Case Report
A 37-year-old female came with complaint of swelling in the right axilla noticed since one and a half month. The swelling was apparently constant in size without any pain or discharge. Clinically suspecting it to be axillary lymphadenopathy, the patient was referred for fine needle aspiration. On examination, a subcutaneous nodule measuring 2 cm x 1.5 cm was felt within a soft, boggy, superficial mass which was isolated from the breast in the right axilla. The nodule was firm, well-defined, freely mobile and non-tender with normal overlying skin. No nodules were palpable in the contralateral axilla or bilateral breasts.
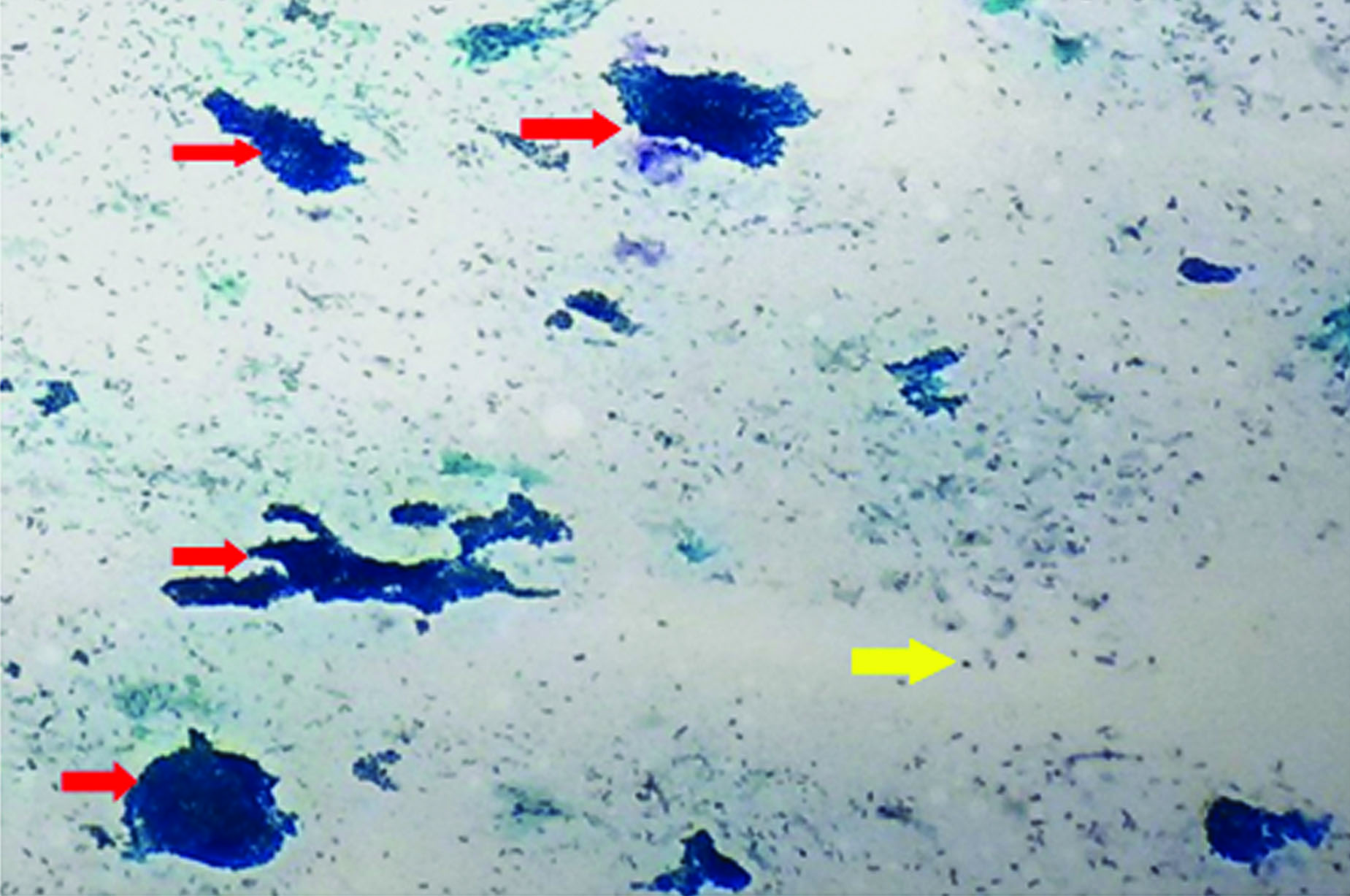
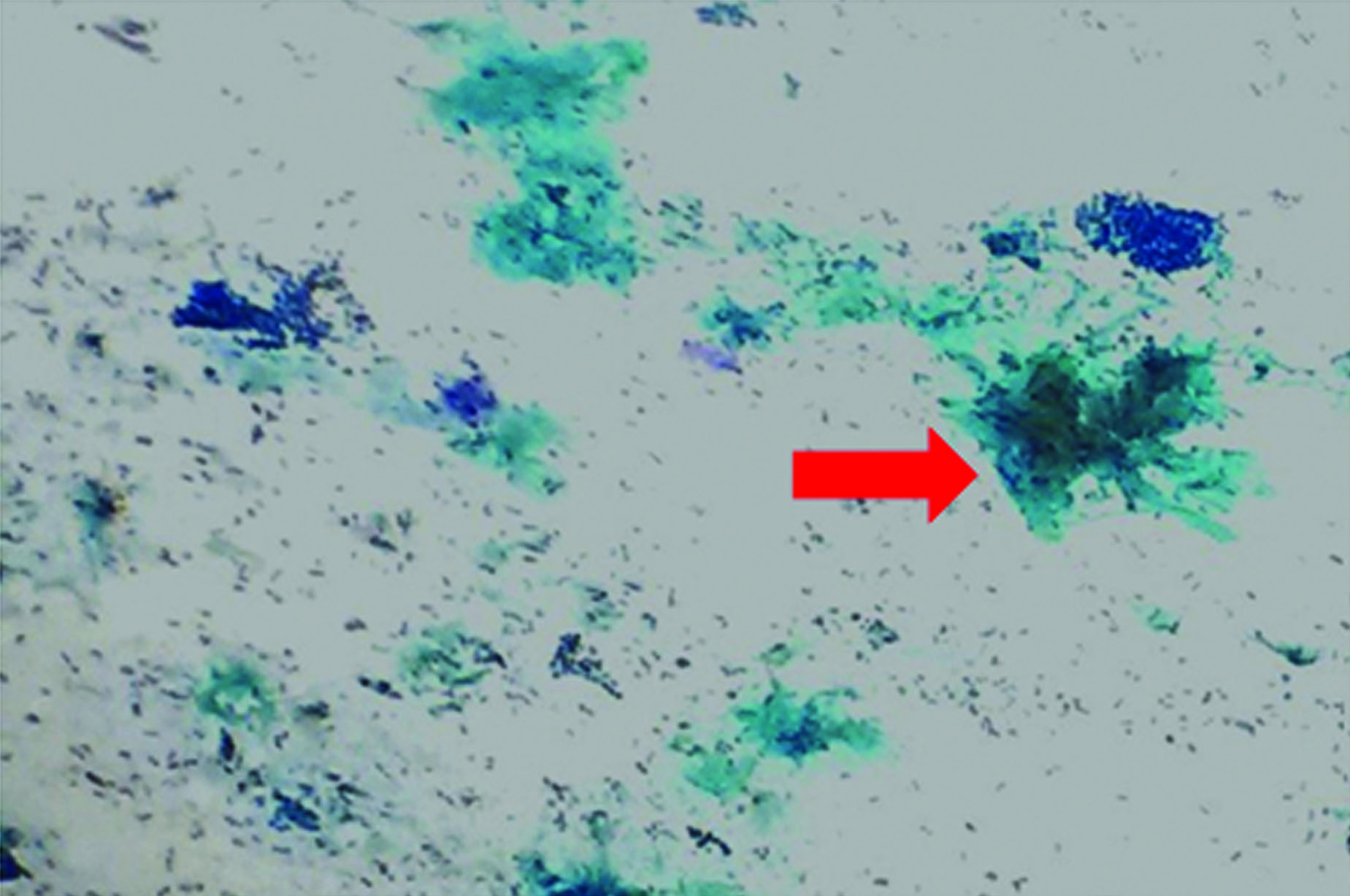
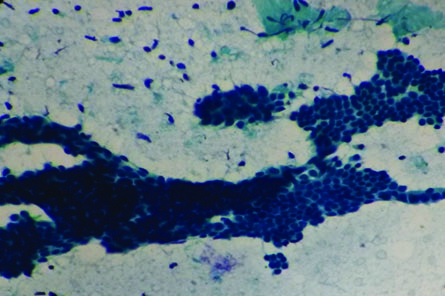
Under all aseptic precautions, a fine needle aspiration was performed which yielded a blood mixed aspirate. Smears were prepared and stained with the Papaniculaou (PAP) stain using the Rapid PAP technique. Smears revealed moderate cellularity with bimodal pattern containing epithelial and stromal fragments [Table/Fig-1,2]. The duct epithelial cells were arranged in cohesive clusters forming elongated, branching staghorn like pattern interspersed with myoepithelial cells [Table/Fig-3]. The individual cells were uniform with nuclei showing bland granular chromatin. Background showed numerous single bare bipolar nuclei along with fragments of fibromyxoid stroma. However, no lymphoid cells were seen, thus ruling out lymphadenopathy. Hence, based on this cytopathological examination, we diagnosed it to be a fibroadenoma within the axillary ectopic breast tissue. Unfortunately, the patient was lost to follow up.
Papaniculaou (PAP) stained smear showing moderate cellularity comprising of duct epithelial cells (red arrows) and bare bipolar nuclei in the background (yellow arrow) (PAP; 4X) (left).
Papaniculaou (PAP) stained smear showing stromal fragments (red arrow) (PAP; 4X) (middle).
Papaniculaou (PAP) stained smear showing benign duct epithelial cells in branching staghorn like pattern with overlapping myoepithelial cells (PAP; 40X) (right).
Discussion
When breast tissue (glandular component/ nipple areola complex/ both) occurs at sites other than the two pectoral regions, it is termed as EBT/supernumerary breasts/accessory breasts. It mostly occurs along the milk line which extends from the mid axilla to the medial groin [1]. EBT may occur unilaterally or bilaterally. Approximately 67% of accessory breast tissue occurs in the thoracic or abdominal portions of the milk line often just below the infra mammary crease, more often on the left side of the body [2], and only 20% of accessory breast tissue occur in axilla. The remaining (13%) of these occur anywhere along the milk line [2,3]. Cases of polymastia have also been reported on other sites such as the face [4], foot [5], lumbar region, vulva and perineum [6].
The incidence of EBT is 0.4%-6% amongst women [3,7] and the disease occurring in these is still rarer. The incidence of EBT in the male population is 50% of that of in females [3]. This tissue is prone to similar diseases viz., fibrocystic changes, mastitis, intraductal papillomas, abscesses, fibroadenoma, carcinomas and phyllodes tumour like the normal breast [7]. Hence, we need to recognise a swelling (especially, one occurring along the milk line) as being EBT and further evaluate it for early diagnosis of the diseases.
Supernumerary breast can present as either polythelia that is presence of ectopic breast tissue with a nipple-areolar complex, or as polymastia comprising of only glandular tissue without the nipple-areola complex, making it more difficult to diagnose. Polymastia occurs due to regression of ectodermal element of the skin but a normal proliferation of mesenchyme [8].
During the fifth or sixth week of embryonic development, two ectodermal thickenings (mammary ridges or milk lines) develop on the ventral surface of the embryo and extend in a curvilinear fashion convex towards the midline. These extend from the anterior axillary folds to the inside of the inguinal folds. In normal development, most of the embryologic mammary ridges resolve, except for two segments in the pectoral region, which later become breasts. Failure of any portion of the mammary ridge to involute can lead to ectopic breast tissue. Therefore, ectopic breast usually occurs along the “milk line” or mammary line [9].
The occurrence of ectopic breast tissues in locations other than the milk line can be explained by two hypotheses. Either it can represent a migratory arrest of breast primordium during chest wall development [10] or this occurrence can be attributed to its development from the modified apocrine sweat glands [11].
A classification system for supernumerary breast tissue was given by Kajava Y [12]. Accordingly,
Class I consists of a complete breast with nipple, areola and glandular tissue.
Class II consists of nipple and glandular tissue but no areola.
Class III consists of areola and glandular tissue but no nipple.
Class IV consists of glandular tissue only.
Class V consists of nipple and areola but no glandular tissue (pseudomamma).
Class VI consists of polythelia.
Class VII consists of an areola only (polythelia areolaris).
Class VIII consists of a patch of hair only (polythelia pilosa).
Our case belonged to Class IV. Patients with polythelia have been associated with urinary tract abnormalities such as supernumerary kidneys, failure of renal formation, renal adenocarcinoma, hydronephrosis, polycystic kidney disease, duplicate renal arteries and ureteric stenosis. This association can be partly explained by the parallel development of mammary structure and genitourinary system [13]. Also, seen are other congenital anomalies such as pyloric stenosis, epilepsy and cardiac abnormalities [3].
When a nodule is detected in the axillary region, the differential diagnosis includes enlargement of lymph nodes, lipomas, tuberculosis, neuromas, axillary tail of Spence, skin lesions such as epidermal inclusion cysts, sebaceous cyst, suppurative hidradenitis, vascular lesions and lesions arising from EBT [3,7,13]. As detailed earlier, EBT can be affected by same diseases as the normal breast, carcinoma being the most common [7,13]. Hence, these swellings need to be evaluated at the earliest for development of any nodules.
Rizvi G et al., have described a similar case as ours, in a 32-year-old female which was clinically diagnosed to be fat hypertrophy. Fine needle aspiration was helpful in their case too [1]. Kohli S et al., have reported fibroadenoma in right sided axillary ectopic breast tissue in a 34-year-old female with bilateral axillary accessory breasts. A combination of mammogram, ultra sonogram, colour flow Doppler and fine needle aspiration were used to diagnose the lesion prior to surgery [14].
An unusual case of juvenile fibroadenoma was reported by Borsook et al., in a 10-year-old female. The patient was a known case of mitochondrial disease with mutation in the POLG1 gene and had presented with a left axillary mass of 10 months duration. Suspecting it to be a lymph node in this case too, the mass was excised in an attempt to rule out lymphoma but histopathological examination proved it to be a fibroadenoma [15].
In our case, the patient might not have noticed the ectopic breast tissue earlier. She was a null gravida, further explaining the fact that she ignored the axillary ectopic breast as pad of fat. Accessory breasts are known to undergo enlargement and cause discomfort with hormonal stimulation. It came to her notice only after it developed a fibroadenoma, forming a well-defined nodule. Axillary tail of Spence is axillary accessory breast tissue that is connected with outer part of normal thoracic breast tissue and is located deep. In our patient, axillary nodule was separate from the breast and was situated superficially. Hence it was EBT and not extension of the breast parenchyma in the axilla. FNAC was a quick and cost effective procedure giving a definite diagnosis and ruling out tuberculosis and more importantly malignancy.
Conclusion
While dealing with swellings in the axilla, a differential of an EBT should always be borne in mind because though rare, it requires prompt diagnosis for further management. FNAC is a quick, cost effective procedure tolerated well by most patients. It is reliable to differentiate benign from malignant lesions, giving earlier diagnosis to plan for definitive management. Hence, FNAC can be considered as the first diagnostic tool for palpable lesions.
[1]. Rizvi G, Pandey H, Gupta M, Fibroadenoma of ectopic breast tissue in axillaJournal of Case Reports 2012 2:36-38. [Google Scholar]
[2]. Nayak S, Acharjya B, Devi B, Polymastia of axillaeIndian Journal of Dermatology 2007 52(2):118 [Google Scholar]
[3]. Goyal S, Sangwan S, Singh P, Bawa R, Fibroadenoma of axillary ectopic breast tissue: A rare clinical entityClinical Cancer Investigation Journal 2014 3(3):242 [Google Scholar]
[4]. Koltuksuz U, Aydin E, Supernumerary breast tissue: A case of pseudomamma on the faceJournal of Pediatric Surgery 1997 32(9):1377-78. [Google Scholar]
[5]. Conde DM, Kashimoto E, Torresan RZ, Alvarenga M, Pseudomamma on the foot: an unusual presentation of supernumerary breast tissueDermatology Online Journal 2006 12(4):7 [Google Scholar]
[6]. Chung-Park M, Liu CZ, Giampoli EJ, Emery JD, Shalodi A, Mucinous adenocarcinoma of ectopic breast tissue of the vulvaArchives of Pathology and Laboratory Medicine 2002 126(10):1216-18. [Google Scholar]
[7]. Rong X, Zhu Q, Jia W, Ma T, Fang Y, Zhou Y, Fibroadenoma of the ectopic axillary breast tissue: sonographic appearancesOpen Journal of Clinical Diagnostics 2014 04:205-11. [Google Scholar]
[8]. Langman J, “Medical Embryology.” 1975 3rd edBaltimoreThe Williams and Wilkins Company [Google Scholar]
[9]. Shin SJ, Sheikh FS, Allenby PA, Rosen PP, Invasive secretory (juvenile) carcinoma arising in ectopic breast tissue of the axillaArchives of Pathology and Laboratory Medicine 2001 125(10):1372-74. [Google Scholar]
[10]. Breast Embryology: Overview, The Integument, The Embryologic Breast [Internet]. Emedicine.medscape.com. Available from: http://emedicine.medscape.com/article/1275146-overview#aw2aab6b8 [Google Scholar]
[11]. Craigmyle M, The apocrine glands and the breast 1984 1st edChichesterWiley [Google Scholar]
[12]. Kajava Y, The proportions of supernumerary nipples in the Finnish populationDuodecim 1915 1:143-70. [Google Scholar]
[13]. Amaranathan A, Balaguruswamy K, Bhat R, Bora M, An ectopic breast tissue presenting with fibroadenoma in axillaCase Reports in Surgery 2013 2013:1-3. [Google Scholar]
[14]. Kohli S, Garg P, Kharkwal S, Verma A, Rare clinical entity- Fibroadenoma of ectopic breast tissueIndian Journal of Basic and Applied Medical Research 2015 5(1):575-78. [Google Scholar]
[15]. Borsook J, Thorner PS, Grant R, Langer JC, Juvenile fibroadenoma arising in ectopic breast tissue presenting as an axillary massJ Pediatr Surg Case Rep 2013 :1359-61. [Google Scholar]