Emergency Peripartum Hysterectomy: Indications and Outcome in a Tertiary Care Setting
Anshuja Singla1, Rajlaxmi Mundhra2, Latika Phogat3, Sumita Mehta4, Shalini Rajaram5
1 Assistant Professor, Department of Obstetrics & Gynaecology, UCMS & GTB Hospital, Delhi, India.
2 Ex-Senior Resident, Department of Obstetrics & Gynaecology, UCMS & GTB Hospital, Delhi, India.
3 Ex-Senior Resident, Department of Obstetrics & Gynaecology, UCMS & GTB Hospital, Delhi, India.
4 Specialist, Department of Obstetrics & Gynaecology, UCMS & GTB Hospital, Delhi, India.
5 Director Professor, Department of Obstetrics & Gynaecology, UCMS & GTB Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajlaxmi Mundhra, Ex-Senior Resident, Department of Obstetrics & Gynecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi-110095, India.
E-mail: Rmundhra54@yahoo.com
Introduction
Emergency Peripartum Hysterectomy (EPH) is an important lifesaving procedure, mostly reserved for conditions deemed to be serious and life threatening, and not amenable to conservative methods. In the present scenario, the advent of newer medical and conservative surgical methods for controlling obstetric haemorrhage has influenced the incidence, trend and the outcomes of the procedure.
Aim
To evaluate the demographic profile, indications, operative details, maternal morbidity and mortality and neonatal outcomes of women undergoing EPH.
Materials and Methods
A descriptive analysis of case records of women who underwent EPH between September 2006 to July 2014, at Guru Teg Bahadur Hospital Delhi, India was done. Data were collected from the medical records department.
Results
A total of 194 cases (n) were identified among 1,00712 deliveries, an incidence of 1.92 per 1000 deliveries. Majority of the women were unbooked i.e., they did not receive any form of antenatal care and were gravida 3 and above. The indications were atonic PPH in 89 (45.87%), rupture of unscarred uterus in 36 (18.56%), morbidly adhered placenta in 30 (15.46%), scar rupture in 20 (10.31%) and gangrenous uterus 19 (9.79%). The mean blood loss was around 1.6±0.45 litres. Approximately 14% cases underwent stepwise devascularisation prior to hysterectomy and in only 2% women, B-Lynch suture was applied. Thirteen (6.7%) cases had bladder injury and 22 (11.34%) needed re-laparotomy for hysterectomy. Around 76 (39%) women were shifted for ICU care. Nineteen (9.79%) women developed Disseminated Intravascular Coagulation (DIC). The case fatality rate was 7.2% and perinatal mortality was 30%.
Conclusion
Atonic PPH remains the leading cause of EPH in our analysis. Surprisingly rupture of unscarred uterus was more common compared to scar rupture. Creating awareness among women to seek health services in time with facilities for early referral, teaching younger obstetricians with conservative surgical procedures like stepwise devascularisation steps and compressive sutures should be of utmost priority.
Atonic PPH, Compressive sutures, Obstetric hysterectomy
Introduction
More than 100 years old, the first successful obstetric hysterectomy was carried out in 1876 by Eduardo Porro from Pavia, Italy for obstetric haemorrhage [1]. Since then, Emergency Peripartum Hysterectomy (EPH) is an important lifesaving procedure, reserved for conditions deemed to be crucial and life threatening and not amenable to conservative methods. In the present scenario, the advent of newer medical and conservative surgical procedures for controlling obstetric haemorrhage has helped in decreasing the incidence of EPH [2].
In modern era, with both vaginal and caesarean deliveries, the incidence is 0.4 to 2.5 per 1000 deliveries [3]. There remains a considerable variation in the incidence and aetiology of EPH between the developing and the developed world owing to the monstrous gap between the availability and the acceptability of the health care infrastructure. In the developed world, the ever increasing load of caesarean section with its attendant risks of abnormal placentation constitutes the commonest indication whereas unsupervised pregnancies with advanced obstetric complications remain the commonest in the developing countries. Despite many initiatives like the Millienium Development Goals [4], lack of antenatal care with unsupervised and unskilled birth attendants, illiteracy, poverty, poor transportation facilities, inadequate distribution of health services have contributed to delay in seeking health care service leading to a rise in the incidence of peripartum hysterectomy.
Despite being a lifesaving procedure, EPH is not without risks. It is known to be associated with uncontrolled bleeding, blood transfusion risks, infections, DIC, and increased maternal morbidity and mortality. Maternal mortality rates associated with EPH range from 0 to 30%, with the higher rates in regions with limited medical facilities [5,6].
Though, conservative measures to control obstetric bleeding should be attempted first, timely decision to resort to hysterectomy can be vital in saving maternal lives. With this background, this study was planned to evaluate the demographic profile, indications, operative details, maternal morbidity and mortality and neonatal outcomes in women undergoing EPH.
Materials and Methods
A retrospective audit of medical case records of women who underwent EPH at a tertiary care hospital in Delhi was done from September 2006 to July 2014. This hospital caters to a mixed population of urban, semirural and rural population in and around Delhi and Uttar Pradesh states of India.
Information was collected regarding age, parity, antenatal booking and literacy status, presenting complaints, indications of hysterectomy, operative details, maternal morbidity, mortality and neonatal outcomes.
Results
During the study period, there were a total of 100712 deliveries. 194 cases underwent EPH, an incidence of 1.92 per 1000 deliveries.
The mean age of patients was 29±2.2 years and majority were gravida 3 and above [Table/Fig-1]. Approximately 92% cases were unbooked i.e., women did not receive any form of antenatal care. Eighty-nine (45.8%) women were illiterate and 50 (25.7%) had education upto only primary level [Table/Fig-2]. There was an initial rise in the incidence of EPH but later, a drop was noted, though the incidence has largely remained the same over the years [Table/Fig-3].
| n(%) No. of cases |
|---|
| Age (years) | |
| <20 | 5 (2.5%) |
| 21-30 | 149 (76.8%) |
| 31-40 | 39 (20.10%) |
| >40 | 1 (0.5%) |
| Parity | |
| Primigravida | 12 (6.19%) |
| Second gravid | 40 (20.6%) |
| Third gravid & more | 142 (73.2%) |
Footnotes: n - No. of cases
Maternal and neonatal outcomes.
| n(%) |
|---|
| Booked | 16 (8.2%) |
| Un booked | 178 (91.8%) |
| Literacy status | |
| Illiterate | 89 (45.87%) |
| Primary | 50 (25.7%) |
| Secondary | 42 (21.6%) |
| Higher | 13 (6.7%) |
Footnotes: n - No. of cases

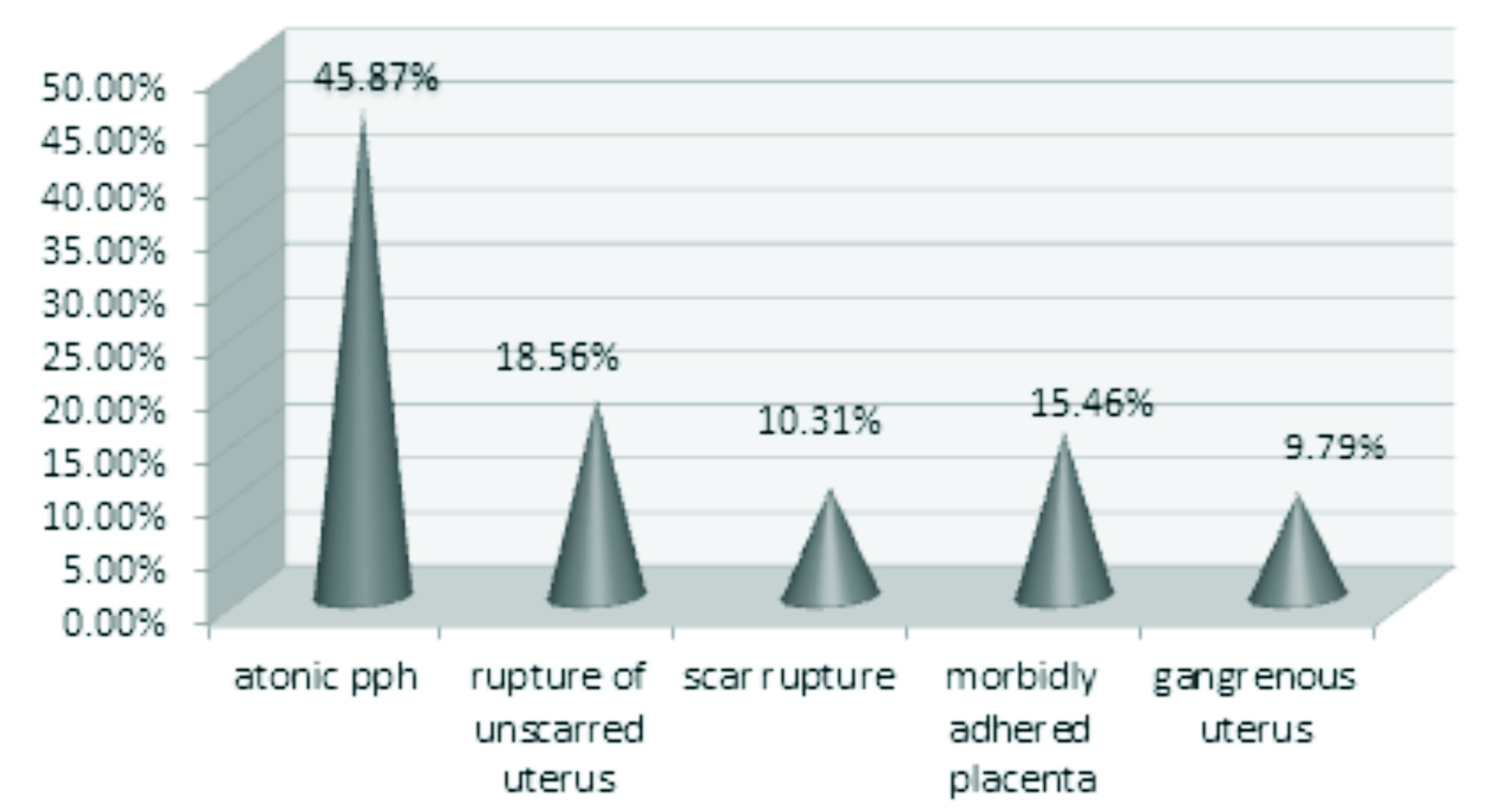
Atonic Postpartum Haemorrhage (PPH) was the leading cause of emergency peripartum hysterectomy accounting for 89 (45.87%) cases followed by rupture of unscarred uterus in 36 (18.56%) and morbidly adhered placenta in 30 (15.46%). Surprisingly, rupture of unscarred uterus (n=36, 18.5%) was more common than scar rupture (n=20, 10.31%). These were women in advanced obstructed labour who did not seek hospital care in time. Gangrenous uterus secondary to post abortal complications accounted for 19 (9.79%) cases [Table/Fig-4].
Indications of EPH.
Footnotes: PPH - Postpartum Haemorrhage
There was a mean blood loss of 1.6±0.45 litres. Step wise devascularisation was done in 14.43% cases and B-lynch suture was applied in only 2.06% cases prior to resorting to hysterectomy. [Table/Fig-5] depicts maternal complications and [Table/Fig-6] shows neonatal outcomes. Of the 102 (58.28%) live born babies, 23 (22.4%) required NICU care and 59 (30.43%) babies died of various complications. All 14 maternal deaths were due to disseminated intravascular coagulation and multiorgan failure.
| n(%) |
|---|
| Bladder injuries | 13 (6.7%) |
| ICU care | 76 (39.17%) |
| DIC | 19 (9.79%) |
| Relaparotomy | 22 (11.34%) |
| Maternal Deaths | 14 (7.2%) |
| Wound infection | 8 (15.52%) |
Footnotes: ICU - Intensive Care Unit; DIC - Disseminated Intravascular Coagulation; n - no. of cases
| n(%) |
|---|
| Live born | 102 (58.28%) |
| Still births | 73 (41.7%) |
| NICU care | 23 (22.4%) |
| Perinatal mortality | 59 (30.43%) |
Footnotes: NICU - Neonatal Intensive Care Unit; n - No of cases
Discussion
The present study is only a descriptive study of the causes and complications of EPH. Undoubtedly, emergency peripartum hysterectomy still remains a necessary technique for managing intractable obstetric haemorrhage. When to resort to this drastic step, has always been an obstetrician’s dilemma especially in a primigravida. Often a number of conservative approaches are undertaken before sacrificing her reproductive potential. Skill and assessment of one’s own capability in undertaking such a major surgery should be prompt and immediate referral to a higher facility is the key as every second matters.
With advancement in the medical management of PPH, there is a changing trend noticed in the incidence of EPH. The incidence of 1.92/1000 deliveries in our audit was less than that reported by D’Arpe S et al., (2.2/1000), Singh N et al., (2.08% in caesarean hysterectomy and 0.54% following vaginal delivery) and by Khan B et al., (10.52/1000) [7–9].
A total of 178 (92%) women undergoing EPH were unbooked and 89 (45.87%) were illiterate. Illiteracy and ignorance has been a major roadblock in usage of health care facilities and availing antenatal care. Such women are an easy prey to unskilled birth attendants and its risks. A 74.2% of the women were multigravidas (gravida 3 and above), indicating that high parity is a risk factor for obstetric hysterectomy.
There was an initial rise in the incidence of obstetric hysterectomy followed by a decrease and then a plateau probably owing to better management and availability of a number of conservative modalities.
Postpartum Haemorrhage (PPH) was the most common indication accounting for 45.87% cases, similar to that reported by Sohasrabhojanee N et al., (50%) [10]. Second most common indication was rupture of unscarred uterus in 18.56% cases. A 15.46% had morbidly adherent placenta as compared to 26% and 27.45% in studies by Praneshwari Deci et al., and Singh and Nagrath respectively [11,12].
Incidence of bladder injury was similar to that of Anita and Kavita (6.7% vs 7.3%) [13]. Bladder injury was seen in 13 women in our study and was more common in women with morbidly adherent placenta (n=7), rupture uterus (n=4) and iatrogenic (n=2). Re-laprotomy for haemoperitoneum was done in 11.34% cases unlike 16.42%% cases in study by Yalinkaya et al., [14]. The case fatality rate was 7% in comparison to 10.9% by Baskett [15]. Perinatal mortality was 30.43% in contrast to 85.71% reported by Singh et al., [8]. [Table/Fig-7] lists the national and international studies reported in literature on EPH [5,6–9,15–22].
Comparison of incidence of EPH [5,7–9,15–21].
| Incidence of of EPH (%) |
|---|
| Sturdee & Rushton (1986) [5] | 0.7% |
| Ambiye & Venkatraman (1988) [16] | 0.12% |
| Radha et al (1991) [17] | 0.3% |
| Allahabadia & Vaidya (1991) [6] | 0.19% |
| Mantri et al (1993) [16] | 0.32% |
| Agashe & Marathe (1995) [19] | 0.56% |
| Whiteman et al (2006) [20] | 0.77% |
| Sakse et al (2997) [21] | 0.24% |
| Bodelon et al (2009) [22] | 0.56% |
| Khan et al (2012) [9] | 10.52% |
| Singh et al (2014) [8] | 2.08% |
| D’Arpe (2015) [7] | 2.2% |
| Present study | 1.92% |
The major limitation of the study of this study was its retrospective nature.
Conclusion
The rate of PPH has remained more or less the same over years. Atonic PPH is still the leading cause and rupture of unscarred uterus due to obstructed labour is more common a cause of hysterectomy than scarred uterus. In spite of being a lifesaving procedure, a significant number of EPH can be prevented by creating community awareness about the necessity of seeking early and regular antenatal care in addition to immediate and urgent referral as and when required.
Footnotes: n - No. of cases
Footnotes: n - No. of cases
Footnotes: ICU - Intensive Care Unit; DIC - Disseminated Intravascular Coagulation; n - no. of cases
Footnotes: NICU - Neonatal Intensive Care Unit; n - No of cases
[1]. Todman D, Eduardo Porro (1842-1902) and the development of caesarean section: a reappraisalInternet Scientific Publications [Internet][cited 2016 Apr 2]. Available from: http://ispub.com/IJGO/7/2/11772 [Google Scholar]
[2]. Omole-Ohonsi A, Olayinka HT, Emergency peripartum hysterectomy in a developing countryJ Obstet Gynaecol Can 2012 34(10):954-60. [Google Scholar]
[3]. Cunningham FG, Leveno KJ, Bloom SL, Amniotic fluid. In: Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM, Sheffield JS, edsWilliams Obstetrics 2014 24th edNew York, NYMcGraw-Hillchap 11 [Google Scholar]
[4]. Millennium Project. Goals, targets and indicators. Available from: http://www.unmillenniumproject.org/goals/gti.htm. Accessed on 6th October 2015 [Google Scholar]
[5]. Sturdee DW, Rushton DI, Cesarean and postpartum-hysterectomy 1968-1983Br J Obstet Gynaecol 1986 93:270-74. [Google Scholar]
[6]. Allahabadia G, Vaidya P, Obstetric hysterectomy (A review of 50 cases from January 1987 to August 1990)J Obstet Gynecol India 1991 41:634-37. [Google Scholar]
[7]. D’Arpe S, Franceschetti S, Corosu R, Palaia I, Di Donato V, Perniola G, Emergency peripartum hysterectomy in a tertiary teaching hospital: a 14-year reviewArch Gynecol Obstet 2015 291(4):841-47. [Google Scholar]
[8]. Singh N, Pandey K, Gupta R, Agarwal S, Choudhary A, Obstetric hysterectomy, still a life saving tool in modern day obstetrics: a five year studyInt J Reprod Contracept Obstet Gynecol 2014 3(3):540-43. [Google Scholar]
[9]. Khan B, Khan B, Sultana R, Bashir R, Deeba F, A ten year review of emergency peripartum hysterectomy in a tertiary care hospitalJ Ayub Med Coll Abbottabad 2012 24(1):14-7. [Google Scholar]
[10]. Sohasrabhojanee M, Jindal M, Kamat A, Obstetric hysterectomy a life saving emergencyJ. Obstet Gynecol India 2006 58:138-41. [Google Scholar]
[11]. Praneshwari Devi RK, Singh NN, Singh D, Emergency obstetric hysterectomyJ Obstet Gynecol India 2004 54:127-29. [Google Scholar]
[12]. Singh R, Nagrath A, Emergency Obstetric hysterectomy- A retrospective study of 51 cases over a period of 5 yearsJ Obstet Gynecol India 2005 55:428-30. [Google Scholar]
[13]. Anita K, Kavita W, Emergency Obstetric hysterectomyJ Obstet Gynaecol India 2005 55:132-34. [Google Scholar]
[14]. Yalinkaya A, Güzel AI, Kangal K, Emergency peripartum hysterectomy: 16-year experience of a medical hospitalJ Chin Med Assoc 2010 73(7):360-63. [Google Scholar]
[15]. Baskett TF, Emergency obstetric hysterectomyJ Obstet Gynaecol 2003 23(4):353-55. [Google Scholar]
[16]. Ambiye VR, Venkataraman V, Kudchadkar DB, Hysterectomy in obstetricsJ Obstet Gynecol Ind 1988 38:318-21. [Google Scholar]
[17]. Radha T, Prabhu B, Radha B, Obstetric hysterectomyJ Obstet Gynecol Ind 1991 41:342-45. [Google Scholar]
[18]. Mantri L, Maheshwari K, Kiran C, Emergency hysterectomy. A 10 years reviewJ Obstet Gynecol Ind 993 43:936-39. [Google Scholar]
[19]. Agashe AP, Marathe SS, Obstetric hysterectomy (A review of 50 cases from January 1987 to August 1990)J Obstet Gynecol Ind 1991 45:490-93. [Google Scholar]
[20]. Whiteman MK, Kuklina E, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, Incidence and determinants of peripartum hysterectomyObstet Gynecol 2006 108(6):1486-92. [Google Scholar]
[21]. Sakse A, Weber T, Nickelsen C, Secher NJ, Peripartum hysterectomy in Denmark 1995-2004Acta Obstet Gynecol Scand 2007 86:1472-75. [Google Scholar]
[22]. Bodelon C, Bernabe-Ortiz A, Schiff MA, Reed SD, Factors associated with peripartum hysterectomyObstet Gynecol 2009 114(1):115-23. [Google Scholar]