The course of the Acute Pancreatitis (AP) ranges from mild form to severe acute form. Most of the episodes are mild and they subside early spontaneously [1,2]. It is associated with increased mortality in patients who develop Severe Acute Pancreatitis (SAP). In such situations we need an indicator which can be trusted upon to predict the outcome of attack whether it is mild or severe.
Pancreatitis which includes 3 criteria only (PANC-3) scoring developed by Brown A et al., of Harvard Medical School as claimed by authors is such a scoring system which is easy to apply, needs facilities of a basic hospital and is as good as other scoring systems in predicting the outcome of an attack of AP. PANC-3 scoring system involves inclusion of three very simple parameters which are: 1) Haematocrit of > 44mg/dl; 2) Body Mass Index of >30 Kg/m2; and 3) Chest X-rays which reveals pleural effusion.
There are several other scoring systems (Ransons, Imrie, CTSI, Acute Physiology and Chronic Health Evaluation (APACHE II, and APACHE III) which have their own statistical importance and prediction of outcome in AP, forecasting patients at risk of SAP [3]. Each one has its pros and cons. Certain scoring systems like Ransons, Imrie have better predictability but one has to wait for 48 hours for full scoring, as a result early therapeutic intervention is missed which may lead to increased mortality. Others can be used to assess the severity at admission and have good predictability but are very cumbersome to use. Also, unnecessarily subjecting the patients to investigations makes it unacceptable universally (APACHE II). The single best marker for predicting severity has yet to be found. CTSI is calculated based on CT findings of some local complications and cannot reflect the systemic inflammatory response.
PANC-3 scoring system is one of the better systems because the three criteria used are simple, easy to assess, available at every health care centre and cost of assessing is low compared to other systems. Using PANC-3 at admission to predict severity is as specific and sensitive as APACHE II, which is the gold standard now [4].
Materials and Methods
This study was conducted in Department of General Surgery, ESIC Medical College, Bengaluru, from March 2015 to February 2016, with the approval from the Institutional Ethics Committee. An 82 patients presenting to the surgical emergency with abdominal pain with raised amylase and lipase levels were included in the study. Chronic pancreatitis and recurrent attack of acute pancreatitis with the previous history of complications like pseudocyst, pancreatic abscess were excluded.
Apart from the routine investigations, investigations to evaluate PANC-3 score – haematocrit, X-ray chest/Ultrasonography for pleural effusion, calculation of body mass index was done.
Investigations to evaluate APACHE II score - ABG with electrolytes, serum creatinine, serum LDH was done. These investigations were done at the time of admission and other investigations were repeated after 48 hours. Above investigations were done on all the patients included in the study, and PANC-3 and APACHE II score was calculated.
Statistical Analysis
Statistical analysis was performed using SPSS 21.0 software. The results of test as patient developed SAP or not were tabulated and the final result were evaluated statistically using Pearsons Chi-Square Test for discrete variables and Mann-Whitney test, Student’s t-test for continuous variables. Results with p-value less than 0.05 were considered statistically significant.
Results
Among 82 patients studied, 59(72%) cases were mild AP and 23(28%) of them presented with SAP based on using the definition from Atlanta Symposium report 2007.
Patients presenting to Emergency Department with diagnosis of AP were stratified according to age [Table/Fig-1]. Majority of patients belonged to age group of 25-35 with 32 of 82 patients (39%).
Age wise distribution of the cases.
| Age (years) | No. of patients | Percentage |
|---|
| 15 – 25 | 13 | 15.8 % |
| 25 – 35 | 32 | 39 % |
| 35 – 45 | 15 | 18.3 % |
| 45 – 55 | 16 | 19.5 % |
| > 55 | 6 | 7.3 % |
The patients with mild AP presented with mean age of 36.03 years when compared to patients with SAP who presented with mean age of 40.39 years. This is against the overall mean of 37.26 years. The range of the patient’s age was between 15-70 years. With a standard deviation of 12.09 years. (p - 0.144).
Among 82 patients 67(81.70%) were male and 15(18.3%) were female, 17 of 23 patients who developed acute severe pancreatitis were male. There was no statistically significant difference was observed when gender was to taken to compare with severity p-value of 0.254.
Regarding the aetiology, 49 cases among 82 were alcoholic as against 21 cases with gall stones, 1 patient was alcoholic and had gall stones. In 13 of the remaining, 1 patient had history of trauma and in others cause was not established.
13 patients (56.5%) among 23 were alcoholic and 5 (21.7%) were of gall stone aetiology. When compared the results with those people who had mild attack there was no significant statistical difference made out in terms of aetiology of an attack. Value of p was 0.709 and 0.616 respectively, for alcohol and gall stone disease in severe acute pancreatitis.
BMI of patients were calculated based on height and weight using formula:
BMI = Wt in Kg/(Height in mts)2
The mean BMI patients presented with was 23.92Kg/m2. The mean BMI in acute pancreatitis was 23.31kg/m2 whereas it was 25.48kg/m2 in acute severe pancreatitis.
Independent samples test was applied to find out the significance of difference in BMI between two groups which showed statistical significance between two group. (p<0.001)
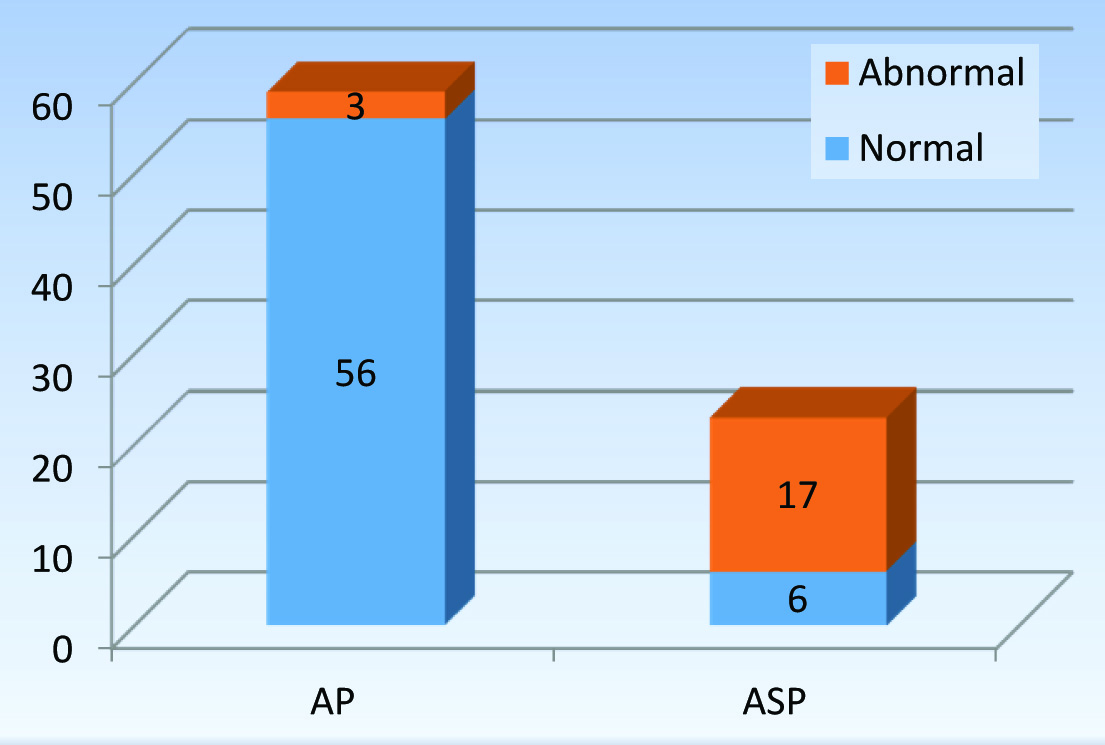
Pleural Effusion
Out of 82 patients who underwent X-ray chest PA view, 27 patients had abnormal X-ray findings. Patients with SAP showed abnormal X-ray findings suggestive of pleural effusion in 18(78.3%)/23. As compared to abnormal findings of 9(15.3%) patients among 59 patients with mild attack (Chi-square test showed p-value of <0.001). Abnormal X-ray findings were more common with ASP group.
Haematocrit
Admission haematocrit of the patient was measured in both AP and ASP cases; with a mean of 43.36 in AP patients and standard deviation of 2.14. There was a statistically significant difference between admission haematocrit of patients with ASP (p<0.001). Patients with an attack of severe pancreatitis had a mean haematocrit value of 46.57 which was over the cut-off>44 [Table/Fig-2].
Mean haematocrit of AP and ASP.
| DIAGNOSIS | N | Mean | Std. Deviation |
|---|
| Hct | AP | 59 | 43.36 | 2.14 |
| ASP | 23 | 46.57 | 2.273 |
PANC-3 Score
Above three criteria were used in calculating PANC-3 score. With 19(82.6%) patients of ASP showing abnormality in PANC-3 score. A total of 6(26.1%) patients had all the three parameters positive with a score of 3, 12(52.2%) had a score of 2 and 1(4.3%) among them had a score of 1.
Cross tabs created taking nil and abnormal PANC-3 score showed statistical significance when compared with PANC-3 score of mild acute pancreatitis (p<0.001) [Table/Fig-3].
Graphical representation of elevated PANC-3 score in patients with AP.
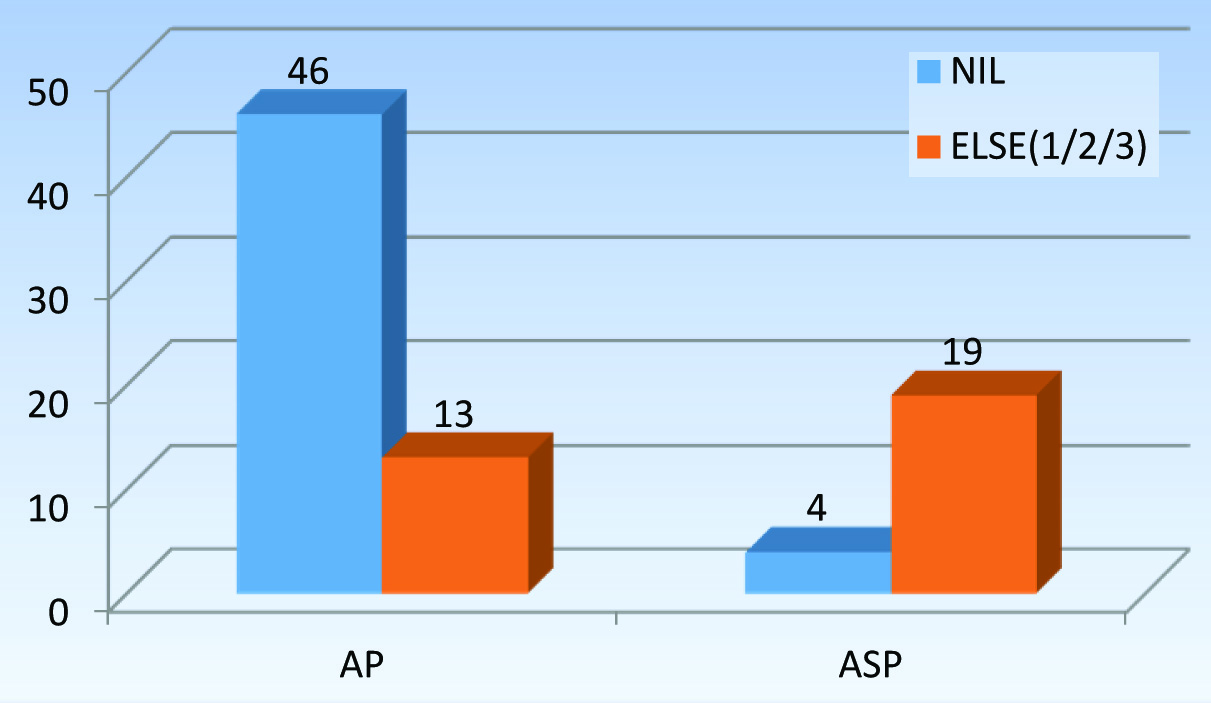
PANC-3 Score
PANC-3 score had a sensitivity of 82.6% and specificity of 77.9%, the test had a Positive Predictive Value (PPV) of 0.59 and Negative Predictive Value (NPV) of 0.92.
APACHE II
APACHE II Score was calculated based on the clinical and laboratory parameters estimated on admission and the results were tabulated as either score of >7 or < 7. Sensitivity of APCHE II in predicting SAP was 91.3% and specificity was 96.6% with PPV of 0.91, NPV was 0.96.
Two (3.4%) of 59 patients of mild pancreatitis had abnormal APACHE II when compared to 21(91.3%) of 23 patients with ASP [Table/Fig-4].
Graphical representation of elevated APACHE II score in patients with acute pancreatitis.
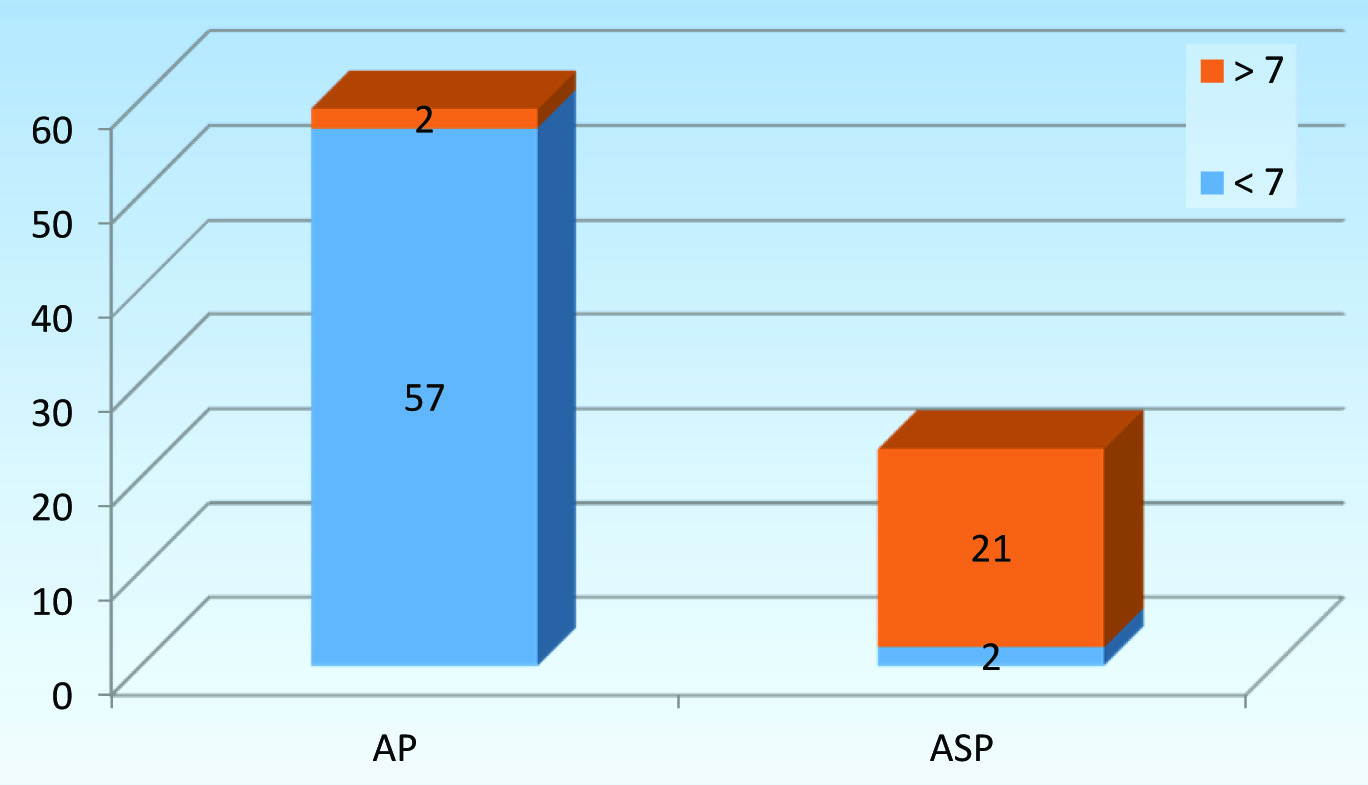
Above graph represents the patients presenting with APACHE II score of >7 and <7. The difference in scores in both the group of mild pancreatitis and severe pancreatitis was statistically significant p < 0.001.
Arterial Blood Gas interpretation
All 82 people were tested for ABG analysis and also as a part of APACHE II score. ABG report alone showed, a statistically significant difference between patients with ASP and mild acute pancreatitis. A total of 17(73.9%) of 23 patients with ASP had an abnormal ABG report. Fifteen (88.2%)/17 of them had metabolic acidosis [Table/Fig-5].
Figure representing abnormal and normal findings of ABG analysis in patients with acute pancreatitis.
Serum Amylase levels
Level of serum amylase was estimated in all the patients who came with history of pain abdomen with suspicion of acute pancreatitis. Mean S. Amylase level was 556.2IU/l which is more than 3 times normal. There was no statistical significance noted p=0.025.
Follow up
Ten patients among 82 admitted for acute pancreatitis did not turn up for follow up.
Four of 23 patients of SAP died due to multiple organ failure, one of them underwent surgery for necrosectomy and patient was in ICU for 20 days. Two were transferred to other ward, one got discharged directly from ICU and other patient was transferred to respiratory medicine.
Thirteen (56.52%) patients with ASP recovered from the disease. While 53(89.83%)/59 of mild attack patients had a normal follow up [Table/Fig-6].
| Follow up | Attrition (LAMA, didn’t follow up etc | Died | Normal | Total |
|---|
| Acute pancreatitis | 6(10.16%) | 0 | 53(89.83%) | 59(100%) |
| Severe Acute pancreatitis | 6(17.4%) | 4(17.4%) | 13(56.52%) | 23(100%) |
Comparison of PANC-3 vs APACHE II scores in predicting acute severe pancreatitis.
Every patient of AP underwent evaluation of PANC-3 score and APACHE II score. And the results were cross-tabulated and statistical tests were applied to the data using SPSS software. The results were analysed separately for both mild attack and severe attack.
Above [Table/Fig–7] shows the comparison of abnormal APACHE II score with abnormal PANC-3 score in patients with mild attack. Thirteen (22%) of patients showed abnormal PANC-3 score, but abnormal APACHE II was present in only 2(3.4%) of cases. When statistical tests were applied there was no significant results obtained. p – 0.007.
PANC-3 vs APACHE II Cross tabulation for Mild Acute Pancreatitis.
| APACHE II |
|---|
| <7 | >7 | Total |
|---|
| PANC-3 | NIL | 46 | 0 | 46 |
| SCORE 1/2/3 | 11 | 2 | 13 |
| TOTAL | | 57 | 2 | 59 |
Comparison of APACHE II and PANC-3 scores in severe acute pancreatitis showed, abnormal findings of PANC-3 was present in 19(82.6%) of 23 patients when compared to 21(91.3%) patients with APACHE II score of >7. Four (17.4%) of 23 acute severe pancreatitis patients had normal PANC-3 compared to 2(8,7%) of abnormal APACHE. Two (8.7%) patients with Acute severe pancreatitis showed normal APACHE II [Table/Fig-8].
PANC-3 * APACHE II Cross tabulation for Acute Severe Pancreatitis.
| APACHE II |
|---|
| <7 | >7 | Total |
|---|
| PANC-3 | NIL | 2 | 2 | 4 |
| SCORE 1/2/3 | 0 | 19 | 19 |
| TOTAL | 2 | 21 | 23 | |
Discussion
Predicting severity of an attack of pancreatitis is an essential step in the management of AP. A 15–20% of patients present with severe disease [3,5] and early recognition of such patients and management in specialized unit helps to avoid the morbidity and mortality associated with the attack. A 50% mortality associated with SAP can be reduced to 8% by early recognition of a case [6].
Various markers have been evaluated to predict the outcome of AP which are markers of severity, early prediction, pancreatic necrosis and infective pancreatic necrosis and mortality [7]. Multi-factorial scoring system using Ranson, Imrie(Glasgow), APACHE II and clinical data like age, aetiology and obesity, Blood urea nitrogen, LDH and evidence of pancreatic necrosis, age, chronic health status, inflammatory markers all were used to predict severity of pancreas.
A total of 82 patients were evaluated in the study over a period of one year. A 72% of patients were of mild attack and 28% of patients had an attack of severe pancreatitis which is comparable with literature all over the world where the incidence is around 20% [3]. Several studies found no difference in the age distribution though there is a general consensus that acute pancreatitis presents late in life. The mean age of presentation in this study was in 4th decade of life when compared to 6th decade of world literature [8]. Patients with severe attack tend to be older than patients with mild attack. The difference was not statistically significant.
Majority (81.7%) of patients were male and there was no statistically significant difference between distributions of disease in terms of gender. It’s been studied that gall stone pancreatitis tend to occur more common in female subjects 1:3 when compared to male and alcohol is more common for pancreatitis in male 6:1 [9,10].
Gall stone pancreatitis was noted in around 20 patients (25.6%) and around 49(59.8%) patients were alcoholic.
Obesity has long been proven to be of a risk factor in many diseases. Even in pancreatitis the severity of an attack is influenced by the Body Mass of a patient [11]. The mean BMI of patients studied were 23.92Kg/m2. In the group with acute severe pancreatitis the mean BMI was 25.48Kg/m2. Western data suggests BMI of ≥25Kg/m2 as overweight and with BMI of >30Kg/m2 being risk factor for developing acute pancreatitis [12]. As the average Indian person body mass index is low compared to western population. Patients who are overweight tend to develop more severe attack. (p<0.001).
An 18(78.3%)/23 of patients had abnormal X-ray findings which is significant in detecting a severe attack. 84.2% of patients had abnormal chest radiograph in a study conducted by Heller et al., [13]. Development of pleural effusion is a sign of SIRS and detection of same radiologically is a good predictor of severity.
AP progresses in severity scale based on the immune response a patient mounts. More severe the immune response more severe the attack for the patient. Fluid sequestration into extravascular space due to leaky capillary channels leads to significant fluid depletion and haemoconcentration. There tends to be increase in haematocrit value in such patients. Haematocrit>44 % and failure to fall in this measure after 24 hours has been shown to be related to the development of pancreatic necrosis and predict organ failure [14]. The mean haematocrit for a patient with severe attack was 46.57% which is significantly more than the mean of 43.3% in the patients with mild attack. Rise in haematocrit not only is a marker of severity but actually can be used as a predictor for severity.
APACHE II score is a very good predictor of severity. It’s been shown that 24 hrs APACHE II score is superior to APACHE II at admission [15]. World literature shows a sensitivity of 65%, specificity of 76% and positive predictive value of 43% and a negative predictive value of 89% when the score was taken as > 7 [15]. Our study showed the sensitivity of APACHE II on admission in predicting acute severe pancreatitis to be 91.3% with specificity of 96.6%, it had a positive predictive value of 91% and negative predictive value of 96%. The results were better than previous studies.
Using combination of the three criteria namely, haematocrit of ≥ 44%, pleural effusion and BMI >25Kg/m2 instead of > 30Kg/m2. The sensitivity of the score in predicting severe acute pancreatitis was 82.6% and specificity of 77.9%, with positive predictive value of 59% and a negative predictive value of 92%. There was no statistically significant difference in predictive value of APACHE II and PANC-3.
Limitation
Only 82 patients were considered for the study, the study requires large number of patients and also needs to be conducted in many institutions so as to prove efficacy of PANC-3 scoring system.
Conclusion
Assessment of severity of pancreatitis helps in better outcome of the patient in terms of morbidity and mortality, as we can give early and advanced care to those in need (i.e., cases of acute severe pancreatitis). Our study shows that PANC-3 can be used to predict the severity of pancreatitis as efficiently as APACHE II. It uses only 3 criteria which are easily done, and available in even the basic health care setup. The interpretation of PANC-3 does not need expertise and can be applied at the time of admission which is an advantage when compared to classical scoring systems.
The ultimate goal of any scoring system or markers is to predict the patients with severe attack early in the course of disease and be able to interrupt the disease as early as possible. PANC-3 scoring system is such an effort to prolong the life of patients by early detection and prompt treatment.