Introduction
Preserving the integrity of primary dentition is the most important aspect of preventive dentistry. It is advantageous to retain the primary teeth until their normal exfoliation to maintain arch length and harmonized temporal and spatial development of permanent teeth. Early loss of primary teeth can lead to malocclusion, masticatory, speech and aesthetic problems. Dental caries and dental trauma are the most common aetiological factors resulting in pulpal involvement necessitating endodontic treatment [1].
Conventionally, root canal treatment was performed in multiple visits. Intracanal medicaments were used between appointments to reduce or eliminate microorganism from the root canal system. Multiple visit endodontic treatment is well accepted as a safe and common therapy [2].
In current times, completing endodontic procedure in single visit is gaining popularity as it has reduced flare-up rate, no risk of intra appointment leakage through temporary cement, decreased number of operative procedure and dental visits [3,4].
Objective of single visit endodontic treatment is to eradicate the remaining bacteria or render them innocuous by burying them with three-dimensional obturation. Completing the treatment in single visit denies the intracanal microorganisms of nutrition resources required to survive and multiply [5,6].
Views regarding the risks and benefits of single- versus multi visit root canal treatment differ significantly [7,8].
Endodontic treatment performed in either single- or multiple visit can be followed by numerous short- and long term complications. One of the short term complications includes postoperative pain and flare–ups [8]. The development of pain following endodontic treatment is usually due to acute inflammatory response to microbial/physical/ chemical injury to the peri-radicular tissues [9]. It commences within few hours or days after endodontic treatment [9]. Although postoperative pain associated with root canal treatment is a poor indicator of long term success [10]. Postoperative pain and flare-ups may weaken patient’s trust in the clinician and attitude towards endodontic procedure. Postoperative pain and flare-ups may even provoke patient to question clinician’s skills [11].
The ability to predict its prevalence and forewarn the patient may go some way towards enabling coping strategies and help dentist in pain management treatment decisions [12].
Many studies have correlated number of visits needed to complete endodontic treatment, status of pulp vitality, presence of preoperative pain, intracanal medicament, and dental anatomy to postoperative pain following root canal treatment in permanent teeth [13–21].
In primary teeth, there are studies evaluating the success rate of single visit [22], single- vs multiple visit pulpectomy [23], success with different obturating medicaments [24]. However, postoperative pain following endodontic treatment in primary teeth has not been studied widely. Conclusion drawn from studies done in permanent teeth cannot be directly employed to primary molars. Primary teeth have unique anatomy. The roots, particularly those of the molars, are long, slender and the canals narrower and flattened [1]. Moreover, continued deposition of secondary dentin throughout the life of primary teeth causes a change in the morphologic pattern of the root canal, producing variations like lateral branching, connecting fibrils, apical ramification, and partial fusion of the canals [25]. Ancillary canals and ever present resorption of root ends add to the problem of endodontic therapy in primary teeth [1].
The aim of the present study was to compare the incidence and intensity of postoperative pain and flare-ups between single- and multiple-visit pulpectomy in primary molars and to correlate the preoperative status of the pulp to postoperative pain and flare-ups.
Materials and Methods
This was a prospective randomized clinical study using parallel study group. The study was carried out at paediatric dental care center, Mumbai, Maharashtra, India, for a period of 38 months. Ethical clearance was obtained from institutional review board.
Sample Size Calculation
NG Y L et al., reported incidence of postobturation pain, 27.2% in multiple visit and 58.2% in single visit root canal [12]. Hence, sample size calculation was done with an assumption that minimum difference in proportions between the two techniques be 30%, with power of the study set at 80% (beta error at 20%), alpha error at 5%, using the formula,
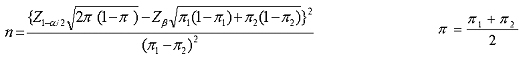
A sample size of N = 38.75 in each group was necessary.
Study Population
Five to eight-year-old cooperative children with one primary molar indicated for pulpectomy (i.e., teeth with irreversible pulpitis and necrosis with minimal root end resorption) [26] were invited to participate in the study. Patients having multiple teeth that required pulpectomy were not included in the study to eliminate the possibility of pain referral. All patients were in good health as determined from medical history. History was taken to ensure that patients had not taken antibiotics or analgesics before the treatment. Teeth with root end resorption more than one third, intraoral or extraoral swellings were not included in the study. Informed written consent was obtained from parents.
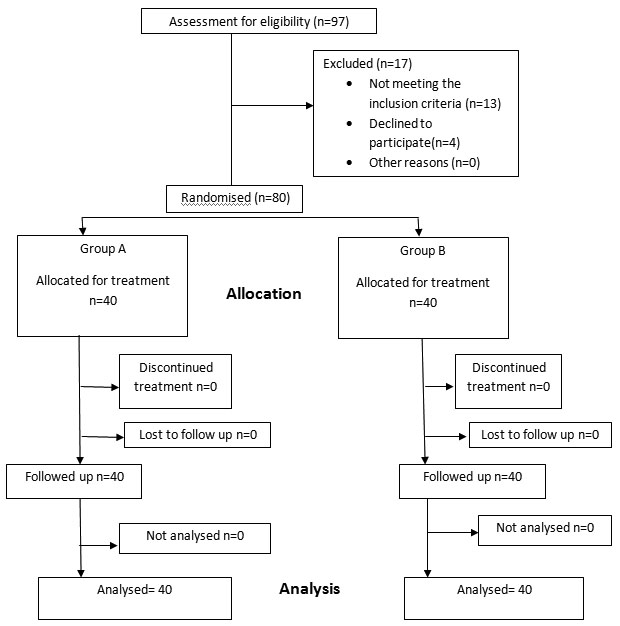
Patients were assigned consecutively to either single visit (Group I) or multiple visit (Group II) treatments (i.e., simple randomization - all odd numbered patients were assigned to single visit and even numbered patients to multiple visit). The decision to use single- or multiple visit treatment was never based on pulp vitality, presence or absence of preoperative pain. This initial disregard for pulp vitality and preoperative pain eliminated the grouping of painful, nonvital teeth into a particular treatment group. After considering the inclusion and the exclusion criteria, 80 patients were included in the study [Table/Fig-1]
Study Design
Tooth location and the vitality of the tooth were recorded. Teeth with no visible haemorrhage on access opening were categorized as nonvital [27]. All the conventional steps in pulpectomy namely access opening, working length determination, chemo mechanical preparation of root canal and obturation were carried out by a single operator. H files (Mani, Inc. Tochigi, Japan) coated with 15% EDTA+10% carbamide peroxide (Prep canal, Ammdent, Mohali, India) were used for mechanical preparation of the root canals. Filing was done 2 mm short of the radiographic root apex to avoid over instrumentation. During instrumentation 3% sodium hypochlorite was used as irrigant. Normal physiologic saline was used as final irrigant in the canals before obturation to flush out any residual sodium hypochlorite. As extrusion of even minimal amount of sodium hypochlorite can result in inflammation and soft tissue destruction [28]. Teeth in Group 1 (single visit pulpectomy) were obturated on the same visit. Teeth in Group 2 (multiple visit pulpectomy) were obturated in the subsequent appointment. Formocresol (Formoa- Cresol, Pharmadent Remedies Pvt Ltd., Vadodara, India) was used as intracanal medicament for teeth in Group II. Metapex (Meta Biomed Co. Ltd., Cheogju city, Korea) was used as obturating material for both the groups. Postobturation radiograph was obtained to make sure that all teeth were satisfactorily obturated.
The patient and parents were familiarized with categorizing the pain before discharging from the dental clinic.
Pain was categorized as none, slight, or moderate/severe as described by Oginni AO and Udoye CI [17] in their study. None: The treated tooth felt normal. Patients didn’t have any pain. Slight pain: Any discomfort no matter how brief in duration that did not require medication and that did not impair masticatory function in any way. Moderate/severe pain: Pain requiring medication (NSAID’s). Impairment of masticatory function (discomfort in chewing). Flare-ups: Pain not controlled with medication (NSAID’s) and or swelling/sinus/pus discharge.
The patients were recalled at three specific postobturation periods, the first, seventh and 30th day. During the first postobturation recall, teeth were restored with stainless steel crowns.
At each postobturation recall visit, the patients were interviewed and examined by one independent evaluator who was blind to visit group under examination. The evaluator determined presence or absence of symptoms at the present visit or during the interval between the present visit and the previous one. The presence or absence of pain, or the suitable degree of pain was recorded at each recall visit.
Intermission between visits and following visit were collectively considered as one postobturation period. The highest degree of pain either in the intermission or at the following visit was noted as the degree of pain for the specific postobturation period.
The compiled data was analyzed using chi-square test. A p-value less than 0.05 was considered as statistically significant.
Results
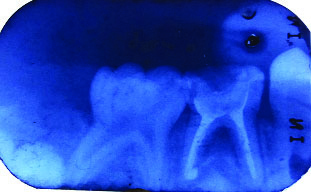
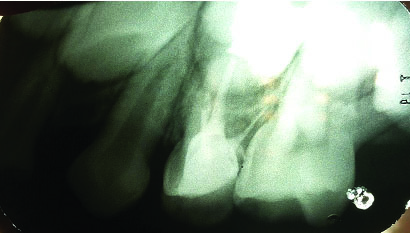
Four cases in both the groups reported postoperative pain (10%) at 24 hours recall, p=0.74 [Table/Fig-2]. One patient reported flare-up (2.5%) in each group, p=0.67 [Table/Fig 3,4 and 5]. These patients reported severe pain which was not controlled with NSAIDs. Clinician had to prescribe antibiotics. However, they did not exhibit any abscess or sinus tract; None of the patients reported pain at seventh day and one month recall.
Comparison of pain on first postobturation day: Single and multiple visit.
| Group | No. of teeth in study | None | Mild | Moderate/Severe | Chi-square value | p-value |
|---|
| No | % | No | % | No | % |
|---|
| Single- visit | 40 | 36 | 90 | 3 | 7.5 | 1 | 2.5 | 1.44 | 0.74 |
| Multiple -visit | 40 | 36 | 90 | 3 | 7.5 | 1 | 2.5 |
| Total | 80 | 72 | 90 | 6 | 7.5 | 2 | 2.5 |
Incidence of postobturation flare-up.
| Group | No. of teeth in study | No. flare-ups | Flare-ups present | Chisquare value | p-value |
|---|
| No | % | No | % |
|---|
| Single-visit | 40 | 39 | 97.5 | 1 | 2.5 | 0.85 | 0.67 |
| Multiple-visit | 40 | 39 | 97.5 | 1 | 2.5 |
Flare up case (nonvital) - Mandibular primary first molar with metapex obturation. Roadiograph showing inter-radicular radiolucency.
Flare up case (vital)-Maxillary primary first molar with metapex obturation.
Postoperative pain was recorded in five non-vital teeth (13.5%) and three vital teeth (6.9%) [Table/Fig-6]. However, it was statistically not significant p=0.53.
Incidence of pain on first postobturation day: vital and nonvital.
| Group | No. of teeth in study | None | Mild | Moderate/Severe | Chi-square value | p-value |
|---|
| No | % | No | % | No | % |
|---|
| Vital | 43 | 40 | 93.02 | 2 | 4.65 | 1 | 2.23 | 0.68 | 0.53 |
| Nonvital | 37 | 32 | 86.48 | 4 | 10.81 | 1 | 2.7 |
Discussion
In the present study, postoperative pain associated with single-visit pulpectomy was the same as postoperative pain associated with multiple visit treatment. The incidence of postoperative pain was 10% for both groups. No statistically significant correlation could be found between pulp vitality and the incidence of postoperative pain.
Immediate postoperative inflammation of periradicular tissues associated with pain is one of the common short term complications of endodontic treatment [8]. Predicting the prevalence of postoperative pain can help dentist in pain management treatment decisions [12].
Pain perception is highly subjective and modulated by multiple physical and psychological factors. The degree of pain/discomfort must be categorized with precise description (e.g., slight pain: any discomfort no matter how brief in duration that did not require medication and that did not impair masticatory function in any way) [8,17]. Hence, in our study, the level of discomfort was rated as slight, moderate, severe pain to simplify pain rating. These three categories were defined clearly before the start of the study and familiarized the patients about categorizing the pain experience.
In our study, postoperative pain associated with single visit pulpectomy was the same as postoperative pain associated with multiple visit treatment. Our results are consistent with those of the majority of the published reports on this topic in permanent teeth [11,16,19,20,29]. Systematic review by Wong AWY et al., [30] also suggested no difference in the incidence of postoperative pain between multi visit and single visit treatment.
However, few studies have expressed other opinion. Yoldas O et al., [18] who studied postoperative pain in retreatment cases, have suggested that two visit treatments with intracanal medicament is effective in reducing postoperative pain and flare–up compared to single-visit in retreatment cases of permanent teeth. Calcium hydroxide mixed with chlorhexidine was used as intra-canal medicament in two visit cases. Subjects of this study were patients who had symptomatic permanent teeth undergoing retreatment. E. faecalis and Candida albicans are common in root canals of teeth undergoing retreatment. Chlorhexidine is effective against E. faecalis [31,32] and Candida albicans [33]. This explains reduced postoperative pain and flare-up in multi visit cases.
Whereas, Su Y et al., (meta-analysis), Roane JB et al., have concluded in their studies that single-visit treatments result in less postoperative pain [4,13]. According to these authors, single visit treatment avoids repeated chemical and physical stimulation to periapical tissues from instrumentation, medicaments and prevents reinfection of the canals as a consequence of leakage past the temporary restoration [4,13].
No postobturation pain persisted to the seventh and 30th day in both groups. Two patients who reported flare–ups had only severe pain which was not controlled by ibuprofen alone and clinician had to prescribe amoxicillin. Pain didn’t persist till seventh postobturation day. No swelling/sinus/pus discharge was noted. Systematic review by Pak JG et al., has also confirmed that the incidence of post-endodontic pain gradually decreases over a period of time [34]. Patients experience highest pain during the first 24-48 hours with a gradual decrease in the following seven days [4]. These evidences suggest that clinicians should not over-respond to initial post-endodontic pain by initiating retreatment immediately.
The pretreatment status of pulp has been suggested to have a considerable influence on the outcome of endodontic treatment. However, our study did not show any statistically significant difference in the pain experience between vital and nonvital teeth. This finding is in disagreement with the conventional idea that single-visit endodontics should be done only in vital teeth. Albashaireh ZS and Alnegrish AS also reported higher incidence of postoperative pain in nonvital teeth [35]. However, results of our study are supported by Roane JB et al., Fava LRG, Eleazer PD et al., Ince B et al., Mulheren JM et al., [13–15,19,21].
Coll JA et al., demonstrated 86.1% success with single visit pulpectomy in nonvital primary molars [22]. Paper point moistened with Buckley’s formocresol was left in the canals for five minutes. Zinc Oxide Eugenol (ZOE) was used as obturating material. Singla R et al., also reported no significant difference in the success rate between single- and multiple visit pulpectomy in primary molar [23]. However, their study did not correlate the preoperative status of the pulp to pulpectomy outcome. Given the combination of effective mechanical instrumentation, the use of antimicrobial irrigating solution and satisfactory obturation, single visit endodontic treatment can effectively take care of the intracanal microbiota and lead to a favourable treatment outcome.
Postoperative pain incidence in permanent teeth ranges from 3%-58% [7]. In our study, the incidence of postoperative pain in primary molars was 10% for both the groups. In permanent teeth, presence of periapical pathology is a risk factor for postoperative pain [12]. Postoperative pain also has a strong correlation with preoperative pain [12,36]. In the current study we excluded the teeth with signs of dentoalveolar abscess and we did not correlate the presence/absence/intensity of preoperative pain with postoperative pain. Probably, these are the reasons for low incidence of postoperative pain.
Pulpectomy when conducted under sound biologic principles by using contemporary scientifically based technique; a low incidence of postoperative pain can be expected.
Further studies need to be carried out to assess the role of different instrument systems, obturating materials, irrigating solutions and patient level of cooperation during treatment on the incidence of postoperative pain in primary teeth. There is also need to identify risk factors for postendodontic pain and flare-up in primary teeth.
Limitation
A possible limitation of any study on pain is the assumption that children’s rating of the pain is a valid estimate of their pain perception. However, there is no way of proving that pain exists other than believing the person in pain.
Another limitation of the current study is inattention to correlate intensity of preoperative pain to postoperative pain. Also, post canal instrumentation pain for multiple visit group was not recorded. Only postobturation pain was taken into consideration.
Conclusion
From the perspective of our study, there was a low incidence of postoperative pain. The majority of patients in both groups reported no pain or only minimal pain at 24 hours recall. There were no differences between single- and multi visit treatment protocols with respect to the incidence of postoperative pain. No significant correlation could be found between pulp vitality and the incidence of postoperative pain.
[1]. Lewis TM, Law DB, Pulpal treatment of primary teeth. In:Finn SB editorsClinical Paedodontics 2003 4th edDelhiAll India traveler bookseller:201-23. [Google Scholar]
[2]. Sathron C, Parasthos P, Messer H, Australian endodontists perception of single and multiple root canal treatmentInt Endod J 2009 2:11-18. [Google Scholar]
[3]. Rossman LE, Hasselgren G, Wolcott JF, Diagnosis and management of orofacial dental pain emergencies. In: Cohen S, Hargreaves KM, editorsPathways of the Pulp 2006 9th edDelhiMosby [Google Scholar]
[4]. Su Y, Wang C, Ye L, Healing rate and postobturation pain of single- versus multiple visit endodontic treatment for infected root canals: A systematic reviewJ Endod 2011 37:125-32. [Google Scholar]
[5]. Oliet S, Single-visit endodontics: A clinical studyJ Endod 1983 9:147-52. [Google Scholar]
[6]. Weiger R, Rosendahl R, Lost C, Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesionsInt Endod J 2000 33:219-26. [Google Scholar]
[7]. Sathorn C, Parashos P, Messer HH, Effectiveness of single-versus multiple-visit endodontic treatment of teeth with apical periodontitis: A systematic review and meta analysisInt Endod J 2005 8:347-55. [Google Scholar]
[8]. Figini L, Lodi G, Gorni F, Gagliani M, Single versus multiple visits for endodontic treatment of permanent teethCochrane Database of Systematic Reviews 2007 4:CD005296 [Google Scholar]
[9]. Sequeria JF, Microbial causes of endodontic flare upInt Endod J 2003 36:453-63. [Google Scholar]
[10]. Taintor JF, Langeland K, Valle GF, Krasny RM, Pain: A poor parameter of evaluation in dentistryOral Surg Oral Med Oral Pathol Oral radiol Endod 1981 52:299-303. [Google Scholar]
[11]. Elmubark AHH, Abu-bakr NH, Ibrahim YE, Postoperative pain in multiple visit and single –visit root canal treatmentJ Endod 2010 36:36-39. [Google Scholar]
[12]. NG Y L, Glenon JP, Setchell DJ, Gulabivala K, Prevalence of and factors affecting postobturation pain in patients undergoing root canal treatmentInt Endod J 2004 37:381-91. [Google Scholar]
[13]. Roane JB, Dryden JA, Grimes EW, Incidence of postoperative pain after single – and multiple – visit endodontic proceduresOral Surg 1983 55:68-72. [Google Scholar]
[14]. Fava LRG, A comparison of one versus two appoint endodontic therapy in teeth with non-vital pulpsInt Endod J 1989 22:179-83. [Google Scholar]
[15]. Eleazer PD, Eleazer KR, Flare -up rate in pulpally necrotic molars in one- visit versus two –visit endodontic treatmentJ Endod 1998 24:614-16. [Google Scholar]
[16]. DiRenzo A, Gresla T, Johnson BR, Rogers M, Tucker D, BeGole EA, Postoperative pain after 1- and 2-visit root canal therapyOral Surg Oral Med Oral Pathol Oral Radiol Endod 2002 93:605-10. [Google Scholar]
[17]. Oginni AO, Udoye CI, Endodontic flare-ups: Comparison of incidence between single and multiple visit procedures in patients attending a Nigerian teaching hospitalBMC Oral Health 2004 4:4 [Google Scholar]
[18]. Yoldas O, Topuz A, Isci AS, Oztunc H, Postoperative pain after endodontic retreatment: Single – versus two- visit treatmentOral Surg Oral Med Oral Pathol Oral Radiol Endod 2004 98:483-87. [Google Scholar]
[19]. Ince B, Ercan E, Dali M, Dulgergil CT, Zorba YO, Colak H, Incidence of postoperative pain after single- and multi-visit endodontic treatment in teeth with vital and non-vital pulpEur J Dent 2009 3:273-79. [Google Scholar]
[20]. Wang C, Xu P, Ren L, Dong G, Ye L, Comparison of postobturatioin pain experience following one visit and two visit root canal treatment on teeth with vital pulps: A randomized controlled trialInt Endod J 2010 43:692-97. [Google Scholar]
[21]. Mulheren JM, Patterson SS, Newton CW, Ringel AM, Incidence of postoperative pain after one-appointment endodontic treatment of asymptomatic pulpal necrosis in single rooted teethJ Endod 1982 8:370-75. [Google Scholar]
[22]. Coll JA, Casper JS, Evaluation of a one-appointment formocresol pulpectomy technique for primary molarsPeadiatr Dent 1985 7:123-29. [Google Scholar]
[23]. Singla R, Marwah N, Dutta S, Single versus multiple visit root canal therapyInt J Clin Peadiatr Dent 2008 1:17-24. [Google Scholar]
[24]. Trairatvorakul C, Chunlasikaiwan S, Success of pulpectomy with zinc oxide-eugenol vs calcium hydroxide/iodoform paste in primary molars: A clinical studyPediatr Dent 2008 30:303-08. [Google Scholar]
[25]. McDonald RE, Avery DR, Dean JA, Treatment of deep caries, vital pulp exposure, and pulpless teeth. In: McDonald RE, Avery DR, Dean JA, editorsDentistry for the child and adolescent 2004 8th edMissouriMosby:388-412. [Google Scholar]
[26]. American Academy on Pediatric Dentistry Clinical Affairs Committee-Pulp Therapy subcommitteeAmerican Academy on Paediatric Dentistry Council on Clinical Affairs. Guideline on pulp therapy for primary and young permanent teethPediatr Dent 2008-2009 30(7 Suppl):170-74. [Google Scholar]
[27]. Berman LH, Hartwell GR, Diagnosis. In: Cohen S, Hargreaves KM, editorsPathways of the Pulp 2006 9th edDelhiMosby [Google Scholar]
[28]. Zhua W, Gyamfi J, Niuc L, Schoeffeld GJ, Liu SY, Santarcangelof F, Anatomy of sodium hypochlorite accidents involving facial ecchymosis – A reviewJ Dent 2013 41:935-48. [Google Scholar]
[29]. Patil AA, Joshi SB, Bhagwat SV, Patil SA, Incidence of postoperative pain after single visit and two visit root canal therapy: A randomized controlled trialJ Clin Diagn Res 2016 10:ZC09-ZC12. [Google Scholar]
[30]. Wong AWY, Zhang C, Chu C, A systematic review of nonsurgical single visit versus multiple -visit endodontic treatmentClin Cosmet Investig Dent 2014 6:45-56. [Google Scholar]
[31]. Steven RH, Grossman LI, Evaluation of antimicrobial potential of calcium hydroxide as an intracanal medicamentJ Endod 1983 9:372-74. [Google Scholar]
[32]. Safavi KE, Spanberg LSW, Langelend K, Root canal dentinal tubule disinfectionJ Endod 1990 16:207-10. [Google Scholar]
[33]. Waltimo T, Orstavik D, Siren E, Haapasalo M, In vitro susceptibility of Candida albicans to 4 disinfecants and their combinationsInt Endod J 1999 32:421-29. [Google Scholar]
[34]. Pak JG, White SN, Pain prevalence and severity before, during, and after root canal treatment: A systematic reviewJ Endod 2011 4:429-38. [Google Scholar]
[35]. Albashaireh ZS, Alnegrish AS, Postobturation pain after single- and multiple visit endodontic therapy. A prospective studyJ Dent 1998 26:227-32. [Google Scholar]
[36]. Risso PA, Cunha AJ, Araujo MC, Luiz RR, Postobturation pain and associated factors in adolescent patients undergoing one and two visit root canal treatmentJ Dent 2008 36:928 [Google Scholar]