Nasal NK/T Cell Lymphoma Presenting with Perforation of Palate: A Case Report and Review of Literature
Shreyas N Shah1, Priyank R Mistry2, Girish R Chauhan3, Vishal Chauhan4, Jayshankar Pillai5
1 Assistant Professor, Department of Oral Pathology, KM Shah Dental College and Hospital, Sumandeep Vidyapeeth, Vadodara, Gujarat, India.
2 Senior Resident, Department of Ear, Nose and Throat, Parul Institute of Medical Sciences and Research, Vadodara, Gujarat, India.
3 Assistant Professor, Department of Oral Pathology, Government Dental College and Hospital, Jamnagar, Gujarat, India.
4 Assistant Professor, Department of Prosthodontics, Government Dental College and Hospital, Ahmedabad, Gujarat, India.
5 Tutor, Department of Oral Pathology, Government Dental College and Hospital, Ahmedabad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Priyank R Mistry, Senior Resident, Department of Ear, Nose and Throat, Parul Institute of Medical Sciences and Research, Vadodara-391760, Gujarat, India.
E-mail: priyankmistry_09@yahoo.co.in
Nasal Natural Killer (NK)/T cell lymphoma, commonly mentioned in the literature as Lethal Midline Granuloma (LMG) is an unusual pathology of the oro-maxillo-facial region characterized by aggressive and progressive destruction of the face, nose, palate and pharynx. This disease is now classified as a T-cell lymphoma based on modern cytogenetics, immunologic and molecular studies. However, it is mentioned in various literatures by various names. Here, we present one such clinically diagnosed, histopathologically and immunologically confirmed case of LMG, designated as NK/T cell lymphoma in a 56-year-old male. The uncommon presentation of NK/T cell lymphomas should be kept as a differential diagnosis for management of patients.
Idiopathic midline destructive diseases, Lethal midline granuloma, Positron Emission Tomograhy-Computed Tomography
Case Report
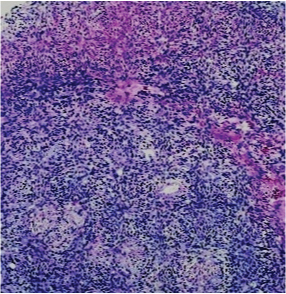
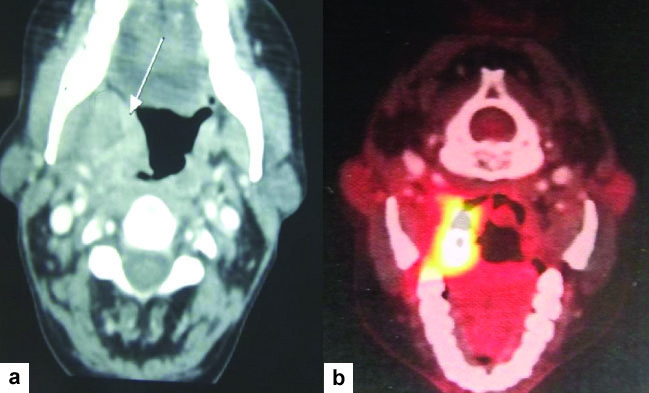
A 56-year-old male patient presented with chief complaint of nasal regurgitation of food and difficulty in swallowing since four months. Intraoral examination revealed palatal perforation measuring around 2 cm x 1.5 cm at the junction of hard and soft palate [Table/Fig-1]. All the routine haematological and biochemical investigations were normal except for a raised ESR. Punch biopsy was taken and culture sensitivity tests were done. The histopathological report revealed ulcerated lining epithelium covered with necrotic and inflammatory exudates [Table/Fig-2]. The culture of the pus swab taken from the edge of ulcer showed significant growth of Gram negative bacilli Pseudomonas aeruginosa. Patient came back for follow up after four months. CT scan, Positron Emission Tomograhy-Computed Tomography (PET-CT), cytology of Cerebro Spinal Fluid (CSF) and biopsy was performed. Computed Tomography (CT) scan revealed non homogenously enhancing marked thickening of the right parapharyngeal wall commencing from above the level of fossa of Rosenmuller extending down up to level of vallecula [Table/Fig-3]. Similar thickening is also seen involving posterior pharyngeal wall in oropharynx extending up to the level of piriform sinuses and left lateral pharyngeal wall in oropharynx. There was also involvement of right border epiglottis with overall narrowing of pharyngeal cavity. PET–CT revealed well enhancing high FDG (Fluorin 18 Fluorodeoxyglucose) avid soft tissue mass of approximate size 43 mm x 32 mm in right tonsillar region with the involvement of soft palate. Enlarged lymph nodes were seen alongwith the greater vessels of neck at bilateral level II, III and IV. Bone marrow biopsy did not reveal any malignancy. A repeat biopsy revealed infiltration by a mixture of small, medium and large size lymphoid cells along with tissue necrosis [Table/Fig-4]. Thus based on the clinical picture and histopathology a presumptive diagnosis of LMG was made. Immunohistochemistry analysis carried out with specific markers (CD2+immune markers) showed positive results. These markers are specific for NK/T cells, hence a final diagnosis of NK/T cell lymphoma was made. An obturator [Table/Fig-5,6] was fabricated by prosthodontist and the patient was referred back to the oncologist for combination treatment of radiotherapy and chemotherapy, but sadly, the patient died during the course of treatment.
Image showing palatal perforation at the junction of hard and soft palate on the right side.

Photomicrograph showing ulcerated lining epithelium with inflammatory exudates (H&E, 10X).
a) CT scan revealing thickening of right para pharyngeal wall (arrow).; b) PET-CT revealing well enhanced high FDG avid soft tissue mass in right tonsillar region with soft palate involvement.
Photomicrograph showing small, medium and large sized lymphocytes cells along with tissue necrosis. (H&E, 45X).
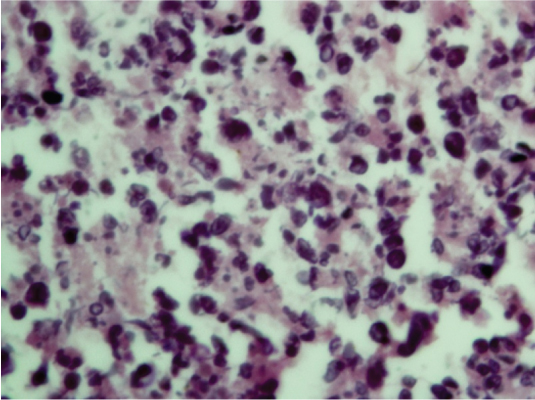
Image showing fabricated obturator over the patient’s maxillary cast.

Image showing try-in of the obturator in patient’s mouth. (Images left to right)

Discussion
LMG was first described by McBride P. It is an idiopathic ulcerating process involving the nose and the oral cavity, leading to severe tissue destruction of the central face [1]. The term “Lethal midline granuloma” or “Granuloma gangrencscenes” were used for this condition because the disease usually showed an aggressive and lethal course [2]. According to literature, the majority of lethal midline granulomas are nasal NK/T cell lymphomas [3], and they are very aggressive, locally destructive, midfacial necrotizing lesions. Many of these were diagnosed as LMG initially, a term that is slowly being replaced. Main challenge in diagnosing these conditions is because of non specific symptoms the patient presents with, which also delays the management. Multidrug chemotherapy followed by radiotherapy appears to be the most effective treatment approach in most of the cases [4].
McBride P first described a case of rapid destruction of the face and nose in 1897 [1] since then a variety of terminologies have been used for the same. In 1922, Stewart’s reported 10 cases of a chronic midfacial destructive process, which became known as Stewart’s syndrome or Stewart’s Granuloma. In 1949, Williams popularized the term LMG to designate inflammatory midline destructive lesions with no known aetiologic factors. Later, it was found that many of the disease process included under this heading were neither lethal nor granulomatous. Thus, other non-specific descriptive terms came into being, such as non-healing midline granuloma, idiopathic midline granuloma, Stewart’s syndrome and Malignant Midline Granuloma (MMG), relatively heterogeneous group of disease processes [5]. This disorder has to be distinguished from other progressive ulcerative disorder of the midline facial tissues, including cocaine abuse, Sarcoidosis, tuberculosis, syphilis, septal carcinoma, Wegener’s Granulomatosis (WG), Polymorphoreticulosis (PMR) [6]. Grossly it appeared as a necrotic granuloma, the disease had an aggressive and lethal course, therefore the term “Lethal Midline Granuloma (LMG)” or “Granuloma Gangrenescens” were used. LMG is composed of three different types of histopathology, i.e., WG, malignant lymphoma and Polymorphic Reticulosis (PR) or Midline Malignant Reticulosis (MMR) [7]. In 1933, Stewart divided the symptoms of LMG into three stages - prodromal, active and terminal [8].
In current case the patient had a perforation of palate and CT-scan and PET-CT showed involvement of naso, oro and laryngopharynx. Facial skin was not involved. WG, PR, or MMR, and malignant lymphoma could be histologically differentiated from each other by taking clinical findings into account. In our patient histopathological findings showed ulcerated epithelium with infiltration of atypical cells with tissue necrosis. The disease was termed as nasal T-cell lymphoma because the proliferating cells showed a positive immunoreactivity for polyclonal antibodies against T cells [7]. However, monoclonal rearrangement of the T-cell receptor genes was hardly seen in cases with “Nasal T-cell lymphoma” [7]. Ng CS et al., showed that the tumour cells showed a positive immunoreactivity for NK cell marker CD56 [9]. There are evidences suggesting that PR is a neoplasm of activated NK cells [7,10,11]. The proliferating cells usually show CD2+, CD56+, CD3e+, CD7-, CD16-, cytotoxic granule associated proteins and do not exhibit rearrangement of T-cell receptor or immunoglobulin genes. Mature or peripheral NK/T cell lymphomas account for only 10-15% of non-Hodgkins lymhoma. Amongst them, the most common and well characterized ones are the ‘nasal’ and ‘nasal type’ NK/T cell lymphomas. They are currently referred to as angiocentric lymphomas in the Revised European American Lymphoma (REAL) classification or nasal NK/T cell lymphoma by World Health Organization–European Organization For Research and Treatment of Cancer (WHO-EORTC) classification [12]. Their characteristic histological feature is an angiocentric/angiodestructive growth pattern with zonal necrosis. Both nasal and nasal type NK/T cell lymphomas reflect specific characteristics of NK cells [13]. Zhong BN et al., reported that most upper aerodigestive tract NK/T cell lymphomas were genotypically of NK cell origin and a few belonged to T cell lineage [14]. Although the upper respiratory tract, especially nasal region, is the common site of presentation. NK/T-cell lymphoma of nasal type may present in diverse extra nodal sites such as gastrointestinal tract, skin, testis, liver, and spleen. In our patient immunohistochemistry shows CD2+ve. NK/T cell marker CD56 was unavailable, but based on clinical picture and histopathology, we came to a diagnosis of NK/T cell lymphoma. Accordingly the patient was referred for chemotherapy and radiotherapy.
Conclusion
Nasal NK/T cell lymphoma usually follows an aggressive and lethal course especially in Asians. Death is common and is mostly due to relapse or systemic spread in 50% of cases. Thus, we need to be aware of the uncommon presentation of these lymphomas and keep it as a differential diagnosis for early diagnosis and management of patients.
[1]. McBride P, Photographs of a case of rapid destruction of the nose and faceJ Laryngol Otol 1897 :64-66. [Google Scholar]
[2]. Katsuyuki A, Mona AA, Epidemiology and pathogenesis of Nasal NK/T – cell Lymphoma: A Mini ReviewThe Scientific World Journal 2011 11:422-28. [Google Scholar]
[3]. Mendenhall WM, Olivier KR, Lynch JW, Mendenhall NP, Lethal Midline Granuloma – Nasal Natural Killer/T-Cell LymphomaAm J Clin Oncol 2006 29:202-06. [Google Scholar]
[4]. Vandana MC, Balachandran Bhat S, Geetha V, Donald F, Nasal NK/T cell Lymphoma presenting as a lethal midline granulomaIndian J Dermatol Venerol Leprol 2008 74(2):145-47. [Google Scholar]
[5]. Alexandra B, James F, Pablo V, Roy E, Robert L, Midline destructive lesions of the sinonasal tract: simplified terminology based on histopathologic criteriaAm J Neuroradiol 2000 21:331-36. [Google Scholar]
[6]. Robert P, Remco L, Paul V, Ben S, Johannes L, Re-irradiation of a second localization of idiopathic midline destructive diseses in the head and neck areaEur Arch otorhinolaryngol 2007 264:1521-23. [Google Scholar]
[7]. Katsuyuki A, Tetsuya T, Tadashi H, Woo-Ick Y, Nasal NK/T cell Lymphoma: epidemiology and pathogenesisInt J Hematol 2008 87:110-17. [Google Scholar]
[8]. Stewart JP, Progressive Lethal Granulomatous Ulceration of the NoseJ Laryng & Otol 1933 48:657-701. [Google Scholar]
[9]. Ng CS, Chan JKC, Lo S, Expression of natural killer cell markers in Non-Hodgkin’s LymphomasHum Pathol 1987 18:1257-62. [Google Scholar]
[10]. Ohsawa M, Nakatsuka S, Kanno H, Miwa H, Kojya S, Harabuchi Y, Immunophenotypic and Genotypic charecterization of nasal lymphoma with polymorphic reticulosis morphologyInt J Cancer 1999 81:865-70. [Google Scholar]
[11]. Jaffe ES, Harris NL, Stein H, Vardiman JW, Pathology and Genetics of tumors of hemopoietic and lymphoid tissues 2001 Lyon, FranceIARC Press [Google Scholar]
[12]. Jaffe ES, Classification of natural killer (NK) cell and NK like T cell malignanciesBlood 1996 87:1207-10. [Google Scholar]
[13]. Kato N, Yasukawa K, Onozuka T, Kikuta H, Nasal and nasal type T/NK cell Lymhoma with cutaneous cell involvementJ Am Acad Dermatol 1999 40:850-56. [Google Scholar]
[14]. Zhong BN, Zhang XH, Li M, Study of the pathology, immunophenotype, aetiology and genetic markers of NK/T cell lymphomaZhonghua Xue Ye Xue Za Zhi 2003 24:505-09. [Google Scholar]