Undifferentiated Uterine Sarcoma: An Uncommon Case Report
Madhumita Mukhopadhyay1, Chhanda Das2, Tamanna Parvin3, Keya Basu4
1 Professor, Department of Pathology, IPGME&R, Kolkata, West Bengal, India.
2 Assistant Professor, Department of Pathology, IPGME&R, Kolkata, West Bengal, India.
3 Postgraduate Student, Department of Pathology, IPGME&R, Kolkata, West Bengal, India.
4 Associate Professor, Department of Pathology, IPGME&R, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chhanda Das, 31, Eastern Park Santoshpur, Kolkata-700075, West Bengal, India.
E-mail: chhhdas@gmail.com
Endometrial Stromal Sarcomas (ESS) are rare uterine malignancy of mesodermal origin. A 65-year-old female presented with postmenopausal bleeding in the Department of Gynaecology in our hospital. Computed Topography (CT) revealed an enlarged uterus with areas of low attenuation. On gross appearance endometrial cavity was distorted with an irregular friable necrotic mass. Histopathologically, it was diagnosed as undifferentiated uterine sarcoma. Rhabdoid, osteoid and cartilaginous differentiation were found along with osteoclast like giant cells. Immunohistochemistry was strongly positive for CD10.
CD10, Postmenopausal bleeding, Uterine malignancy
Case Report
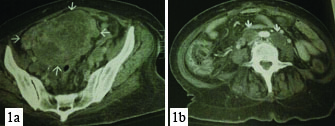
Here we are describing a case of undifferentiated uterine sarcoma in a 65-year-old female who presented with post menopausal bleeding for last six months. In Computed Tomography scan (CT) there was an enlarged uterus with areas of low attenuation with enlarged para-aortic lymph node [Table/Fig-1a,b]. From CT scan view provisionally it was diagnosed as endometrial carcinoma. Total abdominal hysterectomy and salpingophorectomy was done.
a) Picture showing endometrial growth; b) Picture showing enlarged para aortic lymphnode.
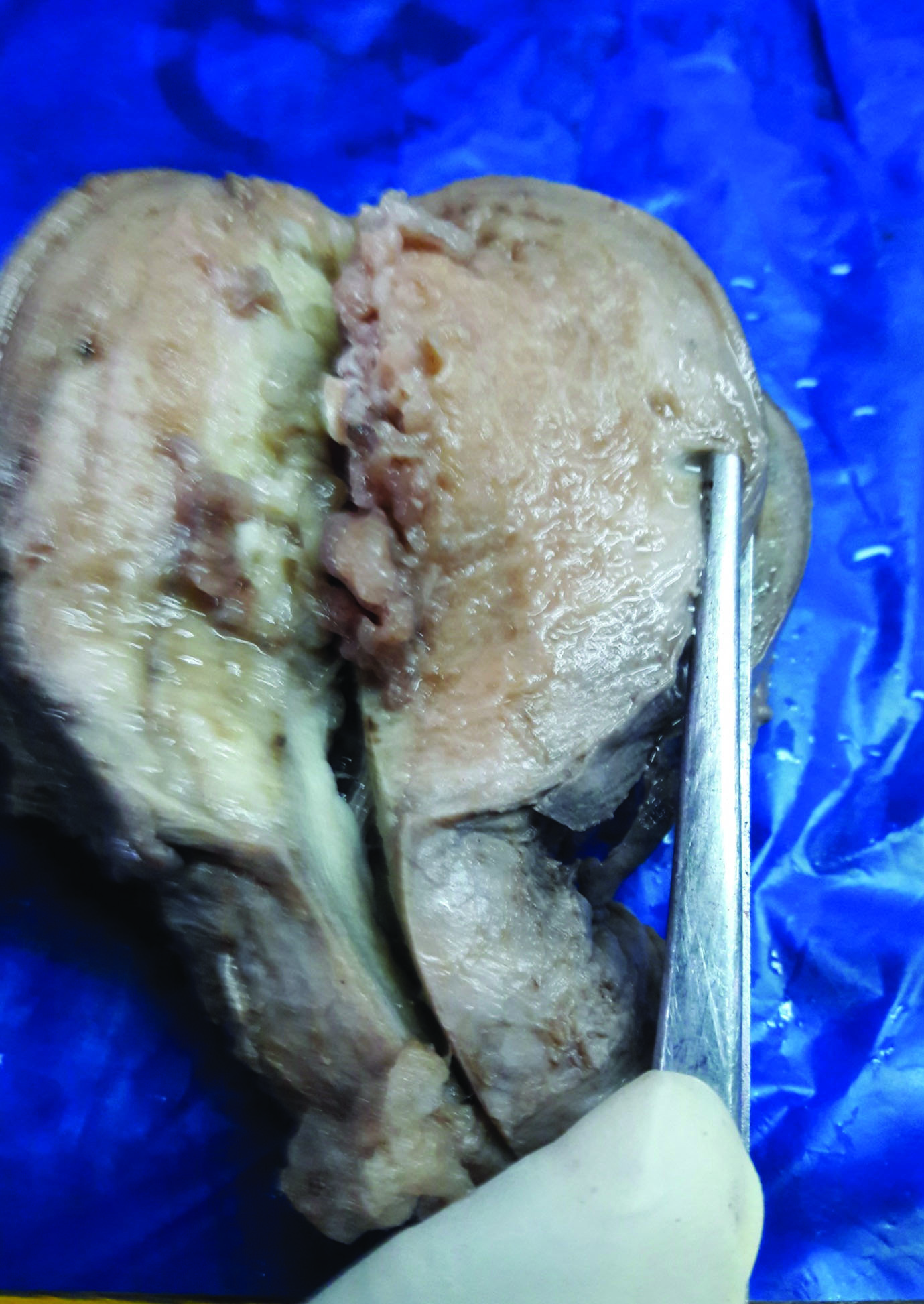
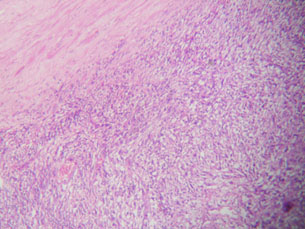
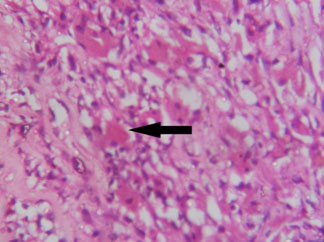
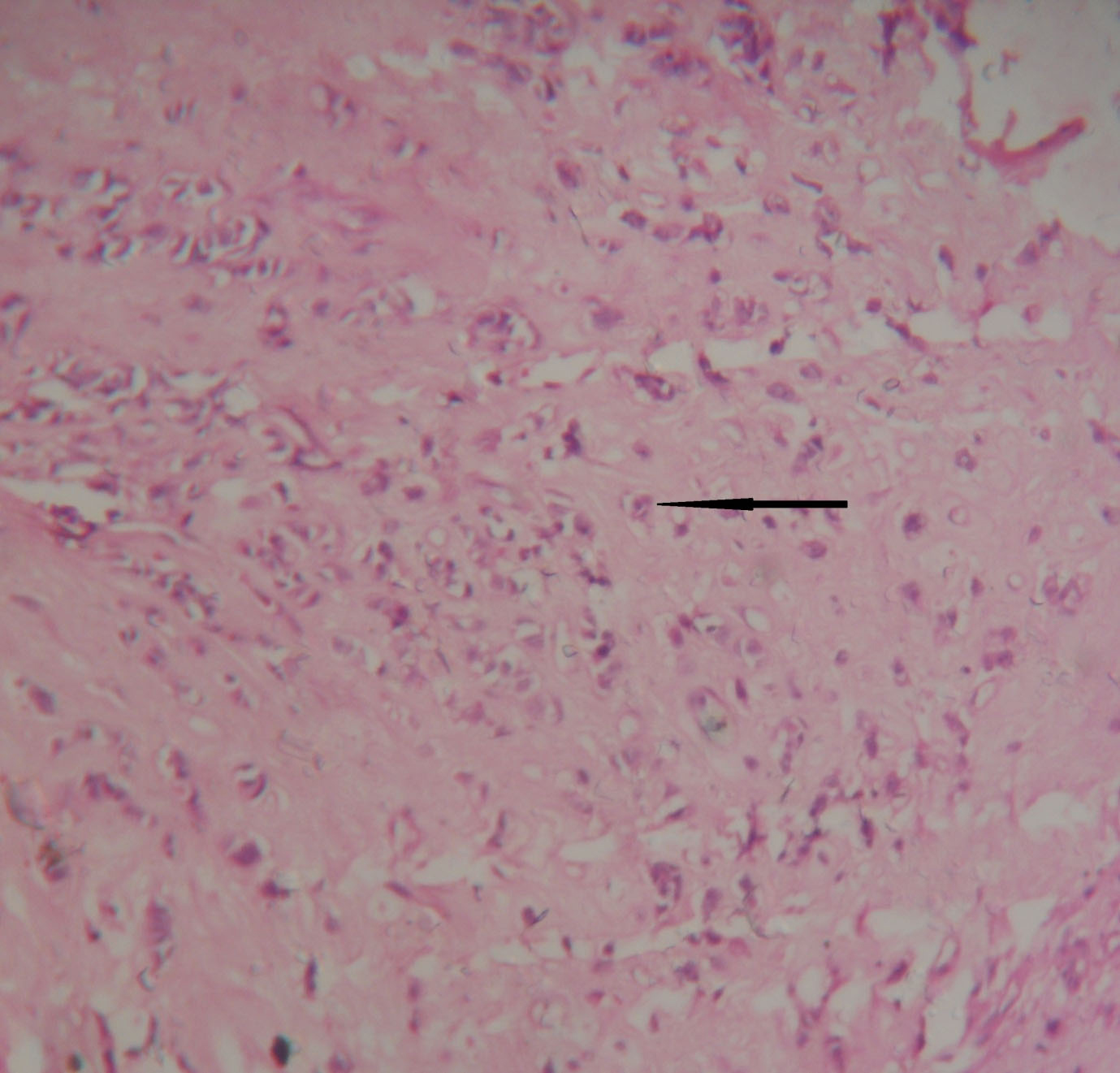
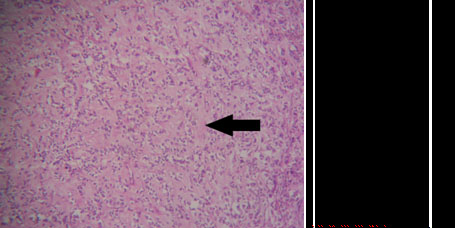
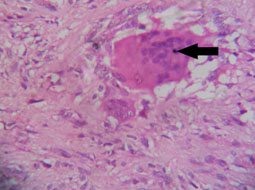
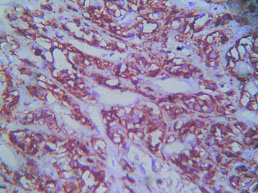
On gross examination of uterus and cervix measured 15 cm x 5 cm x 2 cm, there was irregular friable necrotic mass distorting endometrial cavity [Table/Fig-2]. On histopathological examination, tumour mass was composed of spindle cells arranged in sheets and focally in storiform pattern [Table/Fig-3]. Individual cells showed marked cytological atypia with brisk mitotic activity (>10/10hpf). Features of rhabdoid, cartilaginous and osteoid differentiation were evident associated with osteoclast like giant cells [Table/Fig-4,5,6 and 7]. Lymphovascular and myometrial invasion were noted. Immunohistochemical analysis of tumour revealed strong positivity for CD10 [Table/Fig-8]. It was reported as undifferentiated uterine sarcoma. The patient is still under follow up and is surviving nine months after treatment.
Irregular friable necrotic mass distorting endometrial cavity.
Tumour mass composed of spindle cells arranged in sheets and focally in storiform pattern (H&E, x100);
Tumour mass showing rhabdoid differentiation (H&E, x400).
Tumour mass showing cartilaginous differentiation (x100) (H&E).
Tumour mass showing differentiation (x100) H&E;
Tumour mass showing osteoclastic giant cells (H&E, x400);
Tumour mass showing positive immunostain for CD10 (x400).
Discussion
Endometrial Stromal Tumours (ESTs) of the uterus are the second most common mesenchymal tumours of the uterus [1]. The World Health Organization defined undifferentiated uterine sarcoma as a tumour arising in the endometrium or myometrium, lacking any resemblance to proliferative-phase endometrial stroma, with high-grade cytological features and with no specific type of differentiation. The mean age for diagnosis is 60 years [2]. It has an aggressive clinical course with death occurring usually within three to five years [3]. Approximately two-thirds of patients present with high-stage disease (stage III/IV). They typically have postmenopausal bleeding or signs/symptoms secondary to extrauterine spread [4]. In addition to high-grade cytologic features, ESS can also display variant histologic appearances, including smooth muscle, sex cord, glandular, and fibrous differentiation [5]. In present case, there were features of rhabdoid, osteoid and cartilaginous differentiation with osteoclastic giant cells. These giant cells are stromal in origin and represent a reactive host response.
Based on nuclear pleomorphism Kurihara S et al., recommended a new terminology and classification of undifferentiated uterine sarcomas (non low-grade endometrial stromal sarcomas) [6]. These sarcomas are divided in two groups: Undifferentiated Endometrial Sarcoma with nuclear Uniformity (UES-U) and Undifferentiated Endometrial Sarcoma with nuclear Pleomorphism (UES-P). This case belongs to UES-P.
CD10, a surface neutral endopeptidase is the most sensitive marker for endometrial differentiation and mostly endometrial stromal sarcomas are positive for this marker [7]. The histological differential diagnosis includes endometrial carcinosarcoma with osteoclast-like giant cells, undifferentiated metastatic carcinoma, primary uterine carcinomas, epithelioid leiomyosarcoma or metastatic gastrointestinal stromal tumours and mixed mullerian tumours. Endometrial carcinosarcoma shows positivity for epithelial membrane antigen and pancytokeratin [8]. Epithelioid leiomyosarcoma are positive for myogenic markers [9,10]. Mixed mullerian tumours resemble endometrial stroma tumours with positivity for CD10, WT-1, and pancytokeratin and it also shows variable expression of oestrogen, progesterone, androgen receptors and myogenic markers [11].
Undifferentiated endometrial sarcomas have very poor prognosis and most patients die of disease within two years of the diagnosis. Local recurrences and distant metastases are associated with a high mortality [12]. Treatment is primarily surgical with or without addition of adjuvant radiotherapy or chemotherapy. We are still following our case, surviving nine months after treatment.
Conclusion
Undifferentiated endometrial carcinoma appears to have an aggressive clinical course with advanced stage at presentation. Despite of surgical resection many patients rapidly develop distant metastasis. Adjuvant therapy does not improve patient survival.
[1]. Moinfar F, Kremser ML, Man YG, Zatloukal K, Tavassoli FA, Denk H, Allelic imbalances in endometrial stromal neoplasms: Frequent genetic alterations in the nontumourous normal appearing endometrial and myometrial tissuesGynecol Oncol 2004 95:662-71. [Google Scholar]
[2]. Robert J, Kurman, Maria Luisa Carcangiu, Simon Herrington, Robert H. Young, (Eds.)WHO Classification of Tumours of Female Reproductive Organs 2014 4th editionLyonIARC [Google Scholar]
[3]. Abeler VM, Royne O, Thoresen S, Danielsen HE, Nesland JM, Kristensen GB, Uterine sarcomas in Norway. A histopathological and prognostic survey of a total population from 1970 to 2000 including 419 patientsHistopathology 2009 54:355-64. [Google Scholar]
[4]. Anner EJ, Garg K, Leitao MM Jr, Soslow RA, Hensley ML, High grade undifferentiated uterine sarcoma: surgery, treatment, and survival outcomesGynecol Oncol 2012 127:27-31. [Google Scholar]
[5]. Oliva E, Clement PB, Young RH, Endometrial stromal tumours: An update on a group of tumours with a protean phenotypeAdv Anat Pathol 2000 7:257-81. [Google Scholar]
[6]. Kurihara S, Oda Y, Ohishi Y. Y, Iwasa A, Takahira T, Kaneki E, Endometrial stromal sarcomas and related high- grade sarcomas: Immunohistochemical and molecular genetic study of 31 casesAmerican Journal of Surgical Pathology 2008 32(8):1228-38. [Google Scholar]
[7]. D’Angelo E, Prat J, Uterine sarcomas: A reviewGynecol Oncol 2010 116:131-39. [Google Scholar]
[8]. Amant F, Vandenput I, Van Gorp T, Vergote I, Moerman PH, Endometrial carcinosarcoma with osteoclast-like giant cellsEuropean Journal of Gynaecological Oncology 2006 27(1):92-94. [Google Scholar]
[9]. Irving JA, Lerwill MF, Young RH, Gastrointestinal stromal tumours metastatic to the ovary: A report of five casesAmerican Journal of Surgical Pathology 2005 29(7):920-26. [Google Scholar]
[10]. Leung KM, Wong S, Chow TC, Lee KC, A malignant gastrointestinal stromal tumour with osteoclast-like giant cellsArchives of Pathology and Laboratory Medicine 2002 126(8):972-74. [Google Scholar]
[11]. Soslow RA, Ali A, Oliva E, Mullerian adenosarcomas: an immunophenotypic analysis of 35 casesAmerican Journal of Surgical Pathology 2008 32(7):1013-21. [Google Scholar]
[12]. D’Angelo E, Prat J, Uterine sarcomas: A reviewGynecol Oncol 2010 116(1):131-39. [Google Scholar]