The HC is directed anterolaterally and present above the OC at its junction of anterior one third and posterior two third. It transmits the hypoglossal nerve (which supplies the muscles of the tongue), meningeal branch of ascending pharyngeal artery and emissary vein (which connect the basilar plexus of veins to the internal jugular vein) [1,2]. The venous plexus is considered to be of great significance because it is the major source of venous drainage through the postsellar cranial cavity [3].
Lesions involving the HC are rare and usually benign. They include hypoglossal nerve schwannomas, posterior cranial fossa meningiomas and jugulo-tympanic paragangliomas. The decision to intervene surgically for these lesions is not only based on the tumour size and type but also on the anatomical variations of the HC [4]. Secondly, the extra and intradural tumours are frequently seen in the cranial base near foramen magnum and it poses a challenge to surgeons due to its deeper location. In the modern era with advancement of technology, Transcondylar Approach (TCA) has gained popularity which enables shorter and more direct route to the anterior part of pontomedullary junction with minimal brainstem retraction. The key point of this surgery includes drilling of the posterior part of OC which threatens opening of the HC [5]. Hence the neurosurgeons should be aware of morphological variations of the HC and its relationship to the OC. While going through the literature, we found scanty information regarding osteotic variations in the HC and its relationship with OC in North Indian population. Hence, the aim of the present study was to analyze the morphological and morphometric features of HC and its topographical relationship with OC.
Materials and Methods
The osteologic study was done on 50 adult dry human skulls (100 HC), obtained from the bone bank of the Department of Anatomy, Hamdard Institute of Medical Sciences and Research and Maulana Azad Medical College, New Delhi. Skulls with good condition i.e., intact HC and OC were selected and studied over a period of six months from January to June 2016.
Morphologic study
The morphological variability of HC in relation to the presence of spur, incomplete and complete septa was examined. We classified HC on the basis of these morphological variations into different types based on the classification suggested by Singh V et al., [4] and Paraskevas GK et al., 6].Our proposed classification is shown in [Table/Fig-1].
Classification of morphological variations in the HC into different types.
| Type | Characteristics | Abbreviation |
|---|
| Type 1 | No evidence of bony spur or septum | Type 1 HC |
| Type 2 | Spur in HC | A | Spur present near external opening of HC | Type 2a HC |
| B | Spur present near internal opening of HC | Type 2b HC |
| C | Spur present in the middle part of HC | Type 2c HC |
| Type 3 | Incomplete septa dividing a portion of HC into two parts | A | Septa present near external opening dividing it into double external opening | Type 3a HC |
| B | Septa present near internal opening dividing itinto double internal opening | Type 3b HC |
| C | Septa present in the middle part dividing a portion of HC into two | Type 3c HC |
| Type 4 | Complete septa dividing whole HC into two parts | Type 4 HC |
Morphometric study
Morphometric measurements were taken with the help of sliding Vernier caliper accurate to 0.01 mm. The inclination of the HC with the midsagittal plane was recorded with the help of goniometer. The following morphometric measurements were taken:
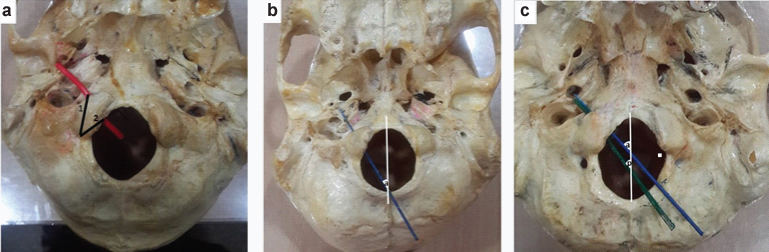
Distance of the extracranial opening of HC from the posterior end of the OC [Table/Fig-2a];
Distance of the intracranial opening of HC from the posterior end of the OC (If two openings were present, then posterior opening i.e., closer to posterior end of OC was considered) [Table/Fig-2a];
Anterior angle of the HC: Angle of inclination of HC to the midsagittal plane in case of Type I HC (no spur/septa) [Table/Fig-2b]; Anterior opening in case of Type 3b HC [Table/Fig-2c];
Posterior angle- Angle of inclination of HC with midsagittal plane through posterior opening in case of Type 3b HC [Table/Fig-2c].
Showing distance of posterior end of OC to the external and internal openings of HC and angle of inclination of HC with the midsagittal plane; a) 1. distance of posterior end of OC to the external opening of HC, 2. distance of posterior end of OC to the internal opening of HC; b) 1. angle of inclination of HC to the midsagittal plane [blue probe in the HC]; c) a- anterior angle of inclination of HC to the midsagittal plane, p- posterior angle of inclination of HC to the midsagittal plane [blue probe in the anterior opening of HC and green probe in the posterior opening of HC in case of double internal opening].
Statistical Analysis
The statistical analysis was done using SPSS software. Descriptive statistics like range, mean, standard deviation were evaluated for all the parameters collected from the skulls. For all the analysis, p<0.05 was accepted as statistically significant, p<0.01 was accepted as highly significant.
Results
Morphologic study
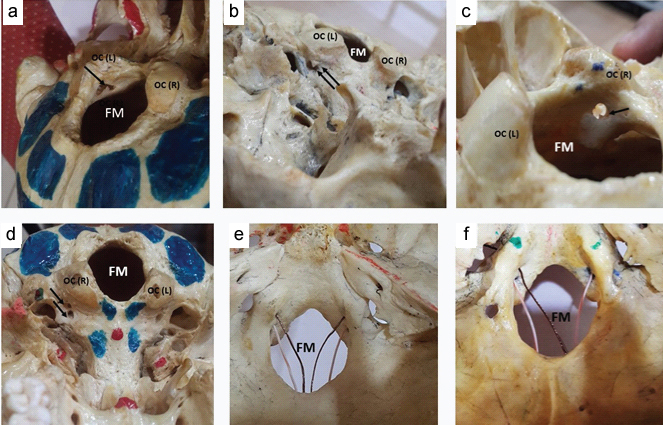
The morphological variations of HC are described in [Table/Fig-3,4]. The spur and septa in the HC were observed in 52% skulls. In some cases, spur and septa both were observed simultaneously in single HC. Type 2 HC was seen in 28% skulls and Type 3 HC in 26% skulls. Type 4 HC was not found in our study. Type 2 and Type 3 both had unilateral predominance with more frequency on left side.
Morphological parameters of HC- Frequency of osteotic variations in HC and its distribution in 50 dry skulls.
| Sl no. | Type | n=Number of skulls | Total % |
|---|
| 1. | Type 1 | 24 | 48% |
| 2. | Type 2 (Spur) | | Unilateral | Bilateral | 28%* |
| Right | Left |
| N | % | N | % | N | % |
| a | 2 | 4 | - | | 2 | 4 |
| b | 2 | 4 | 4 | 8 | 2 | 4 |
| c | - | | 2 | 4 | - | |
| 3. | Type 3(Incomplete septa) | a | - | | 2 | 4 | - | | 26%* |
| b | - | | 3 | 6 | 5 | 10 |
| c | 2 | 4 | 1 | 2 | - | |
| 4. | Type 4 (Complete septa) | - | | - | | - | | Absent |
* In some cases, spur and septa were seen in same skull at different locations of HC
Showing osteotic variations in the HC: a)- Spur near internal opening of HC (Type 2B); b) Spur near external opening of HC (Type 2A); c) Spur in the middle of HC (Type 2C); d) Incomplete septa in the HC near external opening forming double external opening of HC (Type 3A) (Unilateral); e) Bilateral incomplete septa in the HC near internal opening forming double internal opening of HC (Type 3B); f) Unilateral incomplete septa in the HC near internal opening forming double internal opening of HC (Type 3B). OC(L)- occipital condyle left, OC(R)- occipital condyle right, FM- foramen magnum, arrow- showing spur or septa in the HC.
Morphometric study
The morphometric study of HC and its distance from OC is shown in [Table/Fig-5]. The distance of external and internal openings of HC from posterior end of OC was more on the left side. The anterior angle of HC to the midsagittal plane was 32.08±2.6 on the right side and 31.96±3.2 on the left side. Posterior angle of HC to the midsagittal plane was 33.5±3.1 on the right side and 35±4.7 on the left side.
Morphometric parameters of HC-1,2. Distance of the posterior end of OC from external and internal opening of HC. 3. Angle of Inclination of the HC with the midsagittal plane.
| Sl. No | Parameters | Right | Left | p-value |
|---|
| Total (n=50) | Total (n=50) |
|---|
| Range | Mean±(SD) | Range | Mean±(SD) |
|---|
| 1. | Distance of posterior end of OC from external opening of HC (mm) | 6.3-19.4 | 13.83±2.9 | 11.3-19.7 | 15.02±1.9 | 0.006* |
| 2. | Distance of posterior end of OC from internal opening of HC (mm) | 5.3-19.1 | 10.66±2.7 | 7.5-20.1 | 11.89±2.9 | 0.010* |
| 3 | Anterior angle of inclination of HC to midsagittal plane (in degree)** | 28-34 | 32.08±2.6 | 26-40 | 31.96±3.2 | 0.56 |
| Posterior angle of inclination of HC to midsagittal plane (in degree)*** | 29-36 | 33.5±3.1 | 29-42 | 35±4.7 | 0.87 |
* Significant p < 0.05, **in case of double internal opening of HC (type 3), anterior opening was considered alongwith the single internal opening of the HC (Type1 and Type 2), *** in case of double internal opening of HC (type 3), posterior opening was considered
Discussion
HC is directed anterolaterally, surrounded by the OC inferiorly, the sphenoid portion of the clivus superomedially and the jugular foramen and jugular process of the occipital bone laterally [7–9]. The osteotic variations of HC is clinically significant in view of delicate neurovascular structures traversing through it. The spurs and septa in the canal will divide it into compartments which may compress these structures. Signs of venous compression appear earlier as compared to the neural deficity [10]. The tumours like hypoglossal nerve schwannomas, posterior cranial fossa meningiomas and jugulo-tympanic paragangliomas are common in HC [4]. Any osteotic variations in HC will further complicate these situations compelling surgeons to be well aware of such variations.
The lesions that are commonly encountered around the foramen magnum, lower clivus, and ventral aspect of the upper cervical spine include intra and extradural tumours, vascular lesions of the vertebral artery and congenital lesions [11]. Different surgical approaches like ventral and dorsal to OC were taken into consideration but the ventral approach was linked with unacceptably high mortality and morbidity rates and incomplete tumour removal [6]. Now-a-days, TCA has been used more frequently which enables shorter and more direct route to the anterior part of pontomedullary junction with minimal brainstem retraction. It requires drilling of the posterior part of the OC which endangers the opening of the HC leading to the damage of the neurovascular structures [10]. For these reasons, surgeons should know the osteotic variations in HC and the topographic relationship between the HC and the area of the OC to be removed.
The morphological study of incidence of spur and septa in the HC was compared to other studies in [Table/Fig-6]. Spur and septa both were more frequent on the left side in our study while Paraskevas GK et al., [6] in Greek population observed variations more frequently on the right side. In the present study, the spur was observed in 28% of skulls which was comparable to the findings of Paraskevas GK et al., (18.96%) and Bastianini A et al., (35%) but Singh V et al., reported 4.32% in Indian population which is lower as compared to our study [4,6,12]. The incomplete septa were seen in 26% skulls, out of which in 16% skulls it was near internal opening of HC, 6% in the midway and 4% near the external opening. Incomplete septa were also reported by Singh V et al., near internal opening in 11.36% but they did not find any septa near external opening of HC. None of the researchers had reported the presence of septa in the middle of HC. The total number of incomplete septa in our study was similar when compared to study by Paraskevas GK et al., (19.86%) and Bastianini A et al., (15-30%). Complete septa were not seen in our study like Singh V et al., but it has been reported by Paraskevas GK et al., and Bastianini A et al., ranging from 1-3% [4,6,12]. Other authors like Zaidi SHH et al.,, Nikumbh RD et al.,, Muthukumar N et al., in Indian population, Katsuta T et al., in US and Indian population, Natsis K et al., in Greek population and Avci E et al., in Turkish population reported the septa and double HC in 10-30% skulls but none of them mentioned the location and extent of septa [10,13–17]. HC develops by fusion of occipital sclerotome and process of occipital chondrification at stage 17 mm while development of hypoglossal nerve occurs at stage 12 mm. Developmentally the nerve originates from several segments forming rootlets which enter into hypoglossal foramen and get enveloped in fibrous sheath to form two or more nerve bundles hence, explaining the canal into two or more compartments. Most of the skull bones are derived from neural crest mesenchyme and any defect in molecular regulation of these cells through HOX genes via fibroblastic growth factors may be the causative factor of duplication of the HC [18,19].
Comparison of the incidence of spur and septa in the HC with previous studies.
| Researchers & year | Population | No. of skulls | Spur | Double HC |
|---|
| Incomplete septa* | Complete septa** |
|---|
| Intra cranial opening | Midway | Extra cranial pening |
|---|
| Present study | North Indian | 50 | 28% | 16% | 6% | 4% | Nil |
| Paraskevas GK et al., [6] | Greek | 116 | 18.96% | 19.83% | Nil | Nil | 1.72% |
| Bastianini A et al., [12] | Sienese | 300 | 35% | 15-30% | Nil | Nil | 1-3% |
| Singh V et al., [4] | Indian | 625 | 4.32% | 11.36% | Nil | Nil | Nil |
| Zaidi SHH et al., [13] | North Indian | 40 | - | 12.5% | Nil | Nil | Nil |
| Nikumbh RD et al., [14] | Indian | 100 | - | 28% | Nil | Nil | Nil |
| Muthukumar N et al., [15] | South Indian | 50 | - | 30% | Nil | Nil | Nil |
| Katsuta T et al., [10] | US and Indian | 30 sides | - | 10% | Nil | Nil | Nil |
| Natsis K et al., [16] | Greek | 143 | - | 25.5% | Nil | Nil | Nil |
| Avci E et al., [17] | Turkish | 30 | - | 30% | Nil | Nil | Nil |
*, ** Incomplete and complete septa will divide HC into double HC partially and completely respectively
The location of the extracranial and intracranial openings of the HC may affect the lateral approaches to the craniovertebral junction. The distance between the HC and the posterior border of the OC is critical. This measurement gives an indication about the maximum amount of resectable condyle without entering the HC. In the present study, the mean distance of posterior end of OC from external and internal opening of HC was 14.4 mm and 11.3 mm respectively. Similar to our study, Muthukumar N et al., Kizilkanat ED et al., and Parvindokht B et al., reported that the distance from the intracranial end of the HC to the posterior margin of the OC ranges from 11.42 mm-12.3 mm [15,20,21]. On the other hand, Kalthur SG et al., Wen HT et al., and Avci E et al., reported the distances lower than our findings [Table/Fig-7] [5,17,22].
Comparison of the distance of posterior end of OC to the internal opening of HC with previous studies.
| Researchers | Population | No. of Skulls | Distance of Posterior End of OC to the Internal Opening of HC |
|---|
| Range | Average Distance |
|---|
| Present study | North Indian | 50 | 5-20 mm | 11.3 mm |
| Muthukumar N et al., [15] | South Indian | 50 | 9-16 mm | 12.2 mm |
| Kalthur SG et al., [22] | South Indian | 71 | 5-10 mm | 7.5 mm |
| Parvindokhtb et al., [21] | Iranian | 26 | 9-14 mm | 11.42 mm |
| Kizilkanat ED et al., [20] | Turkish, Caucasian | 59 | - | 12.3 mm |
| Wen HT et al., [5] | USA | 12 | 06-10 mm | 08.4 mm |
| Avci E et al., [17] | Turkish | 30 | - | 9.9 mm |
In our study, the anterior angle of inclination of HC to the midsagittal plane was less as compared to the posterior angle of inclination in case of double internal opening. The angle of inclination reported by Muthukumar N et al., and Paraskevas GK et al., was higher as compared to our study [Table/Fig-8] [15,6].
Comparison of the angle of HC to midsagittal plane with previous studies.
| Researchers & year | Population | No. of skulls | Angle of HC to midsagittal plane |
|---|
| Anterior angle | Posterior angle |
|---|
| Present study | North Indian | 50 | 32° | 34° (R) and 35° (L) |
| Muthukumar N et al., (2005) [15] | South Indian | 50 | 49° |
| Paraskevas GK et al., (2009) [6] | Greek | 116 | 42.3° (R) and 32.4° (L) |
Limitation
The limitation of our study is that the age and gender of the skulls is not known which could be a factor that affect the morphology of the HC. We did only osteological study but radiological techniques can also be applied. In addition, we did not consider the pathological skulls, so we could not estimate how the degenerative forces can affect the morphology and morphometry of HC and surrounding areas.
Conclusion
Our study has confirmed the presence of spur/septa in HC in more than half of the skulls of North Indian population studied which is higher as compared to other studies. Unilateral variations were more frequent and especially on the left side. The distance of posterior part of OC to the internal opening of HC was 11 mm which can be drilled safely during TCA. In addition, angle of inclination of HC to the midsagittal plane was also measured. Awareness of morphologic and morphometric variations of HC will further help the neurosurgeons in performing surgeries in this area with minimal damage to neurovascular structures in the HC. We believe use of preoperative imaging studies can be helpful in studying the above-mentioned features in an individual and thus, can help the surgeon in choosing the correct approach and the extent of bony resection.
*, ** Incomplete and complete septa will divide HC into double HC partially and completely respectively