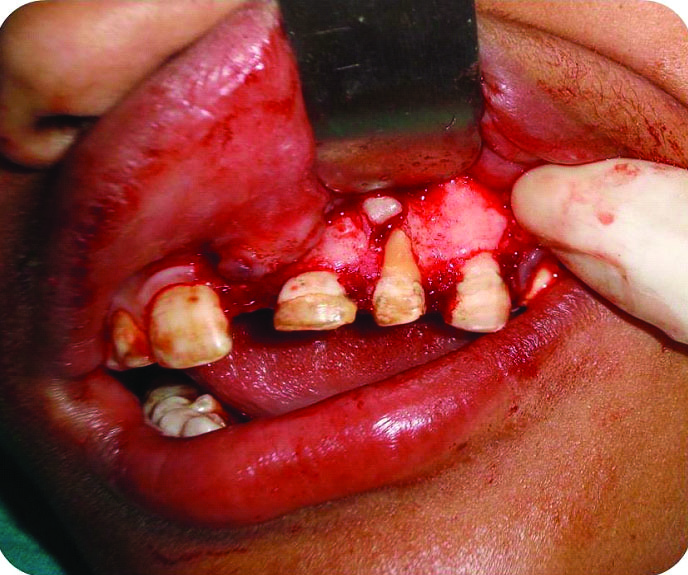
After the initial blood investigations, the surgical procedure was considered. 2.5% sodium hypochlorite was used as an irrigating agent and finally the canals were obturated with gutta-percha using lateral condensation technique [Table/Fig-2c]. The area was anaesthetized and a full thickness mucoperiosteal flap was raised on the buccal side. A complete loss of labial cortical plate along with periapical lesion, indicative of an apicomarginal defect and tooth fragment was evident in relation to 22 [Table/Fig-3]. The debridement of the tissue at the defect site was followed by irrigation with sterile saline solution. After complete debridement and achievement of haemostasis, retrograde fillings were done in the root canal apices with Mineral Tri oxide Aggregate (MTA) Cement. During this period Platelet Rich Plasma (PRP) was prepared by another clinician. PRP preparation was performed by using the procedure described by Okuda K et al., [1]. PRP was thawed at a faster rate, just fifteen minutes prior to its use in surgical procedure. Finally, 0.3 mL of PRP in coagulated form was obtained by mixing it with 0.1 g of sodium alginate in order to get a sticky gel like consistency. Wound closure was obtained with 4-0 silk suture.
Clinical picture showing labial bone loss, a tooth fragment and periapical lesion on flap elevation.
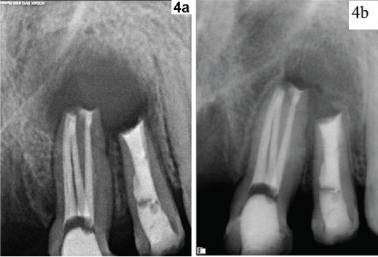
The access cavity were restored with composite resin material (Z250; 3 M), and postoperative radiographs were taken [Table/Fig-4a]. At a 12-month follow-up, both 21 & 22 were asymptomatic. Clinically, the sinus tract had completely resolved, and there was no sign of swelling or oedema. Periodontal probing were 2–3 mm, with no narrow vertical defect evident. A periapical radiograph revealed complete osseous healing of the periradicular radiolucency [Table/Fig-4b].
(a) Immediate postoperative radiograph showing MTA plug formation in both maxillary left central and lateral incisor; (b) Follow up radiograph showing healing of periapical radiolucency after 12 months.
Discussion
Trauma may cause dilacerations of a tooth crown due to the displacement of enamel epithelium and mineralized portion of the tooth in relation to dental papilla and cervical loop [2]. Alterations in the development of permanent teeth caused by trauma to the primary tooth vary from 12 to 69% [2]. The tooth commonly becomes non vital with a periapical lesion as the bent portion with defective enamel and dentin acts as source of entry for microbes [3]. Morphological features of the tooth may adversely affect endodontic procedures. A thorough knowledge of both the external and internal anatomy of teeth is an important aspect of root canal treatment and is essential for the highest possible chance of success [4]. Failure to locate and treat an extra canal/s is one of the most common causes of failures of root canal treatment [5]. A thorough and careful radiographic evaluation and endodontic exploration may lead to identification of additional canals. Radiographs from different angulations helps in locating extra canals. The closeness of two canal orifices to each other also indicates presence of extra canals [5]. It is also imperative to recognize periodontal ligament space that often projects on the tooth and may be similar to a canal [5]. The use of cone beam computed tomography also aids in finding the extra root canals. [6]. In this case, examination of the pulpal floor under an operating microscope and radiographs taken with a file confirmed the existence of the extra canals. Although various cases have been reported having two canals in maxillary central and lateral incisors [6,7], still the cases with three or four root canals are very few [Table/Fig-4c] [8–12]. The present case highlighted the treatment of three canalled maxillary left central incisor and lateral incisor with open apex associated with a tooth like structure. Since the case did not respond to conventional nonsurgical endodontic therapy, so a combined approach with apical surgery was decided to be the treatment plan. Thorough instrumentation of root canal is not achieved usually due to the complexity of the root canal morphology, therefore an intracanal medicament is a requirement so as to disinfect the canals and clear any remaining bacteria. Calcium hydroxide has been considered an ideal material for intracanal dressing as its high alkalinity results in disinfection of the canal system [13].
(c) Table highlighting the studies having three or four root canals in maxillary incisors [8–12].
| Study (year) | Type of tooth | No. of canals |
|---|
| Walvekar SB et al., [8] | Maxillary lateral incisor | three |
| Sheikh-Nezami N et al., [9] | Maxillary central incisor | three |
| Gondim EJr et al., [10] | Maxillary central incisor | three |
| Kattoor K et al., [11] | Maxillary lateral incisor | Four |
| Nosrat A et al., [12] | Maxillary lateral incisor | Four |
The Prognosis of periradicular surgery is significantly decreased when the entire buccal bone plate has been lost (apicomarginal defect). The occurrence of periapical pathosis accompanied by periodontal breakdown constitutes a complex problem in periradicular surgery typically associated with a less favorable prognosis; the predictable and successful management of these cases is a true challenge [14]. In present case also after flap was raised, an apicomarginal defect was revealed in relation to 22. Different recent treatment modalities like guided tissue regeneration, Platelet rich plasma (PRP), platelet rich fibrin have been indicated for the treatment of an apicomarginal defects in anterior teeth [15,16]. In our case, PRP was used for the treatment of the apicomarginal defect. The reason for using PRP was that it is a rich source of growth factors such as Platelet derived growth factor (PDGF), Transforming growth factor (TGF), and - Insulin like growth factor (IGF). PRP works as a haemostatic and stabilizing agent and may aid in blood clot formation because of its high fibrin content. The blood clot aids in regenerative procedures by formation of new periodontal tissue [7,17].
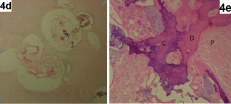
After sending the pathological tissue and tooth like structure from the surgical site for biopsy, we came to conclusion that it was not a radicular cyst case and tooth like entity was confirmed as an odontome [Table/Fig-4d,e]. Since tooth was in developmental stage inflammatory process due to trauma at that time triggered the benign changes in the form of odontome rather than promotion of root apex closure. This odontome could be the contributory factor for appearance of sign and symptoms again and again inspite of giving best endodontic treatment, hence at last surgical procedure was planned to remove the periapical pathology. So, finally a clinical diagnosis of pulpal necrosis with chronic periapical abscess was made. Since with respect to lateral incisor periapical radiolucency along with periodontal communication to the apex was revealed, the final diagnosis of primary endodontic lesion with secondary periodontal involvement was made [18].
(d) Histopathological picture showing ghosts cells, characteristic feature of odontome; (e) Histopathological picture showing abnormal/disorganized mass of normal appearing dentin (D), cementum (C) and pulp tissue (P).
Conclusion
Combined surgical and non surgical approach improves the prognosis of non healing cases in endodontics. In this case satisfactory healing was observed with the use of PRP in the apicomarginal defects but further more studies are required in this direction.
[1]. Okuda K, Tai H, Tanabe K, Suzuki H, Sato T, Kawase T, Platelet rich plasma combined with a porous hydroxyapatite graft for the treatment of intrabony periodontal defects in humans: a comparative controlled clinical studyJ Periodontol 2005 76:890-98. [Google Scholar]
[2]. Andreasen FM, Andreasen JO, Textbook and color atlas of traumatic injuries to teeth 1994 4th edMosby Co:457-494. [Google Scholar]
[3]. Asokan S, Rayen R, Muthu MS, Sivakumar N, Crown dilaceration of maxillary right permanent central incisor- A case reportJ Indian Soc Pedod Prev Dent 2004 22:197-200. [Google Scholar]
[4]. Krasner P, Rankow HJ, Anatomy of the pulp chamber floorJ Endod 2004 30:5-16. [Google Scholar]
[5]. Seltzer S, Bender IB, Smith J, Freedman I, Nazimov H, Endodontic failures: an analysis based on clinical, roentgenographic and histologic findingsOral Surg Oral Med Oral Pathol 1967 23:500-16. [Google Scholar]
[6]. Sharma S, Grover S, Sharma V, Shrivastava D, Mittal M, Endodontic and aesthetic management of a dilacerated maxillary central incisor having two canals using cone beam computed tomography as a diagnostic aidCase rep dent 2014 201:861942 [Google Scholar]
[7]. Sponchiado EC Jr, Ismail HA, Braga MR, de Carvalho FK, Simões CA, Maxillary central incisor with two root canals: a case reportJ Endod 2006 32:1002-04. [Google Scholar]
[8]. Walvekar SV, Behbehani JM, Three root canals and dens formation in a maxillary lateral incisor: a case reportJ Endod 1997 :23185-86. [Google Scholar]
[9]. Sheikh-Nezami M, Mokhber N, Endodntic treatment of a maxillary central incisor with three root canalsJ Oral Sci 2007 :49245-47. [Google Scholar]
[10]. Gondim E Jr, Setzer F, Zingg P, Karabucak B, A maxillry central incisor with three root canals: a case reportJ Endod 2009 35:1445-47. [Google Scholar]
[11]. Kattoor J, Murugesan R, Albuquerque DV, A maxillary lateral incisor with four root canalsInt Endod J 2012 45:393-97. [Google Scholar]
[12]. Nosrat A, Schneider SC, Endodontic management of a maxillary lateral incisor with 4 root canals and a dens Invaginatus tractJ Endod 2015 41:1167-71. [Google Scholar]
[13]. Gomes BP, Ferraz CC, Zaia AA, Teixeira FB, Microbial susceptibility to calcium hydroxide pastes and their vehiclesJ Endod 2002 11:758-61. [Google Scholar]
[14]. Hirsch JM, Ahlström U, Henrikson PA, Heyden G, Peterson LE, Periapical surgeryInt J Oral Surg 1979 8:173-85. [Google Scholar]
[15]. Goyal B, Tewari S, Duhan J, Sehgal PK, Comparative Evaluation of platelet-rich plasma and guided tissue regeneration membrane in the healing of apicomarginal defects: a clinical studyJ Endod 2011 37:773-80. [Google Scholar]
[16]. Dhiman M, Kumar S, Duhan J, Sangwan P, Tewari S, Effect of platelet-rich fibrin on healing of apicomarginal defects: a randomized controlled trialJ Endod 2015 41:985-91. [Google Scholar]
[17]. Marx RE, Carison ER, Eichstaeat RM, Schimmere SR, Strauss JE, Georgeff KR, Platelet-rich plasma: growth factor enhancement for bone graftsOral Surg Oral Med Oral Pathol Oral Radiol & Endod 1998 85:638-46. [Google Scholar]
[18]. Simon JH, Glick DH, Frank AL, The relationship of endodontic- periodontic lesionsJ Periodontol 1972 43:202-08. [Google Scholar]