Immediate Outcome of Balloon Mitral Valvuloplasty with JOMIVA Balloon during Pregnancy
Shanmuga Sundaram Rathakrisnnan1, Ramona Ramasamy2, Tamilarasu Kaliappan3, Rajendiran Gopalan4, Ramasmy Palanimuthu5, Premkrishna Anandhan6
1 Associate Professor, Department of Cardiology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
2 Resident, Department of Cardiology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
3 Associate Professor, Department of Cardiology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
4 Professor, Department of Cardiology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
5 Associate Professor, Department of Cardiology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
6 Assistant Professor, Department of Cardiology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shanmuga Sundaram Rathakrisnnan, Department of Cardiology, PSG Institute of Medical Sciences and Research, Peelamedu-641004, Coimbatore, Tamil Nadu, India.
E-mail: medishan2002@yahoo.co.in
Introduction
Rheumatic mitral stenosis is the most common Valvular Heart Disease encountered during pregnancy. Balloon Mitral Valvuloplasty (BMV) is one of the treatment option available if the symptoms are refractory to the medical management and the valve anatomy is suitable for balloon dilatation. BMV with Inoue balloon is the most common technique being followed worldwide. Over the wire BMV is a modified technique using Joseph Mitral Valvuloplasty (JOMIVA) balloon catheter which is being followed in certain centres.
Aim
To assess the immediate post procedure outcome of over the wire BMV with JOMIVA balloon.
Materials and Methods
Clinical and echocardiographic parameters of pregnant women with significant mitral stenosis who underwent elective BMV with JOMIVA balloon in our institute from 2005 to 2015 were analysed retrospectively. Severity of breathlessness (New York Heart Association Functional Class), and duration of pregnancy was included in the analysis. Pre procedural echocardiographic parameters which included severity of mitral stenosis and Wilkin’s scoring were analysed. Clinical, haemodynamic and echocardiographic outcomes immediately after the procedure were analysed.
Results
Among the patients who underwent BMV in our Institute 38 were pregnant women. Twenty four patients (63%) were in New York Heart Association (NYHA) Class III. All of them were in sinus rhythm except two (5%) who had atrial fibrillation. Thirty four patients (89.5%) were in second trimester of pregnancy at the time of presentation and four (10.5%) were in third trimester. Echocardiographic analysis of the mitral valve showed that the mean Wilkin’s score was 7.3. Mean mitral valve area pre procedure was 0.8 cm2. Mean gradient across the valve was 18 mmHg. Ten patients (26.5%) had mild mitral regurgitation and none had more than mild mitral regurgitation. Thirty six patients had pulmonary hypertension as assessed by tricuspid regurgitation jet velocity. All of them underwent BMV with JOMIVA balloon. Post procedure mean mitral valve area was 1.7 cm2 as assessed by echocardiography. Post procedure mean gradient across the mitral valve as assessed by echocardiography was 5 mmHg. Two patients had moderate to severe mitral regurgitation after the procedure and the rest had either no mitral regurgitation or mild mitral regurgitation after the procedure. None of the patients warranted mitral valve replacement after BMV. No patients had any manifestations of systemic embolism like cerebrovascular accident or limb ischemia after the procedure. None of the patients had preterm delivery or adverse fetal outcome during index hospitalisation.
Conclusion
Over the wire BMV is safe and effective method during pregnancy. The results are comparable to that of Inoue technique. BMV offers a good symptomatic improvement in pregnant women presenting with symptoms of pulmonary congestion because of Rheumatic mitral stenosis.
Mitral valve, Stenosis, Valvular heart disease
Introduction
Rheumatic mitral stenosis is the most common acquired Valvular Heart Disease encountered during pregnancy [1,2]. Moderate or severe mitral stenosis during pregnancy poses a challenge to the clinician since it can increase maternal as well as fetal morbidity and mortality [1,2]. The rate of fetal growth restriction and preterm birth rises with the severity of mitral stemosis from 14% in pregnant patients with mild mitral stemosis, to 28% and 33% in pregnant patients with moderate and severe mitral stemosis [3–5]. Heart failure occurs frequently in pregnant women with moderate or severe mitral stenosis (area <15.cms2) during second or third trimester [3–5]. Closed or open mitral valvotomy during pregnancy is associated with significant maternal and fetal morbidity and mortality [6–8]. BMV is the preferred treatment in pregnant women presenting with severe mitral stenosis if the symptoms are not controlled with medications and the valve anatomy is suitable [8–11]. Safety and efficacy of BMV during pregnancy is proven [9–11]. BMV is commonly done with Inoue balloon [12]. Over the wire BMV is a modified technique using JOMIVA balloon catheter and is being followed in certain centres [13,14]. There are studies assessing the short term and long term outcomes of BMV using JOMIVA balloon [13,14]. There are no studies assessing the safety and efficacy of over the wire BMV during pregnancy. In this study we have assessed the immediate post procedure outcome of over the wire BMV during pregnancy.
Materials and Methods
Clinical and echocardiographic parameters of pregnant women with significant mitral stenosis who underwent elective BMV with JOMIVA balloon in PSG Institute of Medical Sciences and Research, Tamil Nadu, India between 2005 to 2015 were analysed retrospectively. Patients who underwent emergency BMV and patients who were on mechanical ventilation were excluded. Severity of breathlessness (New York Heart Association Functional Class), duration of pregnancy were included in the analysis. Pre procedural echocardiographic parameters were analysed which included severity of the mitral stenosis as assessed by 2 dimensional mitral valve area, morphological analysis of the valve and Wilkin’s scoring (valvular calcification, thickness, mobility and subvalvular disease) [15]. Clinical (New York Heart Association Functional Class) and echocardiographic outcome which included 2 dimensional mitral valve area, pressure gradient across the mitral valve area and severity of mitral regurgitation after the procedure were analysed. Severity of pre procedural mitral regurgitation was noted. Mitral regurgitation was graded as mild, moderate and severe when the jet area occupies less than 20%, 20-40% and more than 40% of left atrium respectively. Width of vena contracta was also used to classify the severity of mitral stenosis, when it is less than 0.3 cm, 0.3-0.7 cm, more than or equal to 0.7 cm classifies mitral regurgitation as mild, moderate and severe respectively [16].
Procedure
Femoral arterial and venous access were taken. Atrial septal puncture was done with Brockenbrough technique [17]. A Mullin sheath and dilator was tracked inside the left atrium. Subsequently a Swan Ganz catheter was taken inside the left atrium through the Mullin sheath [18]. Mitral valve was crossed with the Swan Ganz catheter. A support wire was taken across the mitral valve through the Swan Ganz catheter. An appropriate sized JOMIVA balloon catheter was taken across the mitral valve over the support wire and the valve was dilated.
Statistical Analysis
Data was analysed using the statistical package for the social sciences (WINDOW VERSION 12.0; SPSS). Continuous variables were presented as mean and standard deviation. Categorical variables were expressed as percentages.
Results
Among the patients who underwent BMV in our Institute between 2005 and 2015, 38 were pregnant women. All 38 patients were included in the analysis. All patients underwent BMV with JOMIVA balloon. Baseline clinical and echocardiographic parameters are shown in [Table/Fig-1]. Mean age at the time of the procedure was 25 years. Twenty four patients (63%) were in NYHA Class III at the time of presentation in spite of medications. Ten patients (26.5%) were in NYHA class II and four (10.5%) were in NYHA class IV. Among the patients who underwent BMV all of them were in sinus rhythm except two (5%) who had atrial fibrillation at the time of the procedure. Thirty four patients (89.5%) were in second trimester of pregnancy at the time of presentation and 4 (10.5%) were in third trimester.
Baseline clinical and echocardiographic characteristics of pregnant women who underwent Balloon Mitral Valvuloplasty with JOMIVA balloon.
| Age (mean) | 25±6yrs |
| New York Heart Association Functional Class |
| II | 10 (26.5%) |
| III | 24 (63%) |
| IV | 4 (10.5%) |
| Sinus Rhythm | 36 (95%) |
| Atrial Fibrillation | 2 (5%) |
| Duration of pregnancy |
| Second trimester | 34 (89.5%) |
| Third trimester | 4 (10.5%) |
| Echocardiographic parameters |
| Wilkin’s score (mean) | 7.3 |
| Thickness (mean) | 2.1 |
| Mobility (mean) | 2.1 |
| Calcification (mean) | 1.6 |
| Sub valvular apparatus (mean) | 1.5 |
| Mitral valve area (mean) | 0.82±0.3cm2 |
| Mitral stenosis gradient (mean) | 18 mmHg |
| Pre-existing mitral regurgitation (MR) |
| No MR | 28 (73.5%) |
| Mild MR | 10 (26.5%) |
| Pulmonary hypertension | 36 (94.7%) |
Baseline echocardiographic parameters of the patients are shown in [Table/Fig-1]. Echocardiographic analysis of the mitral valve showed that the mean Wilkin’s score was 7.3. None of the patients had left atrial cavity or appendage thrombus. Mean mitral valve area pre procedure was 0.8 cm2. Mean gradient across the valve was 18 mmHg. Twenty eight patients (73.5%) did not have mitral regurgitation at the time of presentation. Ten patients (26.5%) had mild mitral regurgitation and none had more than mild mitral regurgitation. Thirty six patients (94.7%) had pulmonary hypertension as assessed by tricuspid regurgitation jet velocity.
All of them underwent BMV with JOMIVA. Pre and post procedure echocardiographic and catheterisation haemodynamic parameters are shown in [Table/Fig-2]. Mean mitral valve area as assessed by echocardiography after the procedure was 1.7 cm2. Mean gradient across the mitral valve after the procedure as assessed by echocardiography was 5 mmHg.
Echocardiographic and catheterisation haemodynamic parameters pre and post procedure.
| Echocardiographic Parameters | Pre Procedure | Post Procedure |
|---|
| Mitral Valve Area | 0.8±0.3 cm2 | 1.7±0.4 cm2 |
| Moderate to severe mitral regurgitation | Nil | 2 |
| Mitral stenosis gradient (Mean) | 18±8 mmHg | 5±2 mmHg |
| Catheterisation Parameters | | |
| Left Atrial mean | 26±7 mmHg | 9±2 mmHg |
| Mitral stenosis gradient (mean) | 16±4 mmHg | 4±3 mmHg |
| Pulmonary arterial Systolic pressure (mean) | 50±12 mmHg | 36±10 mmHg |
Procedure related complications are shown in [Table/Fig-3]. Only two patients had moderate to severe mitral regurgitation after the procedure and the rest had either no mitral regurgitation or mild mitral regurgitation after the procedure. Symptomatic improvement was noted in all of the patients except two. Requirement of medications like diuretics reduced after the procedure in all of the patients except those two. Two patients had persistent breathlessness after the procedure which could be managed medically with diuretics. None of the patient warranted mitral valve replacement after BMV. No patients had any manifestations of systemic embolism like cerebrovascular accident or limb ischemia. None of the patients had preterm delivery or adverse fetal outcome during index hospitalisation. One patient had minor groin hematoma at the access site which was managed with mechanical compression.
Showing the list of complications of Balloon Mirtal Valvuloplasty in pregnant women.
| Post procedure Complications | Number of Patients |
|---|
| Significant worsening of mitral regurgitation | 2 |
| Embolic complications | Nil |
| Pericardial effusion | Nil |
| Requirement of emergency Mitral valve replacement | Nil |
| Access site complications | 1 |
| Fetal complications during index hospitalisations | Nil |
Discussion
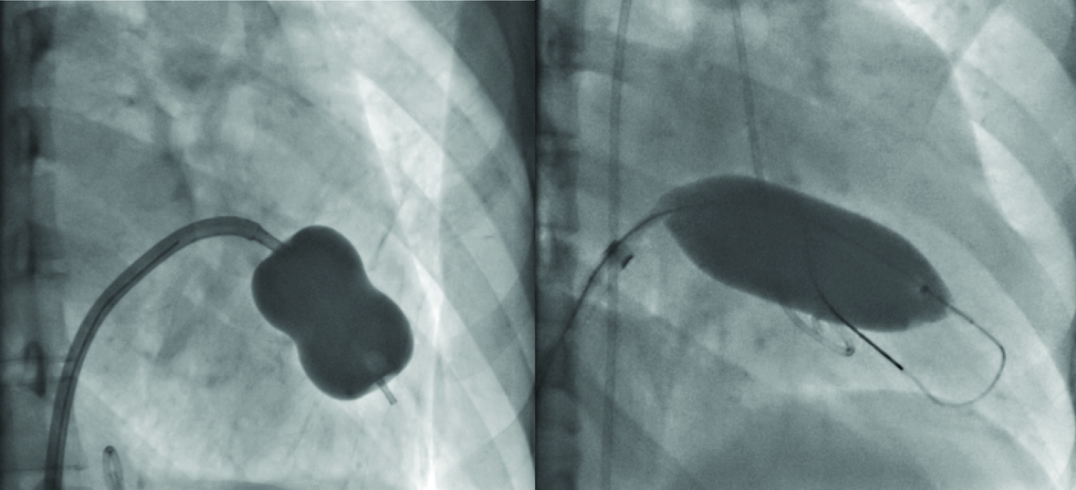
Pregnant women with haemodynamically significant mitral stenosis and significant breathlessness have an estimated mortality rate of 5 to 15% [6]. Closed mitral valvotomy has a mortality rate of less than 2%, fetal mortality of 1.2 to 8% and a miscarriage rate of 5 to 15% [7]. Open valvulotomy has a fetal mortality rate of 37.9% [8]. In view of high morbidity and mortality associated with the open surgical procedures, BMV has become the preferred treatment modality in pregnant women presenting with haemodynamically significant mitral stenosis with valve anatomy suitable for balloon dilatation [8]. Over the wire BMV with JOMIVA balloon was shown to be a cost-effective alternative to the widely followed Inoue technique [13,14]. JOMIVA balloon catheter is different from Inoue balloon in a way that it is a cylindrical balloon and not a dumbbell shaped balloon [Table/Fig-4].
Images showing Inoue balloon (left) with a central waist when inflated and JOMIVA balloon (right) which is cylindrical when inflated.
Baseline characteristics of pregnant women who presented with significant mitral stenosis shows that most of the patients were in sinus rhythm except two who were in atrial fibrillation. Low prevalence of atrial fibrillation in pregnant women presenting with mitral stenosis in our study is similar to other studies where a similar data was noted [10]. This could be explained by the age of these patients at presentation. Pre-existing mitral regurgitation was documented in 10 patients. The valve morphology as assessed by Wilkin’s scoring shows that mean score was 7.3 which indicate that most of the patients had a low risk valve for complications during balloon dilatation.
Procedural success as defined by a reduction in mitral valve gradient less than 50% of the pre BMV gradient, valve area more than or equal to 1.5 cm2 and no significant increase in mitral regurgitation was noted in 90% of the patients. This was similar to the results obtained with Inoue balloon where the procedure success was documented in 90-95% of the patients [8].
Moderate to severe mitral regurgitation as assessed by echocardiography was documented in two (5%) patients in our study. This is similar to the data published earlier with Inoue balloon where significant increase in mitral regurgitation was documented in 4% of the patients [8]. No patient warranted emergency or elective mitral valve replacement in our study. Long term efficacy of BMV during pregnancy, safety in terms of long term effect of radiation during fetal life is also proven [11].
Limitation
Number of patients included in this study was less; it may not represent the entire set of patients who undergo BMV with JOMIVA balloon during pregnancy.
Conclusion
Over the wire BMV with JOMIVA balloon is safe and effective method of BMV during pregnancy. The results with JOMIVA balloon are comparable to that of Inoue technique. Incidence of post procedure mitral regurgitation after BMV with JOMIVA balloon is comparable with Inoue technique. Pregnant women presenting with symptoms of pulmonary congestion refractory to the medical management has good symptomatic improvement with BMV.
[1]. Elkayam U, Bitar F, Valvular heart disease and pregnancy part I: Native valvesJ Am Coll Cardiol 2005 46:223-30. [Google Scholar]
[2]. Stout KK, Otto CM, Pregnancy in women with valvular heart diseaseHeart 2007 93:552-58. [Google Scholar]
[3]. Lesniak-Sobelga A, Tracz W, KostKiewicz M, Podolec P, Pasowicz M, Clinical and echocardiographic assessment of pregnant women with valvular heart diseases—Maternal and fetal outcomeInt J Cardiol 2004 94:15-23. [Google Scholar]
[4]. Silversides CK, Colman JM, Sermer M, Siu SC, Cardiac risk in pregnant women with rheumatic mitral stenosisAm J Cardiol 2003 91:1382-85. [Google Scholar]
[5]. Hameed A, Karaalp IS, Tummala PP, Wani OR, Canetti M, Akhter MW, The effect of valvular heart disease on maternal and fetal outcome of pregnancyJ Am Coll Cardiol 2001 37:893-99. [Google Scholar]
[6]. Sullivan HJ, Valvular heart surgery during pregnancySurg Clin North Am 1995 75:59-75. [Google Scholar]
[7]. Pavankumar P, Venugopal P, Kaul U, Iyer KS, Das B, Sampathkumar A, Closed mitral valvulotomy during pregnancy, a 20 years experienceScandJ Cardiovasc Surg 1988 22:11-15. [Google Scholar]
[8]. de Souza JA, Martinez EE Jr, Ambrose JA, Alves CM, Born D, Buffolo E, Percutaneous balloon mitral valvuloplasty in comparison with open mitral valve commissurotomy for mitral stenosis during pregnancyJ Am Coll Cardiol 2001 37(3):900-03. [Google Scholar]
[9]. Salehi R, Aslanabadi N, Taghavi S, Pourafkari L, Imani S, Goldust M, Percutaneous balloon mitral valvotomy during pregnancyPak J Biol Sci 2013 16(4):198-200. [Google Scholar]
[10]. Salomé N, Dias CC, Ribeiro J, Gonçalves M, Fonseca C, Ribeiro VG, Balloon mitral valvuloplasty during pregnancy- Our experienceRev Port Cardiol 2002 21(12):1437-44. [Google Scholar]
[11]. Gulraze A, Kurdi W, Niaz FA, Fawzy ME, Mitral balloon valvuloplasty during pregnancy: The long term up to 17 years obstetric outcome and childhood developmentPak J Med Sci 2014 30(1):86-90. [Google Scholar]
[12]. Palacios IF, Sanchez PL, Harrel LC, Weyman AE, Block PC, Which patients benefit from percutaneous mitral balloon valvuloplasty? Prevalvuloplasty and postvalvuloplasty variables that predict long-term outcomeCirculation 2002 105:1465-71. [Google Scholar]
[13]. Routray SN, Mishra TK, Patnaik UK, Behera M, Percutaneous transatrial mitral commissurotomy by modified technique using a JOMIVA balloon catheter: A cost-effective alternative to the Inoue balloonJ Heart Valve Dis 2004 13(3):430-38. [Google Scholar]
[14]. Joseph G, Chandy S, George P, George O, John B, Pati P, Evaluation of a simplified transseptal mitral valvuloplasty technique using over-the-wire single balloons and complementary femoral and jugular venous approaches in 1,407 consecutive patientsJ Invasive Cardiol 2005 17(3):132-38. [Google Scholar]
[15]. Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios IF, Percutaneous balloon dilatation of mitral valve. An analysis of echocardiographic variables related to outcome and the mechanism of dilatationBritish Heart Journal 1988 60:299-308. [Google Scholar]
[16]. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiographyJ Am Soc Echocardiogr 2003 16(7):777-802. [Google Scholar]
[17]. Brockenbrough EC, Braunwald E, Ross J Jr, Transseptal left heart catheterization. A review of 450 studies and description of an improved technicCirculation 1962 25:15-21. [Google Scholar]
[18]. Mullins CE, Transseptal left heart catheterization: Experience with a new technique in 520 pediatric and adult patientsPediatr Cardiol 1983 4:239-45. [Google Scholar]