Hyperlipidemia is very common in general population and incidence has further increased in recent years. Evaluation of patient presenting with lipid disorders is essential to obtain a definite diagnosis to prevent complications, and apply the most appropriate treatment. An isolated elevation in triglyceride levels may be caused by a primary disorder of lipid metabolism like familial hypertriglyceridemia. It may also arise secondary to a number of conditions like diabetes mellitus, alcohol intake, hypothyroidism, drugs, infections and nephrotic syndrome. Herein, we describe a case of secondary hypertriglyceridemia leading to Nonalcoholic Steatohepatitis (NASH) in a young female which was attributed to Multiple Myeloma (MM). Significant reduction in triglyceride levels after starting anti-myeloma therapy established their relation. This is the first case of light chain myeloma causing severe secondary hypertriglyceridemia.
Hyperlipidemic myeloma, Lipoprotein lipase, Multiple myeloma, Nonalcoholic steatohepatitis
Case Report
A 35-year-old married lady presented with complaints of weight loss for two months and fever for three days. She had lost almost 10 kg of weight in last two months although her appetite was normal. Fever was high grade, intermittent, associated with chills but not rigors. She was a known case of hypothyroidism for six years and was on regular treatment. There was no family history of dyslipidemia or premature coronary artery disease. On physical examination she had BMI of 22.8 kg/m2, mild pallor and no significant lymphadenopathy. Pulse rate was 90 beats per minute, regular and blood pressure was 130/70 mm Hg in right arm, supine position. Liver was palpable 5 cm below right costal margin, firm in consistency and non tender. Rest of systemic examination including fundus was essentially normal.
Blood examination showed haemoglobin (Hb) of 9.8 g/dL, Total Leukocyte Count (TLC) of 10,100/cu mm with 78% neutrophil and 21% lymphocyte, MCV-78 fl, MCH-32.8 pg, MCHC-36.5 g/dl and Erythrocyte Sedimentation Rate (ESR) of 56 mm/hr. Peripheral smear showed normocytic, normochromic anaemia. Liver Function Test (LFT) was mildly deranged. Serum bilirubin-1.1 mg/dl, SGOT-180 U/L, SGPT-144 U/L, total protein-5.2 g/dl, albumin-2.9 g/dl and globulin-2.3 g/dl. Fasting blood sugar and renal function tests were normal. Urine examination showed trace proteinuria with 30-35 pus cells/hpf. Blood culture was sterile but urine culture grew E. coli which was sensitive to piperacillin/tazobactam and meropenem. Serum TSH was 1.5 mIU/L. Tests for viral hepatitis (Anti HAV, HBsAg, Anti HCV, Anti HEV) and HIV were negative. Serum electrolytes (sodium, potassium, calcium, phosphorus, chloride) were also normal. Serum amylase and lipase levels were normal. Abdominal ultrasonography showed hepatomegaly (liver size 18 cm) with severe fatty infiltration. A fasting lipid profile was done in view of severe fatty liver which showed serum Triglycerides (TG) of 1460 mg/dl, Total Cholesterol (TC)-205 mg/dl, LDL-141 mg/dl, HDL-17 mg/dl and VLDL 47 mg/dl. Extended lipid profile showed TG of 1346 mg/dl (N:<150), TC-195 mg/dl (N:<200), LDL-141mg/dl (N<100), VLDL-47.6 mg/dl (N:<30), HDL-5.90 mg/dl (N:40-60), Apo A1 <25 mg/dl (N:105-205), Apo B 111 mg/dl (N:55-130), Apo B/Apo A1 ratio 13.95 (0.35-0.98), Lp(a) < 5 and chylomicrons were present. Lipoprotein Lipase (LPL) assays couldn’t be done due to its unavailability in our institute.
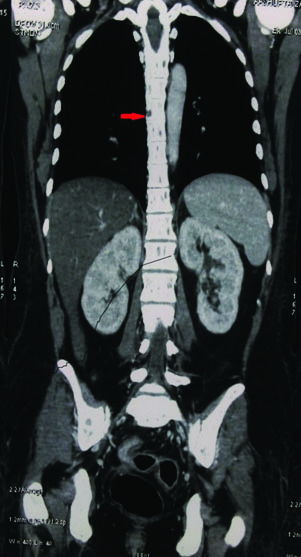
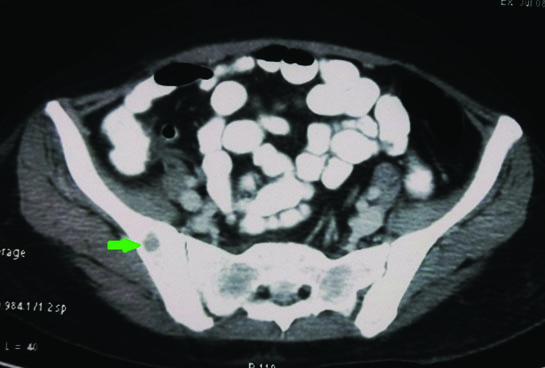
Contrast Enhanced Computed Tomography (CECT) abdomen and chest showed fatty liver with multiple lytic lesions in dorsolumbar spine, S1 vertebrae, both pelvic bones, proximal femur, manubriosternum, both humerus, both scapula and medial end of left clavicle [Table/Fig-1,2 and 3]. Serum Protein Electrophoresis (SPEP) showed M band in gamma region and elevated lambda chain on immunofixation. Urine for Bence-Jones protein was positive. Serum immunoglobulin levels were decreased significantly: serum IgG: 357 mg/dl (N:700-1600), IgM: <20 mg/dl (N:40-230) and IgA: <10 mg/dl (N:70-400). Serum LDH was 411 IU/L (N:150-350).
Coronal section of CT chest and abdomen showing multiple lytic lesions in dorsolumbar spine (arrow).
Transverse section of CT pelvis showing lytic lesions in iliac bone (arrow).
Hepatomegaly with fatty infiltration on transverse section of CT abdomen (star).

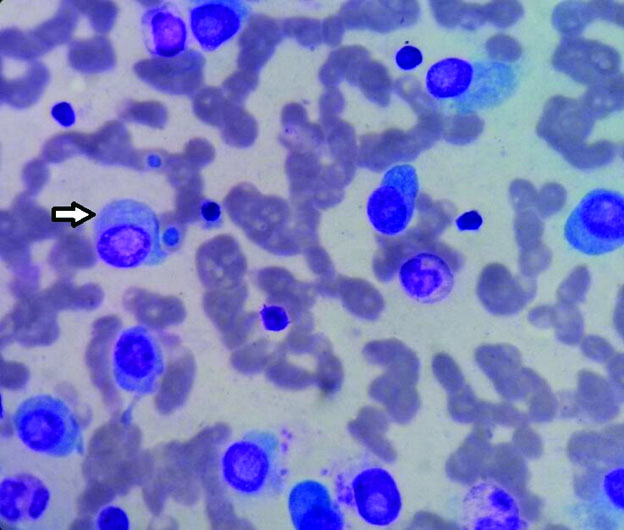
Bone marrow aspiration showed markedly hypercellular marrow with sheets of abnormal plasma cells (63%). Erythroid precursors were significantly decreased and only few megakaryocytes were seen [Table/Fig-4]. Bone marrow biopsy showed plenty of plasma cells, was positive for CD138 and lambda immunostain and was negative for kappa immunostain. This was suggestive of plasma cell dyscrasia.
Bone marrow aspirate smear showing sheets of abnormal immature plasma cells (arrow).
Thus, a diagnosis of light chain myeloma with hypertriglyceridemia, NASH and Urinary Tract Infection (UTI) was made and haematologist consultation was taken. Broad spectrum antibiotics were given for UTI, before starting myeloma therapy. Lipid lowering agents like statin and fenofibrate were given, but there was no significant change in lipid parameters. She received induction therapy with bortezomib, cyclophosphamide and dexamethasone. Repeat lipid profile after two cycles of chemotherapy showed TG of 184 mg/dl, TC-171 mg/dl, LDL-95 mg/dl, HDL-50 mg/dl and normal Apo A1, Apo B levels. At present she is on regular chemotherapy and is planned for autologous hematopoietic cell transplantation.
Discussion
Multiple myeloma is a common haematological malignancy characterized by neoplastic proliferation of plasma cells. There is infiltration of bone by plasma cells causing lytic lesions and various other systemic manifestations like fatigue, weight loss, bone pain, anaemia, hypercalcaemia, renal impairement. Diagnosis is made by presence of more than 10% plasma cells in bone marrow with features of organ impairement (hypercalcaemia, renal insufficiency, anaemia and bony lesions). The basic pathology in MM is production of abnormal Monoclonal (M) protein by malignant plasma cells which is seen as M spike in SPEP. This immunoglobulin type can be detected by immunofixation and can be heavy chain, light chain, both or none [1]. IgG is the most common immunoglobulin produced and kappa is the predominant light chain isotype in MM, except in IgD myeloma where lambda light chain is more frequently seen [2].
Hypertriglyceridemia (HTG) is defined by TG levels more than 150 mg/dl, it could be either familial or acquired. Further it is classified into mild (150-199 mg/dl), moderate (200-999 mg/dl), severe (1000-1999 mg/dl) and very severe (>2000 mg/dl). HTG is generally detected during routine investigation and in a survey done in United States almost 33 percent of the adult population were found to be having HTG [3]. Acquired causes include uncontrolled diabetes, nephrotic syndrome, obesity, hypothyroidism, drugs (oestrogen replacement, tamoxifen, oral contraceptives, anti retroviral therapy, steroids) and pregnancy. MM is a rare cause of HTG and is called as Hyperlipidemic Myeloma (HLM) when associated with dyslipidemia.
HLM is a very rare variant of MM and its pathogenesis remains elusive. Most common lipid abnormality in MM is low cholesterol levels and only a minority of these patients have high cholesterol or triglyceride levels [4]. IgA gammopathy is present in almost half of these patients and no case of only light chain myeloma with HLM has been reported so far. In a review of HLM cases it was found that hyperlipidemia preceded myeloma in most of the patients and skin xanthoma was present in almost 70% of these patients [5]. Hyperviscosity syndrome and atherosclerosis have been also documented in HLM [6]. Lipid lowering agents are not very useful in HLM associated dyslipidemia and most of the patients respond well to MM chemotherapy [7]. We did give lipid lowering drugs to our patient but there was no significant decrease in triglyceride levels and lipid profile normalized only after chemotherapy.
The exact pathogenesis is not known and various hypothesis have been proposed. Hyperlipidemia can be caused by either increased synthesis or reduced clearance of lipids. It is believed that in HLM, M protein binds with LDL and IDL resulting in reduced receptor mediated clearance in liver [8]. Hyperlipidemia is often seen with high levels of paraprotein, and a subsequent decrease in its level causes lowering of lipid levels. Few researchers have also postulated that paraprotein in HLM binds with LPL and prevents degradation of triglyceride rich lipoproteins [9]. In our case lipid profile suggested presence of chylomicron, significantly raised triglyceride levels, mild elevation of VLDL and LDL with low HDL and Apo A1 levels. The possible explanation for this derangement could be inhibition of LPL by light chain paraprotein. A decrease in LPL levels impairs clearance of chylomicrons and VLDL, resulting in hypertriglyceridemia. Also, LPL facilitates cholesterol transfer from other lipoproteins to HDL and in case of LPL deficiency, HDL levels are often low [10].
Conclusion
Every case of dyslipidemia should be evaluated for a secondary cause as it could be the only manifestation of a serious disease like multiple myeloma. An early diagnosis and effective treatment of primary disease can successfully reverse the lipid abnormality.
[1]. Kyle R, Gertz M, Witzig T, Lust J, Lacy M, Dispenzieri A, Review of 1027 Patients With Newly Diagnosed Multiple MyelomaMayo Clinic Proceedings 2003 78(1):21-33. [Google Scholar]
[2]. Bladé J, Lust JA, Kyle RA, Immunoglobulin D multiple myeloma: Presenting features, response to therapy, and survival in a series of 53 casesJ Clin Oncol 1994 12(11):2398-404. [Google Scholar]
[3]. Ford E, Li C, Zhao G, Pearson W, Mokdad A, Hypertriglyceridemia and its pharmacologic treatment among US adultsArch Intern Med 2009 169(6):572 [Google Scholar]
[4]. Kyle RA, Multiple myeloma: Review of 869 casesMayo Clin Proc 1975 50(1):29-40. [Google Scholar]
[5]. Misselwitz B, Goede JS, Pestalozzi BC, Schanz U, Seebach JD, Hyperlipidemic myeloma: Review of 53 casesAnn Hematol 2010 89(6):569-77. [Google Scholar]
[6]. Mehta J, Singhal S, Hyperviscosity syndrome in plasma cell dyscrasiasSemin Thromb Hemost 2003 29(5):467-71. [Google Scholar]
[7]. Fukudome K, Kato J, Ohashi T, Yamamoto Y, Eto T, Hyperlipidemia associated with multiple myelomaIntern Med 1996 35(4):337-40. [Google Scholar]
[8]. Nozaki S, Ito Y, Nakagawa T, Yamashita S, Sasaki J, Matsuzawa Y, Autoimmune hyperlipidemia with inhibitory monoclonal antibodies against low density lipoprotein binding to fibroblasts in a case with multiple myelomaIntern Med 1997 36:920-25. [Google Scholar]
[9]. Glueck CJ, Kaplan AP, Levy RI, Greten H, Gralnick H, Fredrickson DS, A new mechanism of exogenous hyperglyceridemiaAnn Intern Med 1969 71:1051-62. [Google Scholar]
[10]. Nordestgaard BG, Abildgaard S, Wittrup HH, Steffensen R, Jensen G, Tybjaerg-Hansen A, Heterozygous lipoprotein lipase deficiency: Frequency in the general population, effect on plasma lipid levels, and risk of ischemic heart diseaseCirculation 1997 96(6):1737 [Google Scholar]