Vitamin D deficiency has reached an epidemic in India with prevalence rate being 70-100% in the general population [1]. Vitamin D deficiency is widely prevalent in tropical countries like India despite abundant sunlight [1]. It is the most under diagnosed and untreated nutritional deficiency in the world. Vitamin D deficiency is associated with increased risk of vascular disease and ischemic stroke in healthy individuals [2,3]. Vitamin D deficiency is associated with ischemic stroke risk and contributing factors being hypertension, hyperlipidemia, diabetes mellitus and ischemic heart disease [4]. Stroke is the second leading cause of death worldwide, accounting for 9% of deaths. There are an estimated 5.7 million stroke deaths which are expected to increase to 7.8 million by 2030 [5,6]. Vitamin D deficiency in stroke patients preceded stroke and prevalence of vitamin D deficiency was more in stroke patients than general medical patients [7]. Vitamin D supplementation in post stroke patients is helpful in prevention of recurrent stroke and is suggested to reduce neurological, psychological and musculoskeletal disorders [8]. It also reduces morbidity, mortality and improves functional outcome after stroke [9]. American Stroke Association International Stroke Conference 2015 has found that stroke patients with low vitamin D levels have large ischemic infarcts, suffer severe strokes and have poor health outcomes after stroke than those with normal vitamin D level [10].
There are various methods and scales to assess severity of stroke. SSS is reliable and widely used to assess functional outcome in patients with ischemic cerebrovascular disease and has been successfully used in several clinical trials [11].
Even though studies have shown association of vitamin D deficiency in stroke, studies have not been done by supplementation of vitamin D to ischemic stroke patients, which form the basis of our study. We tested the hypothesis that there is improved functional outcome in ischemic stroke patients supplemented with high dose of vitamin D compared with ischemic stroke patients receiving regular conventional treatment. Thus, we have assessed the long term outcome of ischemic stroke patients with low vitamin D level, by supplementation of vitamin D.
Materials and Methods
This is a non blinded, randomized controlled trial conducted at PSG Hospitals, Coimbatore, Tamil Nadu, India. On obtaining approval from Institutional Human Ethics committee, the study was conducted in ischemic stroke patients admitted in Neurology ward from April-2014 to March- 2016. Informed written consent was obtained from the patients.
At the time of planning for the study, there were no trials of vitamin D supplementation in ischemic stroke patients. Therefore, sample size was based on Mean±SD estimates of vitamin D level in ischemic stroke patients and normal persons as per advice by statistician and the study done by Wu C et al., was used for calculation of sample size [12]. Sample size was calculated by Open Epi software version 3.01, by using simplified formula for difference in means of power 80%, confidence interval 95% and α level of 0.05 and was found to be 28 persons in each group.
The study included both males and females of age group from 50 to 80 years with vitamin D insufficiency (Serum 25- hydroxy vitamin D level 21-29 ng/ml) and vitamin D deficiency (Serum 25- hydroxy vitamin D level ≤ 20 ng/ml). Diagnosis of stroke was based on clinical assessment supported by Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI). Ischemic stroke patients with Middle Cerebral Artery (MCA) ischemia as per Alberta Stroke Program Early CT Score (ASPECTS) were taken. ASPECTS is a 10-point quantitative topographic CT scan score and are simple and reliable [13]. ASPECTS of 10 score indicate no infarct and 9 indicates one area of infarct in MCA and so on. ASPECTS of 6-7 indicate moderate infarcts, which were taken for our study. Patients with haemorrhagic stroke, large MCA stem stroke, lacunar stroke, who were thrombolyzed, very poor general condition, multiple organ impairment and with normal vitamin D levels (Serum 25- hydroxy vitamin D level ≥ 30 ng/ml) were excluded from our study.
Vitamin D status was assessed by measuring serum 25- hydroxy vitamin D by electro chemiluminescence binding assay. Interpretation was made as per US Endocrine society [14] and patients with serum 25-hydroxy vitamin D ≤ 20 ng/ml were taken as vitamin D deficient, 21-29 ng/ml were taken as vitamin D insufficient and ≥ 30 ng/ml were taken as normal vitamin D level. Only patients with vitamin D deficiency and insufficiency were taken for study.
SSS is widely used to assess patients with ischemic cerebrovascular disease [15]. It includes two forms of scale, Acute prognostic scale has a range of 0-22 points and long term convalescent scale has a range of 0-48 points with higher scores being associated with good prognosis. Two scales test different components of neurological assessment for e.g., consciousness is rated in acute scale but not in long term, while orientation and language are not rated in acute scale but important part of follow up score. Low scores in SSS suggest more severe ischemic stroke. SSS has been used in several clinical trials to assess stroke outcome after treatment [11,16]. We used long term stroke scale in our study. It assesses arm motor power, hand motor power, leg motor power and orientation whose maximum point is 6 indicating no abnormality and minimum score is 0 indicating total loss of function. It also assesses speech with maximum points of 10, facial palsy with maximum points of 2 and gait with maximum points of 12. Thus, total score of 48 denotes no abnormality and 0 denotes total paralysis.
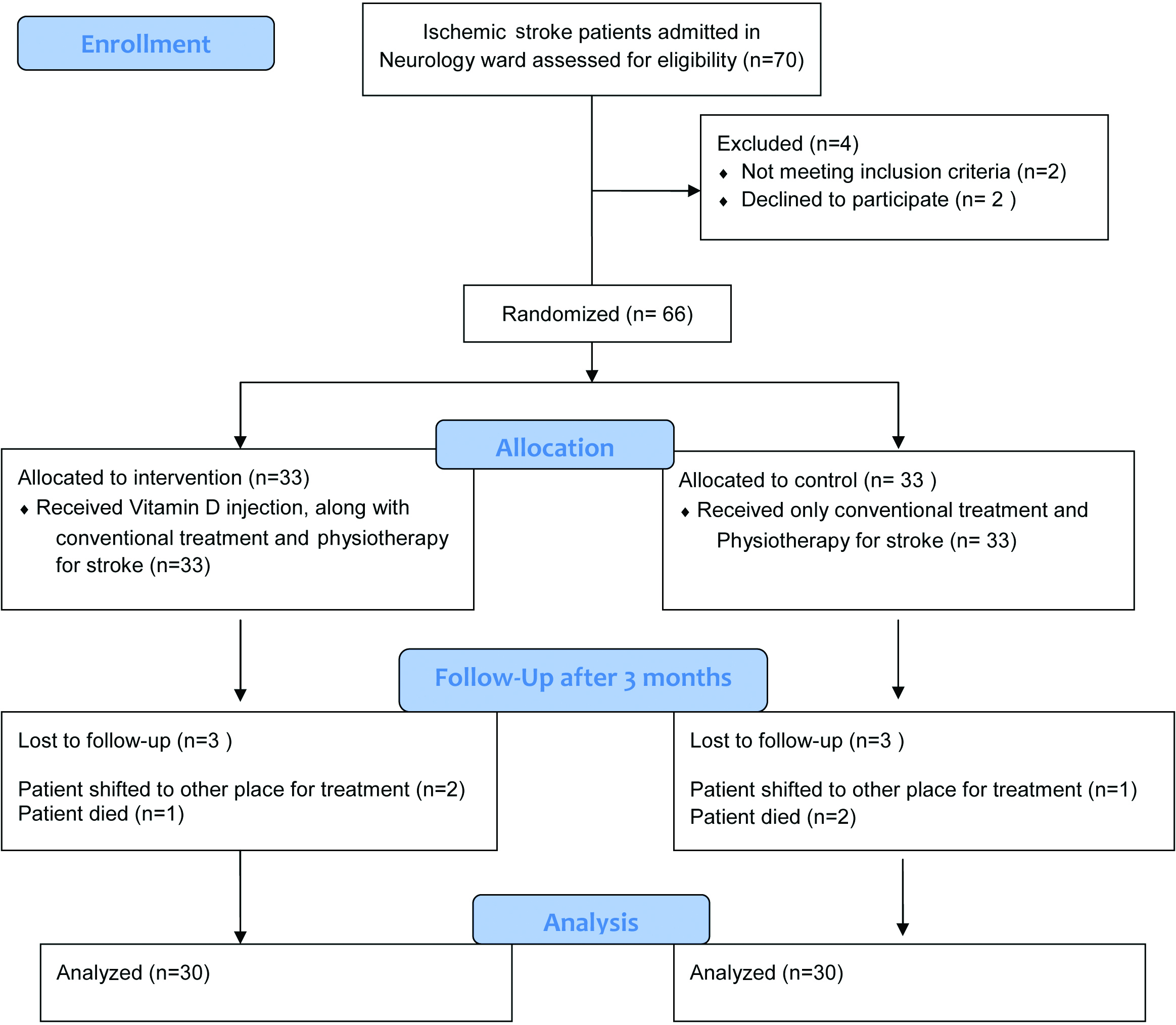
As the ischemic stroke patients got admitted in Neurology ward, every consecutive patient were assessed for inclusion and exclusion criteria and were randomized by simple randomization method where random numbers were computer generated using Microsoft Excel Spreadsheet Software. Seventy Ischemic stroke patients were assessed for the study, 66 were found to be eligible and were randomized and assigned to Group A or Group B of 33 in each group. SSS (long term) was applied for 66 patients at the time of admission to assess the severity of stroke. Group A were given 6 lac IU of cholecalciferol intramuscularly at time of admission. Group B were not given vitamin D. The regular medical treatment for ischemic stroke and physiotherapy were continued in both groups. At the end of three months, six patients lost follow up and finally 60 patients were analysed with 30 patients in each group as per [Table/Fig-1]. SSS was applied to 60 patients at end of three months to assess the outcome of vitamin D supplementation in ischemic stroke patients.
Flow chart of participants.
Compliance to oral therapy of vitamin D is a major limitation which is overcome by IM injection of vitamin D. We gave a single IM injection of 6 lac IU of cholecalciferol to Group A as high dose of vitamin D is found to be more effective and safe in increasing vitamin D levels and balance performance [17]. We measured the outcome after three months since the vitamin D reaches the maximum level and is found to be effective by three months period as per study by Telliglo A et al., [17]. We observed no side effects in patients supplemented with vitamin D, as they were patients with vitamin D deficiency.
Statistical Analysis
The difference in SSS between time of admission and after three months in Group A and Group B were analyzed statistically using SPSS software version 19.0 and independent t-test was used for the analysis.
Results
Among 30 ischemic stroke patients taken for study in Group A and Group B, median age was 62 and 65 respectively. In Group A there were 19 males (63.3%) and 11 females (36.7%) and in Group B there were 21 males (70%) and 9 females (30%). Mean±SD of vitamin D levels in Group A and Group B were 17.98±3.81ng/ml and 18.44±4.69 ng/ml respectively. Both the values fall in vitamin D deficiency range.
Based on vitamin D levels we divided each group into vitamin D deficiency (≤ 20 ng/ml) and vitamin D insufficiency (21-29 ng/ml). In Group A, there were 20 patients (66.7%) with vitamin D deficiency and 10 patients (33.3%) with vitamin D insufficiency. In Group B, there were 19 patients (63.3%) with vitamin D deficiency and 11 patients (36.7%) with vitamin D insufficiency. Most patients fall in vitamin D deficiency range.
Mean±SD of vitamin D levels in patients with vitamin D deficiency and vitamin D insufficiency in Group A and Group B is shown in [Table/Fig-2]. There is not much difference in mean values of vitamin D in deficiency and insufficiency in Groups in A and B.
Mean±SD of vitamin D levels in patients with vitamin D deficiency and vitamin D insufficiency in Group A and Group B.
| Group | Mean±SD of vitamin D (ng/ml) in vitamin D deficiency patients | Mean±SD of vitamin D (ng/ml) in vitamin D insufficiency patients |
|---|
| A | 15.59±1.48 | 23.04±1.36 |
| B | 14.92±1.38 | 24.13±1.11 |
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment; Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
Mean±SD of SSS at time of admission and after three months in Group A was 32.50±11.61 and 38.89±8.34 respectively. Mean±SD of SSS at time of admission and after three months in Group B was 35.82±8.56 and 38.32±7.10 respectively as shown in [Table/Fig-3].
Mean SSS at time of admission and after three months in Group A and Group B.
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment; Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
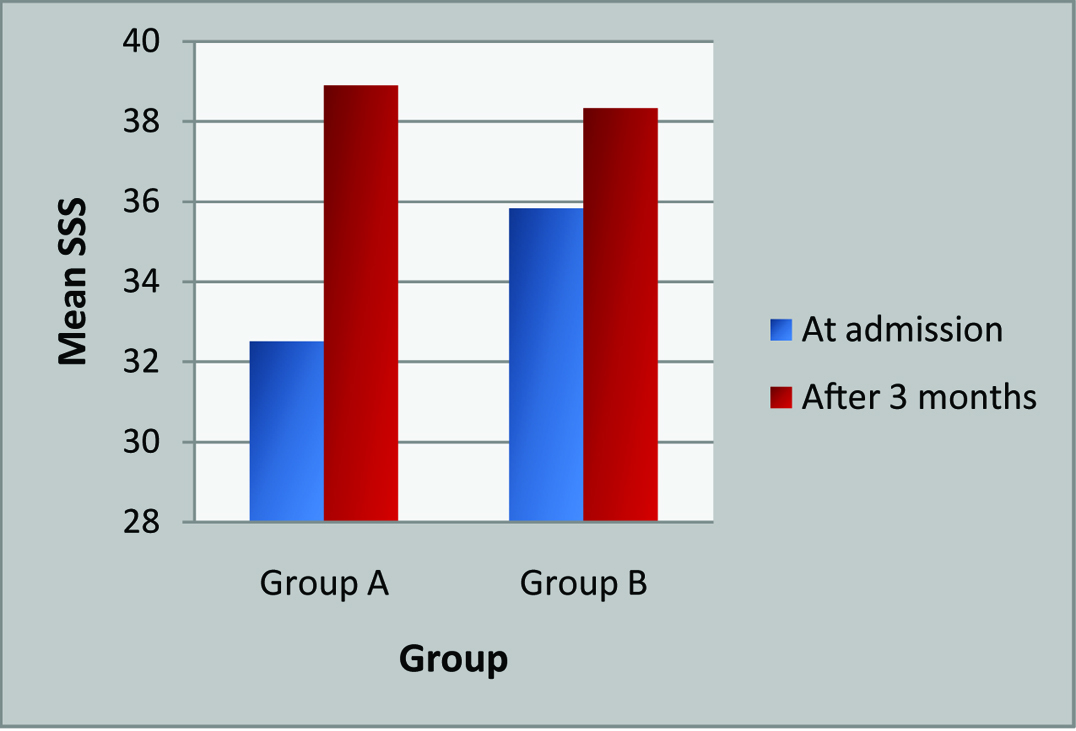
The mean SSS at time of admission in Group A was 32.50 which improved to 38.89 after vitamin D injection and regular treatment for stroke i.e., improved by 6.39 points, while in Group B the mean SSS at time of admission was 35.82 which improved to 38.32 by only regular treatment for stroke i.e., improved by 2.50 points. We took the difference in SSS between time of admission and after three months to denote the outcome of stroke. The outcome is better when the difference is more (mean±SD is 6.39±4.56) as seen in Group A, who were supplemented with vitamin D. The outcome is worse when the difference is less (mean±SD is 2.50±2.20) as seen in Group B, who were not supplemented with vitamin D. This difference in SSS at time of admission and after three months in Group A and Group B were analyzed statistically using independent t-test and found to be highly significant as p-value<0.001 as in [Table/Fig-4].
Comparison of differences in SSS at time of admission and after 3 months between Group A and Group B.
| Group | N | Difference in SSS mean±SD | p-value (T) |
|---|
| A | 30 | 6.39±4.56 | < 0.001** |
| B | 30 | 2.50±2.20 |
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment, Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
N= Number of patients, SSS – Scandinavian Stroke Scale, p<0.05-significant, p <0.001** – Highly significant, T – independent t-test.
The difference in SSS between vitamin D deficiency patients in Group A and Group B was statistically significant as p-value< 0.001. The difference in SSS between vitamin D insufficiency patients in Group A and Group B was not statistically significant as p=0.182. Even though Group A showed more difference in SSS than Group B in both deficiency and insufficiency group, it was found to be statistically significant only in vitamin D deficiency group (p<0.001), suggesting that vitamin D supplementation produces better outcome in ischemic stroke patients with vitamin D deficiency than vitamin D insufficiency as in [Table/Fig-5].
Comparison of differences in SSS between:
i) Vitamin D deficiency patients in Group A and Group B;
ii) Vitamin D insufficiency patients in Group A and Group B.
| Vitamin D | Group | N | Difference in SSSMean±SD | p-value (T) |
|---|
| Deficiency | A | 20 | 6.84±4.45 | < 0.001** |
| B | 19 | 2.06±2.48 |
| Insufficiency | A | 10 | 5.18±4.44 | 0.182 NS |
| B | 11 | 3.00±1.65 |
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment, Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
N= Number of patients, SSS – Scandinavian Stroke Scale, p<0.05-significant, p <0.001** – Highly significant, NS = Not significant, T – independent t-test.
Discussion
Vitamin D deficiency is very common in India and studies have shown the association of vitamin D deficiency with cardiovascular, renal diseases, cancer, autoimmune, neurological and infectious diseases [18–21]. Vitamin D deficiency is associated with increased prevalence of diabetes, hypertension, hyperlipidemia and stroke [22]. Turetsky A et al., did a study in 96 stroke patients and found that patients with low vitamin D level had two times larger areas of infarct when compared with normal vitamin D levels. For each 10 ng/ml decrease in vitamin D level, stroke recovery after three months decreased by half [10].
Pilz S et al., found low vitamin D levels are independent risk factor for fatal stroke in patients referred for coronary angiography and suggested that vitamin D might protect against stroke as studies have shown that vitamin D also protects hypertension, diabetes mellitus and atherosclerosis [23]. Autier P et al., did a meta-analysis on life threatening diseases like cancer, cardiovascular disease, diabetes etc., and found a significant decrease of total mortality in patients who received vitamin D [24].
Studies have shown the association of vitamin D with ischemic stroke [3,4,7,10], but ours might be the first one to study the outcome of ischemic stroke in vitamin D deficiency patients on supplementation with vitamin D. Chaudhuri J et al., found independent association of vitamin D deficiency with ischemic stroke in large artery atherosclerosis and cardio embolic stroke [25]. In our study total 65% had vitamin D deficiency and 35% had vitamin D insufficiency as our study group included only patients with low vitamin D level.
Park KY et al., found baseline vitamin D levels in patients with good outcomes were significantly higher than those with poor outcome (20 vs.17 ng/ml). The functional outcome after three month was better in highest quartile group (vitamin D 35 ng/ml) than lowest quartile group (8 ng/ml). The average vitamin D status was only 19 ng/ml, 69% had vitamin D < 20 ng/ml while 14% had > 30 ng/ml [9]. In our study all subjects had vitamin D < 30 ng/ml and mean vitamin D level in Group A (vitamin D supplemented) was 17.98 ng/ml and Group B (Vitamin D not supplemented) was 18.44 ng/ml, which falls in deficiency range.
The scales available for assessment of stroke include SSS, Barthel index, Rankin scale and Sickness impact profile. SSS has been used in many stroke studies to measure neurological function. It is reliable and has been validated in predicting mortality and functional outcome [15]. We assessed the severity of ischemic stroke patients at time of admission and after three months of vitamin D supplementation by SSS.
Study done by Edwards DF et al., analyzed validity, sensitivity and specificity of SSS and neurological scale for MCA infarction in stroke patients with varied aetiology and their results supported the use of both tests in trials of ischemia and haemorrhagic strokes. They found the admission score of SSS to be 33.7±15.4 and haemorrhagic stroke 31.13±14.6 [26]. Mean±SD of SSS on admission in Group A and Group B were 32.50±11.61 and 35.82±8.56 respectively while Mean±SD of SSS after 3 months in Group A and Group B were 38.89±8.34 and 38.32±7.10 respectively in our study.
Matthews LR administered 50,000-100,000 IU vitamin D immediately after admission and continued to supplement with vitamin D for up to five days and reported significant improvement in functional outcome in three months, fewer deaths and fewer disabilities [27]. Park KY et al., found that giving 50,000 IU/day, for first few days after stroke is safe and improves the outcome [9].
We assessed the outcome of stroke after giving a single injection of cholecalciferol of 6 lac IU intramuscularly at time of admission. This has not been studied in ischemic stroke patients but its effect has been studied in hypovitaminoses D. Einarsdottir K et al., found single IM cholecalciferol injection (6 lac IU) as an adjunct to oral supplementation is a safe and effective method to increase and maintain vitamin D levels after biliopancreatic divergent surgery [28]. Single injection of 6 lac IU of cholecalciferol raised vitamin D level from 2 ng/ml to 22 ng/ml in two weeks and to 27 ng/ml in six weeks in elderly people. Single injection is safe and recommended for elderly in autumn to prevent winter time vitamin D deficiency [29].
We assessed the severity of stroke by SSS, at the time of admission and after three months in both groups. Both groups showed increase in mean SSS after three months (Group A from 32.5 to 38 89, Group B from 35.82 to 38.32) showing improvement, patient is considered to have better outcome when difference in scores is more (Group A vs Group B was 6.39 vs 2.20) which was statistically significant (p<0.001). SSS has been used to assess the severity of stroke but no similar study has been done to assess the outcome of stroke after vitamin D supplementation.
Contrast to our study, Ford JA et al., in his study found that vitamin D supplementation does not protect against heart attack or stroke and found it is helpful only in old heart failure patients [30]. Pilz S et al., recommended to supplement vitamin D in stroke patients and to maintain it at 30 ng/ml to increase the survival rate [23].
Relevant risk factor for stroke associated with vitamin D deficiency is hypertension attributable to compensatory secondary hyperparathyroidism [31]. Proposed mechanism by which vitamin D improves cardiovascular disease are negative regulation of renin angiotensin system, effects on glycemic control, direct effects on vasculature and regulation of Parathormone (PTH) levels [32–34]. The Northern Manhattan study showed low vitamin D was significantly associated with increased intimal media thickness and carotid plaques in cardio embolic stroke [35]. Vitamin D deficiency caused a dysregulation in inflammatory response and reduces neuroprotective factors like Insulin Growth Factor-1(IGF-1) [36]. Vitamin D might promote neuroplastic changes that may in turn improve clinical recovery. Since vitamin D can cross blood brain barrier and Vitamin D Receptors (VDR) are identified in brain, it also exerts antithrombotic and neuroprotective actions [37,38]. Prabhakar P et al., found that genetic variants in VDR gene was associated with an increased risk for stroke in vitamin D deficient persons [39].
Our study can be considered unique as trials involving functional outcome of ischemic stroke after vitamin D replenishment in low vitamin D patients have not been studied.
Limitation
The limitations of our study are small sample size, confounding factors affecting the stroke were not considered and the results cannot be generalized. Vitamin D level was not measured at the time of assessing the outcome of stroke after three months.
Conclusion
Vitamin D is a potential risk factor for stroke and vitamin D supplementation has better outcome in ischemic stroke patients with vitamin D deficiency. Single dose replacement of vitamin D has significantly improved the outcome of ischemic stroke. Screening for vitamin D status is essential in ischemic stroke patients and supplementation to be done to maintain vitamin D at normal level.
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment; Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment, Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
N= Number of patients, SSS – Scandinavian Stroke Scale, p<0.05-significant, p <0.001** – Highly significant, T – independent t-test.
Group A: Ischemic stroke patients supplemented with vitamin D along with conventional treatment, Group B: Ischemic stroke patients not supplemented with vitamin D, receiving only conventional treatment.
N= Number of patients, SSS – Scandinavian Stroke Scale, p<0.05-significant, p <0.001** – Highly significant, NS = Not significant, T – independent t-test.